The originating document has been archived. We cannot confirm the completeness, accuracy, or currency of the content.
Liotrix
Drug class: Thyroid Agents
ATC class: H03AA02
VA class: HS851
CAS number: 8065-29-0
Introduction
Synthetic thyroid agent; combination preparation containing tetraiodothyronine (levothyroxine, T4) sodium and triiodothyronine (liothyronine, T3) sodium.
Uses for Liotrix
Hypothyroidism
Replacement or supplemental therapy in congenital or acquired hypothyroidism of any etiology, except transient hypothyroidism during the recovery phase of subacute thyroiditis. Specific indications include primary (thyroidal), secondary (pituitary), and tertiary (hypothalamic) hypothyroidism.
Not considered drug of choice for replacement therapy because offers no therapeutic advantage over levothyroxine sodium and may result in excessive serum T3 concentrations. Levothyroxine is considered drug of choice for replacement therapy.
For treatment of congenital hypothyroidism (cretinism), levothyroxine is considered drug of choice.
Pituitary TSH Suppression
Treatment or prevention of various types of euthyroid goiters, including thyroid nodules, subacute or chronic lymphocytic thyroiditis (Hashimoto’s thyroiditis), multinodular goiter, and in the management of thyroid cancer.
Diagnosis of Thyroid Disorders
Used diagnostically in suppression tests to differentiate suspected mild hyperthyroidism or thyroid gland autonomy. Use with caution in patients in whom there is a strong suspicion of thyroid gland autonomy because exogenous hormone effects will be additive to endogenous source.
Thyrotoxicosis
Has been used in combination with antithyroid agents for the treatment of thyrotoxicosis to prevent goitrogenesis and hypothyroidism.
Liotrix Dosage and Administration
General
-
Initially, monitor response to therapy about every 6–8 weeks. Once normalization of thyroid function and serum TSH concentrations has been achieved, patients may be evaluated less frequently (i.e., every 6–12 months). However, if dosage is changed, measure serum TSH concentrations after 8–12 weeks.
-
Natural and synthetic thyroid agent preparations are not necessarily directly comparable; however, the following equivalencies have been suggested based on clinical response:
|
Thyroid Agent |
Approximate Equivalent Dosage |
|---|---|
|
Levothyroxine sodium |
100 mcg or less |
|
Liothyronine sodium |
25 mcg |
|
Liotrix (levothyroxine sodium/liothyronine sodium) |
50 mcg/12.5 mcg (Thyrolar) |
|
Thyroglobulin |
65 mg |
|
Thyroid |
60–65 mg (1 grain) |
Administration
Oral Administration
Administer orally, usually as a single daily dose before breakfast.
Dosage
Available as fixed-combination preparation containing levothyroxine sodium and liothyronine sodium; dosage expressed in terms of the salts of both drugs.
Current USP standards define liotrix as containing levothyroxine sodium and liothyronine sodium in a ratio of 4:1 by weight. Thus, Thyrolar-1 contains 50 mcg of levothyroxine sodium and 12.5 mcg of liothyronine sodium, which is approximately equivalent to 60 mg of thyroid. (See General under Dosage and Administration.)
Adjust dosage carefully according to clinical and laboratory response to treatment. Avoid undertreatment or overtreatment. (See Therapy Monitoring under Cautions.)
Initiate at a lower dosage level in geriatric patients, in patients with functional or ECG evidence of cardiovascular disease, and in patients with severe, long-standing hypothyroidism or other endocrinopathies.
Pediatric Patients
Hypothyroidism
Oral
Initiate therapy at full replacement dosages as soon as possible after diagnosis of congenital hypothyroidism to prevent deleterious effects on intellectual and physical growth and development. The following dosages have been recommended:
|
Age |
Daily T3/T4 Dosage |
|---|---|
|
0–6 months |
3.1/12.5–6.25/25 mcg |
|
6–12 months |
6.25/25–9.35/37.5 mcg |
|
1–5 years |
9.35/37.5–12.5/50 mcg |
|
6–12 years |
12.5/50–18.75/75 mcg |
|
>12 years |
>18.75/75 mcg |
When transient hypothyroidism is suspected, therapy may be temporarily discontinued when the child is >3 years of age to reassess the condition. (See Pediatric Use under Cautions.)
