Flibanserin (Monograph)
Brand name: Addyi
Drug class: Central Nervous System Agents, Miscellaneous
Chemical name: 1,3-Dihydro-1-[2-[4-[3-(trifluoromethyl)phenyl]-1-piperazinyl]ethyl]-2H-benzimidazol-2-one
Molecular formula: C20H21F3N4O
CAS number: 167933-07-5
Warning
- Hypotension and Syncope with Alcohol
-
Use of alcohol concomitantly or close together in time (i.e., within 2 hours) with flibanserin increases the risk of severe hypotension and syncope.
-
Patients should wait at least 2 hours before taking the dose of flibanserin if 1–2 standard alcoholic drinks were consumed or skip the dose of flibanserin if ≥3 standard alcoholic drinks were consumed during the evening. (See Hypotension and Syncope with Alcohol under Cautions.)
- Hypotension and Syncope with CYP3A4 Inhibitors
-
Concomitant use of flibanserin and moderate or potent CYP3A4 inhibitors is contraindicated because of substantially increased flibanserin exposure and risk of severe hypotension and syncope. (See Hypotension and Syncope with CYP3A4 Inhibitors under Cautions and also see Interactions.)
- Hypotension and Syncope in Patients with Hepatic Impairment
-
Flibanserin is contraindicated in patients with hepatic impairment because of substantially increased flibanserin exposure and risk of severe hypotension and syncope. (See Absorption: Special Populations, under Pharmacokinetics.)
Introduction
5-HT1A receptor agonist and 5-HT2A receptor antagonist.
Uses for Flibanserin
Hypoactive Sexual Desire Disorder (HSDD)
Used in premenopausal women for treatment of acquired, generalized HSDD, which is characterized by low sexual desire that causes marked distress or interpersonal difficulty and is not due to a coexisting medical or psychiatric condition, problems within the relationship, or the effects of medication or other drug substances.
HSDD may be categorized as acquired if the sexual dysfunction develops only after a period of normal functioning and as generalized if it is not limited to certain types of stimulation, situations, or partners.
Treatment of HSDD may include psychosocial (e.g., psychotherapy, including cognitive behavioral therapy, sex therapy, or couples therapy) and pharmacologic approaches (including bremelanotide and flibanserin).
In 3 randomized, controlled trials and an extension trial conducted in premenopausal women with HSDD, flibanserin was associated with an increased number of satisfying sexual events (SSEs), improved sexual desire, and decreased sexual distress.
Manufacturer states not indicated for treatment of HSDD in postmenopausal women† [off-label] or in men† [off-label].
Manufacturer also states not indicated to enhance sexual performance† [off-label].
Flibanserin Dosage and Administration
General
-
Allow at least 2 hours to elapse if 1–2 standard alcoholic drinks were consumed before taking flibanserin at bedtime. Do not take bedtime dose of flibanserin if ≥3 standard alcoholic drinks were consumed during the evening. After a dose of flibanserin is taken at bedtime, do not consume alcohol until the following day (i.e., at least until the next morning). (See Hypotension and Syncope with Alcohol under Cautions and also see Specific Drugs and Foods under Interactions.)
-
Allow at least 2 weeks to elapse between discontinuance of a moderate or potent CYP3A4 inhibitor and initiation of flibanserin and allow at least 2 days to elapse between discontinuance of flibanserin and initiation of a moderate or potent CYP3A4 inhibitor. (See Hypotension and Syncope with CYP3A4 Inhibitors under Cautions and also see Interactions.)
Administration
Oral Administration
Once daily at bedtime without regard to meals. Because taking flibanserin during waking hours increases the risk of hypotension, syncope, accidental injury, and CNS depression, do not administer at any other time of the day. (See CNS Depressant Effects under Cautions.)
Dosage
Adults
HSDD
Oral
100 mg once daily at bedtime.
Discontinue if HSDD symptoms are not improved after 8 weeks of therapy.
Special Populations
Hepatic Impairment
Contraindicated in patients with hepatic impairment. (See Hypotension and Syncope in Patients with Hepatic Impairment under Cautions.)