Adults
Hypothyroidism
Oral
Usual initial dosage is one tablet of Thyrolar-1/2 daily. Increase by one tablet of Thyrolar-1/4 at intervals of 2–3 weeks.
For management of long-standing myxedema, particularly when cardiovascular impairment is suspected, usual initial dosage is one tablet of Thyrolar-1/4 daily.
Usual maintenance dosage is one tablet of Thyrolar-1 to one tablet of Thyrolar-2 daily. Serum TSH and T4 concentrations usually return to normal after 2–3 weeks of therapy. Failure to respond adequately to one Thyrolar-3 tablet daily suggests presence of malabsorption or patient noncompliance.
Pituitary TSH Suppression
Thyroid Cancer
OralAdministration of dosages higher than those used for replacement therapy usually is required to suppress TSH to low or undetectable concentrations. Medullary carcinoma of the thyroid usually unresponsive to this therapy.
Special Populations
Patients with Cardiovascular Disease
Hypothyroidism
Initiate therapy at lower dosages than those recommended for patients without cardiovascular disease.
Usual initial dosage is one Thyrolar-1/4 tablet or one Thyrolar -1/2 tablet daily. If angina appears or if cardiovascular disease is aggravated, reduce dosage or temporarily withhold therapy and then cautiously restart therapy at a lower dosage.
Geriatric Patients
Hypothyroidism
Initiate therapy at lower dosages than those recommended for younger patients.
Usual initial dosage is one Thyrolar-1/4 tablet or one Thyrolar -1/2 tablet daily. If cardiovascular disease is aggravated, reduce dosage or temporarily withhold therapy and then cautiously restart therapy at a lower dosage.
Cautions for Liotrix
Contraindications
-
Untreated thyrotoxicosis.
-
AMI uncomplicated by hypothyroidism.
-
Uncorrected adrenal insufficiency.
-
Known hypersensitivity to any ingredient in the formulation. (See Sensitivity Reactions under Cautions.)
Warnings/Precautions
Warnings
Unlabeled Uses
Should not be used for the treatment of obesity or for weight loss either alone or with other therapeutic agents. In euthyroid patients, doses within the range of daily hormonal requirements are ineffective for weight reduction. Larger doses may produce serious or life-threatening toxicity, particularly when given in conjunction with sympathomimetic amines (e.g., anorectic agents).
Should not be used in the treatment of male or female infertility unless this condition is associated with hypothyroidism.
Sensitivity Reactions
Hypersensitivity to thyroid hormone is not known to occur. However, hypersensitivity reactions to inactive ingredients of thyroid hormone products have been reported and include urticaria, pruritus, rash, flushing, angioedema, abdominal pain, nausea, vomiting, diarrhea, fever, arthralgia, serum sickness, and wheezing.
Major Toxicities
Effects on Bone Mineral Density
Increased markers of bone turnover.
General Precautions
Therapy Monitoring
Thyroid agents have a narrow therapeutic index. Avoid undertreatment or overtreatment, which may result in adverse effects on growth and development in pediatric patients, cardiovascular function, bone metabolism, reproductive function, cognitive function, emotional state, GI function, and glucose and lipid metabolism.
Periodically perform appropriate laboratory tests (e.g., serum TSH, total or free T4, total T3) and clinical evaluations to monitor adequacy of therapy.
Preexisting Cardiovascular Disease
Use with extreme caution. (See Patients with Cardiovascular Disease under Dosage and Administration.) Patients with CHD should be monitored closely during surgical procedures due to increased risk of arrhythmias.
Associated Endocrine Disorders
Hypopituitarism, adrenal insufficiency, and other endocrine disorders such as diabetes mellitus and diabetes insipidus are characterized by signs and symptoms which may be diminished in severity or obscured by hypothyroidism. Thyroid agents may aggravate the intensity of previously obscured symptoms in patients with endocrine disorders, and appropriate adjustment of therapy for these concomitant disorders may be required.
In patients with secondary or tertiary hypothyroidism, consider possibility of additional hypothalamic/pituitary hormone deficiencies and treat if diagnosed.
Chronic autoimmune thyroiditis may occur in association with other autoimmune disorders (e.g., adrenal insufficiency, pernicious anemia, type 1 diabetes mellitus.)
Patients with concomitant adrenal insufficiency should be treated with replacement corticosteroids prior to initiation of thyroid agents. Failure to do so may precipitate an acute adrenal crisis due to increased metabolic clearance of corticosteroids when the thyroid agent is initiated.
Patients with diabetes mellitus may require increased dosages of antidiabetic agents when treated with thyroid agents.
Specific Populations
Pregnancy
Category A.
During pregnancy, serum free T4 levels may decrease and serum TSH levels increase to values outside the normal range. Elevations in serum TSH may occur at 4 weeks’ gestation; monitor TSH levels during each trimester (or every 6 weeks) and adjust liotrix dosage accordingly. Reduce dosage to pre-pregnancy level immediately after delivery, since postpartum TSH concentrations are similar to preconception levels; measure serum TSH concentrations 6–8 weeks postpartum.
Lactation
Although thyroid hormones are distributed minimally into human milk, exercise caution when administering to a nursing woman. However, adequate replacement dosages generally are needed to maintain normal lactation.
Pediatric Use
The goal of treatment in pediatric patients with hypothyroidism is to achieve and maintain normal intellectual and physical growth and development. Initiate therapy immediately upon diagnosis. Maintain therapy for life, unless transient hypothyroidism is suspected.
Neonates with suspected hypothyroidism should receive thyroid agent therapy pending results of confirmative tests. If a positive diagnosis cannot be made on the basis of laboratory findings but there is a strong clinical suspicion of congenital hypothyroidism, initiate replacement therapy to achieve euthyroidism until the child is 1–2 years of age. During the first 2 weeks of therapy, closely monitor infants for cardiac overload, arrhythmias, and aspiration resulting from avid suckling. Evaluate infant’s clinical response to therapy about 6 weeks after initiation of thyroid agent therapy and at least at 6 and 12 months of age and yearly thereafter.
When transient hypothyroidism is suspected, temporarily discontinue therapy for 2–8 weeks to reassess the condition when the child is >3 years of age. If the diagnosis of permanent hypothyroidism is confirmed, reinstitute full replacement therapy. However, if serum concentrations of free T4 and TSH are normal, discontinue thyroid agent therapy and monitor carefully; repeat thyroid function tests if manifestations of hypothyroidism develop.
In pediatric patients with transient severe hypothyroidism, reduce replacement dose by half for 30 days to reassess condition. If, after 30 days, serum TSH >20 mU/L, consider the hypothyroidism permanent and reinstitute full replacement therapy. However, if serum TSH has not increased, temporarily discontinue thyroid agent therapy for another 30 days, then repeat serum free T4 and TSH measurements. Reinstitute or discontinue replacement therapy based on laboratory findings.
Monitor patients closely to avoid undertreatment or overtreatment. Undertreatment may result in poor school performance (due to impaired concentration and slowed mentation) and reduced adult height. Overtreatment may result in craniosynostosis in infants and accelerate aging of bones, resulting in premature epiphyseal closure and compromised adult stature.
Treated children may manifest a period of catch-up growth, which may be adequate in some cases to achieve normal adult height. In children with severe or long-standing hypothyroidism, catch-up growth may not be adequate to achieve normal adult height.
Pseudotumor cerebri and slipped capital femoral epiphysis have been reported in children receiving thyroid agents.
Geriatric Use
Because of the increased risk of cardiovascular disease among geriatric patients, liotrix therapy should not be initiated at the full replacement dose. (See Geriatric Patients under Dosage and Administration.)
Common Adverse Effects
Adverse reactions result from overdosage and resemble manifestations of hyperthyroidism, including fatigue, weight loss, increased appetite, heat intolerance, fever, excessive sweating, headache, hyperactivity, nervousness, anxiety, irritability, emotional lability, insomnia, tremor, muscle weakness, palpitations, tachycardia, arrhythmias, increased heart rate and BP, heart failure, angina, AMI, cardiac arrest, diarrhea, vomiting, abdominal cramps, elevations in liver function test results, hair loss, flushing, decreased bone mineral density, menstrual irregularities, and impaired fertility.