Renal Impairment
Manufacturer provides no specific dosage recommendations at this time. Dosage adjustments unlikely to be necessary because of only slight increases in exposure in patients with mild to severe renal impairment. (See Absorption: Special Populations, under Pharmacokinetics.)
Cautions for Flibanserin
Contraindications
-
Concurrent use of moderate or potent CYP3A4 inhibitors. (See Hypotension and Syncope with CYP3A4 Inhibitors under Cautions and also see Interactions.)
-
Hepatic impairment. (See Hypotension and Syncope in Patients with Hepatic Impairment under Cautions.)
Warnings/Precautions
Warnings
Hypotension and Syncope with Alcohol
Use of alcohol concomitantly or close together in time (i.e., within 2 hours) with flibanserin increases the risk of severe hypotension and syncope. Syncope requiring therapeutic intervention (e.g., ammonia salts and/or placement in supine or Trendelenburg position), hypotension, and somnolence occurred at a higher incidence when flibanserin was administered with alcohol during an alcohol interaction study.
Following consumption of 1–2 standard alcoholic drinks, allow at least 2 hours to elapse before administration of the flibanserin dose. If ≥3 standard alcoholic drinks were consumed during the evening, skip the bedtime flibanserin dose.
One standard alcoholic drink contains 14 grams of pure alcohol and is equivalent to:
-
A 12-ounce can of beer (5% alcohol content),
-
A 5-ounce glass of wine (12% alcohol content), or
-
1.5 ounces/shot of distilled spirit (40% alcohol content [80-proof]).
After a dose of flibanserin is administered at bedtime, do not consume alcohol until the following day. (See Specific Drugs and Foods under Interactions and also see Advice to Patients.)
Hypotension and Syncope with CYP3A4 Inhibitors
Moderate or potent CYP3A4 inhibitors substantially increase flibanserin exposure and the risk of hypotension and syncope; therefore, concomitant use of flibanserin and moderate or potent CYP3A4 inhibitors is contraindicated.
If treatment with a moderate or potent CYP3A4 inhibitor is required, discontinue flibanserin at least 2 days prior to initiation of therapy. If the benefit of initiating therapy with a moderate or potent CYP3A4 inhibitor within 2 days of flibanserin discontinuance clearly outweighs the risk of hypotension and syncope, monitor patient for signs of hypotension and syncope. Allow at least 2 weeks to elapse between discontinuance of the CYP3A4 inhibitor and reinitiation of flibanserin therapy.
Concomitant use of flibanserin with multiple weak CYP3A4 inhibitors, including dietary or herbal supplements (e.g., ginkgo, resveratrol) and OTC drugs (e.g., cimetidine), also may increase flibanserin exposure and lead to hypotension and syncope. (See Interactions.)
Hypotension and Syncope in Patients with Hepatic Impairment.
Use in patients with any degree of hepatic impairment substantially increases flibanserin concentrations, which can cause hypotension and syncope. Flibanserin is therefore contraindicated in patients with hepatic impairment. (See Absorption: Special Populations, under Pharmacokinetics.)
Other Warnings and Precautions
CNS Depressant Effects
Risk of somnolence and sedation when given alone; CNS depressant effects are most prominent approximately 1–4 hours after oral administration.
Risk of CNS depression is increased if flibanserin is taken during waking hours, with alcohol or other CNS depressants, or with drugs that increase flibanserin concentrations (e.g., CYP3A4 inhibitors). (See Dosage and Administration, Interactions, and Advice to Patients.)
Hypotension and Syncope with Flibanserin Alone
Use of flibanserin alone can cause hypotension and syncope. In controlled studies of premenopausal women with HSDD, hypotension and syncope were reported in 0.2 and 0.4% of flibanserin-treated patients, respectively. The risk of hypotension and syncope is increased if taken during waking hours or in higher than recommended dosages.
Consider the clinical benefits of flibanserin therapy and the risks of hypotension and syncope in patients with preexisting conditions that predispose to hypotension. (See Warnings under Cautions.)
If presyncope occurs, patient should immediately lie supine and promptly seek medical attention if symptoms do not resolve. If syncope occurs, patient should promptly obtain medical attention.