Interactions for Liotrix
Drugs Affecting Hepatic Microsomal Enzymes
Potential increased metabolism of thyroid agent with drugs that induce hepatic microsomal enzymes resulting in increased thyroid agent dosage requirements.
Drugs That May Decrease T4 5’-Deiodinase Activity
Inhibitors of T4 5’ mono-deiodinase decrease peripheral conversion of T4 to T3, resulting in decreased T3 concentrations. However, serum T4 concentrations usually remain within normal range but may occasionally be slightly increased.
Specific Drugs and Foods
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Amiodarone |
Decreased metabolism of T4 to T3 |
|
|
Anticoagulants, oral (e.g., coumarins) |
Potentiation of anticoagulant activity |
Carefully monitor PT and adjust anticoagulant dosage accordingly when thyroid agent therapy is initiated |
|
Antidepressants (tricyclics, tetracyclics, SSRIs) |
Increased risk of cardiac arrhythmias and CNS stimulation when levothyroxine is used with tricyclics or tetracyclics Faster onset of action of tricyclics following concomitant use with levothyroxine Sertraline may increase levothyroxine requirements |
|
|
Antidiabetic agents (biguanides, meglitinides, sulfonylureas, thiazolidinediones, insulin) |
Thyroid agent may cause increased antidiabetic agent or insulin requirements |
Carefully monitor diabetic control, especially when thyroid therapy is initiated, changed, or discontinued |
|
β-Adrenergic blocking agents (e.g., propranolol hydrochloride dosages >160 mg daily) |
Decreased metabolism of T4 to T3 Impaired antihypertensive effects when hypothyroid patient is converted to euthyroid state |
|
|
Bile acid sequestrants (e.g., cholestyramine, colestipol) |
Impaired thyroid agent absorption |
Administer liotrix ≥4 hours apart from these agents |
|
Carbamazepine |
Potential increased metabolism of thyroid agent Reduced levothyroxine serum protein binding |
May require thyroid agent dosage increase |
|
Cardiac glycosides |
Decreased serum digitalis glycoside concentrations in patients with hyperthyroidism or in patients with hypothyroidism in whom a euthyroid state has been achieved; potential for reduced therapeutic effects of digitalis glycosides with thyroid agent use |
May need to increase dosage of digitalis glycoside when hypothyroidism has been corrected |
|
Corticosteroids (e.g., dexamethasone at dosages ≥4 mg daily) |
Decreased metabolism of T4 to T3 Short-term administration of large doses of corticosteroids may decrease serum T3 concentrations by 30% with minimal change in serum T4 concentrations |
|
|
Estrogen or estrogen-containing oral contraceptives |
Possible decreased free T4 concentrations |
Patients without a functioning thyroid gland may require liotrix dosage increase |
|
Ferrous sulfate |
Delayed or impaired thyroid absorption |
Administer liotrix ≥4 hours apart from this agent |
|
Food with large amounts of fiber (e.g., cotton seed meal, infant soybean formula, soybean flour, walnuts) |
Decreased levothyroxine absorption |
|
|
Furosemide (at IV dosages >80 mg) |
Concomitant use with levothyroxine produces transient increases in serum free T4 concentrations; continued administration results in a decrease in serum T4 and normal free T4 and TSH concentrations, and therefore, patients are clinically euthyroid |
|
|
GI drugs (e.g., antacids [aluminum hydroxide, magnesium hydroxide, calcium carbonate], simethicone, sucralfate) |
Delayed or impaired thyroid agent absorption |
Administer liotrix ≥4 hours apart from these agents |
|
Growth hormones (e.g., somatropin) |
Excessive use of thyroid agents with growth hormones may accelerate epiphyseal closure; however, untreated hypothyroidism may interfere with growth response to growth hormone |
|
|
Heparin |
Concomitant use with levothyroxine produces transient increases in serum free T4 concentrations; continued administration results in a decrease in serum T4 and normal free T4 and TSH concentrations, and therefore, patients are clinically euthyroid |
|
|
Hydantoins (e.g., phenytoin) |
Potential increased metabolism of thyroid agent Reduced levothyroxine serum protein binding Concomitant use with levothyroxine produces transient increases in serum free T4 concentrations; continued administration results in a decrease in serum T4 and normal free T4 and TSH concentrations, and therefore, patients are clinically euthyroid |
May require thyroid agent dosage increase |
|
Ketamine |
Risk of marked hypertension and tachycardia |
Use with caution |
|
NSAIAs (e.g., fenamates, phenylbutazone) |
Concomitant use with levothyroxine produces transient increases in serum free T4 concentrations; continued administration results in a decrease in serum T4 and normal free T4and TSH concentrations, and therefore, patients are clinically euthyroid |
|
|
Phenobarbital |
Potential increased metabolism of thyroid agent |
May require thyroid agent dosage increase |
|
Radiographic agents (iodine-containing) |
Reduced uptake of 123I, 131I, and 99mTc |
|
|
Rifampin |
Potential increased metabolism of thyroid agent |
May require thyroid agent dosage increase |
|
Salicylates (dosages >2 g daily) |
Concomitant use with levothyroxine produces transient increases in serum free T4 concentrations; continued administration results in a decrease in serum T4 and normal free T4and TSH concentrations, and therefore, patients are clinically euthyroid |
|
|
Sodium polystyrene sulfonate |
Delayed or impaired thyroid absorption |
Administer liotrix ≥4 hours apart from this agent |
|
Sympathomimetic agents |
Potentiation of sympathomimetic effects; increased risk of coronary insufficiency in patients with CAD |
Observe patient carefully when sympathomimetic agent is administered |
|
Xanthine derivatives (e.g., theophylline) |
Clearance of xanthine derivatives may be decreased in hypothyroid patients but returns to normal when the euthyroid state is achieved |
Drugs Affecting Thyroid Function or Thyroid Function Tests
Various drugs or concomitant medical conditions (e.g., pregnancy, infectious hepatitis) may adversely affect thyroid function (e.g., alter endogenous thyroid hormone secretion, reduce TSH secretion) resulting in hypothyroidism or hyperthyroidism or interfere with laboratory tests used to assess thyroid function. Consult specialized references for information.
Some drugs may affect transport of thyroid hormones (T3, T4) by affecting serum thyroxine-binding globulin (TBG) concentrations. However, free T4 concentrations may remain normal and the patient may remain euthyroid. Monitor therapy and adjust liotrix dosage as necessary.
Drugs Affecting Thyroxine Binding Globulin Concentrationsb j
- Drugs That May Increase Serum TBG Concentration
-
Estrogens, oral (including estrogen-containing oral contraceptives)
-
Fluorouracil
-
Methadone
-
Mitotane
-
Tamoxifen
- Drugs That May Decrease Serum TBG Concentration
-
Androgens
-
Asparaginase
-
Corticosteroids
-
Niacin (extended-release)
Liotrix Pharmacokinetics
Absorption
Bioavailability
Levothyroxine (T4): Variably absorbed from the GI tract (range: 40–80%). Extent of absorption is increased in the fasting state and decreased in malabsorption states.
Liothyronine (T3): Almost completely absorbed from the GI tract (about 95%).
Onset
Liothyronine has a more rapid onset of action than levothyroxine (24–72 hours versus 1–3 weeks).
Distribution
Extent
T4 is distributed throughout most body tissues and fluids; highest concentrations found in liver and kidneys.
Thyroid hormones do not readily cross the placenta; however, some transfer does occur, as evidenced by levels in cord blood of athyrotic fetuses being approximately one-third maternal levels.
Thyroid hormones are minimally distributed into breast milk.
Plasma Protein Binding
Circulating thyroid hormones are >99% bound to serum proteins, including TBG, thyroxine-binding prealbumin (TBPA), and albumin. T4 is more extensively and firmly bound to TBG and TBPA than T3. Only unbound hormone is metabolically active.