Mammary Tumors in Female Mice
Dose-related increase in incidence of malignant mammary tumors observed in female mice at exposures 3 and 10 times those attained with recommended human dosage; effect not observed in male mice or in male or female rats. Clinical relevance not known.
Specific Populations
Pregnancy
No studies to date in pregnant women. In animal studies, fetal toxicity occurred only in conjunction with substantial maternal toxicity (e.g., reduced weight gain, sedation). Decreased fetal weight, structural abnormalities, and increases in fetal loss occurred at exposures >15 times those achieved with recommended human dosage. Manufacturer states that animal studies cannot exclude potential for fetal harm.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Because of the potential for serious adverse reactions, including sedation, in nursing infants, breast-feeding during flibanserin therapy not recommended.
Pediatric Use
Not indicated for pediatric patients.
Geriatric Use
Not FDA labeled for use in geriatric patients; safety and efficacy not established. Manufacturer states not indicated for treatment of HSDD in postmenopausal women† [off-label]. (See Absorption: Special Populations, under Pharmacokinetics.)
Hepatic Impairment
Contraindicated in patients with hepatic impairment. (See Hypotension and Syncope in Patients with Hepatic Impairment under Cautions and also see Absorption: Special Populations, under Pharmacokinetics.)
Renal Impairment
Exposure only increases slightly in patients with mild to severe renal impairment. Dosage adjustment unlikely to be necessary. (See Absorption: Special Populations, under Pharmacokinetics.)
Pharmacogenomics and Poor CYP2C19 Metabolizers
Peak plasma concentrations and AUC are increased and elimination half-life is prolonged in poor CYP2C19 metabolizers compared with extensive CYP2C19 metabolizers. (See Pharmacokinetics.) Increased monitoring for adverse effects (e.g., hypotension) recommended. Approximately 2–5% of Caucasians and Africans and approximately 2–15% of Asians are poor CYP2C19 metabolizers.
Common Adverse Effects
Dizziness, somnolence, nausea, fatigue, insomnia, dry mouth. Most of these adverse effects began during first 14 days of therapy.
Drug Interactions
Metabolized principally by CYP3A4 and, to a lesser extent, by CYP2C19. CYP 1A2, 2B6, 2C8, 2C9, and 2D6 contribute minimally (<10%) to metabolism.
Inhibits P-glycoprotein (P-gp).
Drugs Affecting Hepatic Microsomal Enzymes
Moderate or potent CYP3A4 inhibitors: Substantially increased flibanserin exposure possible; may lead to hypotension and syncope. Concomitant use contraindicated. (See General under Dosage and Administration and also see Hypotension and Syncope with CYP3A4 Inhibitors under Cautions.)
Weak CYP3A4 inhibitors: Possible increased flibanserin exposure with concurrent use of multiple weak CYP3A4 inhibitors; advise patients of increased risk of adverse effects (e.g., hypotension, syncope, CNS depression). (See Hypotension and Syncope with CYP3A4 Inhibitors under Cautions.)
CYP3A4 inducers: Substantially decreased flibanserin exposure possible. Concomitant use not recommended.
Potent CYP2C19 inhibitors: Potential increased flibanserin exposure; advise patients of increased risk of adverse effects (e.g., hypotension, syncope, CNS depression).
Substrates of P-glycoprotein Transport
Potential increased exposure to P-gp substrates resulting in possible toxicity; more frequent monitoring of concentrations of P-gp substrates with a narrow therapeutic index recommended.