Elimination
Metabolism
T4 and T3 are metabolized principally in the liver through sequential deiodination. Approximately 80% of the daily dose of T4 is deiodinated to yield equal amounts of T3 and reverse T3 (rT3). T3 and rT3 are further deiodinated to diiodothyronine. Thyroid hormones are also metabolized via conjugation with glucuronides and sulfates and excreted directly into the bile and gut where they undergo enterohepatic recirculation.
Elimination Route
Thyroid hormones are primarily eliminated by the kidneys. A portion of the conjugated hormone reaches the colon unchanged and is eliminated in the feces. Approximately 20% of T4 is eliminated in stool. Urinary excretion of T4 decreases with age.
Half-life
T4: Approximately 6–7 days.
T3: Approximately 1–2 days.
These plasma half-lives are decreased in patients with hyperthyroidism and increased in those with hypothyroidism.
Stability
Storage
Oral
Tablets
Tight, light-resistant containers at 2–8°C.
Actions
-
Thyroid hormones (T4 and T3) regulate multiple metabolic processes, including augmentation of cellular respiration and thermogenesis, as well as metabolism of proteins, carbohydrates, and lipids.
-
Thyroid hormones also play an essential role in normal growth and development and normal maturation of the CNS and bone. The protein anabolic effects of thyroid hormones are essential for normal growth and development.
-
The physiologic actions of thyroid hormones are produced predominantly by T3, most of which (approximately 80%) is derived from T4 by deiodination in peripheral tissues.
-
T3 is approximately 4 times more potent than T4.
Advice to Patients
-
Importance of understanding the need to continue thyroid agent therapy for life, unless transient hypothyroidism is suspected.
-
Importance of taking thyroid agent exactly as prescribed. Do not alter regimen or discontinue therapy unless directed by a clinician.
-
Risk of transient hair loss. Importance of immediately informing a clinician if rapid or irregular heartbeat, chest pain, shortness of breath, leg cramps, headache, nervousness, irritability, sleeplessness, tremors, change in appetite, weight gain or loss, vomiting, diarrhea, excessive sweating, heat intolerance, fever, changes in menstrual periods, hives or skin rash, or any other unusual medical event occurs.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements, as well as any concomitant illnesses (e.g., cardiovascular disease, diabetes mellitus, clotting disorders, adrenal or pituitary gland problems).
-
In patients with diabetes mellitus, importance of monitoring blood and/or urinary glucose levels and immediately reporting any changes to a clinician. In patients receiving concomitant anticoagulant therapy, importance of monitoring clotting status frequently.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Dosage may need to be increased during pregnancy.
-
Importance of informing physician or dentist of current thyroid hormone therapy prior to any surgery.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
U.S. Pharmacopeia, an official public standards-setting authority for all prescription and over-the-counter medicines and other health care products manufactured or sold in the United States, has mandated new specifications for a component used in the manufacturing of Thyrolar. As a result, all strengths of Thyrolar are currently on long-term back order while Forest makes the modifications necessary to meet these new specifications. Forest is working diligently to complete these modifications. In the meantime, patients should speak with their physician regarding appropriate treatment for their condition, and check for future updates on the availability of Thyrolar through the Forest product availability toll-free hotline at (866) 927-3260.
Update: Actavis (formerly Forest) discontinued all Thyrolar presentations in September 2018.
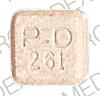
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
Levothyroxine Sodium 12.5 mcg and Liothyronine Sodium 3.1 mcg |
Thyrolar-¼ |
Forest |
|
Levothyroxine Sodium 25 mcg and Liothyronine Sodium 6.25 mcg |
Thyrolar-½ |
Forest |
||
|
Levothyroxine Sodium 50 mcg and Liothyronine Sodium 12.5 mcg |
Thyrolar-1 |
Forest |
||
|
Levothyroxine Sodium 100 mcg and Liothyronine Sodium 25 mcg |
Thyrolar-2 |
Forest |
||
|
Levothyroxine Sodium 150 mcg and Liothyronine Sodium 37.5 mcg |
Thyrolar-3 |
Forest |
AHFS DI Essentials™. © Copyright 2023, Selected Revisions March 27, 2019. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about liotrix
- Check interactions
- Compare alternatives
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: thyroid drugs
- Breastfeeding