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Increased risk of severe hypotension, syncope, and CNS depression (see Hypotension and Syncope with Alcohol under Cautions) Pharmacokinetics of flibanserin not substantially altered |
If 1–2 standard alcoholic drinks were consumed, allow at least 2 hours to elapse before taking the flibanserin dose at bedtime If ≥3 standard alcoholic drinks were consumed, skip the flibanserin dose that evening After flibanserin is taken at bedtime, do not consume alcohol until the following day |
|
Anticonvulsants (carbamazepine, phenobarbital, phenytoin) |
Possible decreased flibanserin exposure |
Concomitant use not recommended |
|
Antidepressants, SSRIs |
Possible increased flibanserin exposure with SSRIs that are potent CYP2C19 inhibitors (e.g., fluvoxamine); may lead to hypotension, syncope, and CNS depression Fluoxetine (weak CYP3A4 inhibitor): Possible increased flibanserin exposure with multiple weak CYP3A4 inhibitors Paroxetine: No clinically important effects on flibanserin pharmacokinetics |
Fluoxetine and fluvoxamine: Advise patients of the increased risk for adverse effects |
|
Antifungals, azole (fluconazole, itraconazole, ketoconazole, posaconazole, voriconazole) |
Possible increased flibanserin exposure with moderate or potent CYP3A4 inhibitors (fluconazole, itraconazole, ketoconazole, posaconazole, voriconazole) and/or potent CYP2C19 inhibitors (fluconazole); may lead to hypotension, syncope, and CNS depression Fluconazole: Increased peak concentrations and AUC of flibanserin 2.2- and 7-fold, respectively; hypotension and syncope reported Itraconazole: Increased peak concentrations and AUC of flibanserin 1.7- and 2.6-fold, respectively Ketoconazole: Increased peak concentrations and AUC of flibanserin 1.8- and 4.5-fold, respectively |
Concomitant use contraindicated If treatment with an azole antifungal is necessary, discontinue flibanserin ≥2 days prior to initiation of the azole antifungal If benefit of initiating azole antifungal therapy within 2 days of flibanserin discontinuance clearly outweighs risk of hypotension and syncope, monitor for hypotension and syncope Allow ≥2 weeks to elapse between discontinuance of the azole antifungal and reinitiation of flibanserin |
|
Antimycobacterials (rifabutin, rifampin, rifapentine) |
Possible decreased flibanserin exposure Rifampin: Decreased flibanserin exposure by about 95% |
Concomitant use not recommended |
|
Bupropion |
No clinically important effects on bupropion pharmacokinetics |
|
|
Ciprofloxacin |
Possible increased flibanserin exposure; may lead to hypotension and syncope |
Concomitant use contraindicated If treatment with ciprofloxacin is necessary, discontinue flibanserin ≥2 days prior to initiation of ciprofloxacin If benefit of initiating ciprofloxacin therapy within 2 days of flibanserin discontinuance clearly outweighs risk of hypotension and syncope, monitor for hypotension and syncope Allow ≥2 weeks to elapse between discontinuance of ciprofloxacin and reinitiation of flibanserin |
|
CNS depressants (e.g., benzodiazepines, diphenhydramine, sedatives and hypnotics, opiates) |
Possible additive CNS depression |
Advise patients of increased risk for adverse CNS effects |
|
Conivaptan |
Possible increased flibanserin exposure; may lead to hypotension and syncope |
Concomitant use contraindicated If treatment with conivaptan is necessary, discontinue flibanserin ≥2 days prior to initiation of conivaptan If benefit of initiating conivaptan therapy within 2 days of flibanserin discontinuance clearly outweighs risk of hypotension and syncope, monitor for hypotension and syncope Allow ≥2 weeks to elapse between discontinuance of conivaptan and reinitiation of flibanserin |
|
Contraceptives, hormonal |
Possible increased flibanserin exposure and increased risk of adverse effects (e.g., nausea, dizziness, somnolence, fatigue) Pharmacokinetics of oral contraceptive components (ethinyl estradiol and levonorgestrel; weak CYP3A4 inhibitor) not substantially affected |
Advise patients of the increased risk of adverse effects, particularly when used with other weak CYP3A4 inhibitors |
|
Digoxin |
Increased AUC and peak concentrations of digoxin (a P-gp substrate) by 2- and 1.5-fold, respectively; digoxin toxicity possible |
More frequent monitoring of digoxin concentrations recommended |
|
Diltiazem |
Possible increased flibanserin exposure; may lead to hypotension and syncope |
Concomitant use contraindicated If treatment with diltiazem is necessary, discontinue flibanserin ≥2 days prior to initiation of diltiazem If benefit of initiating diltiazem therapy within 2 days of flibanserin discontinuance clearly outweighs risk of hypotension and syncope, monitor for hypotension and syncope Allow ≥2 weeks to elapse between discontinuance of diltiazem and reinitiation of flibanserin |
|
Etravirine |
Etravirine (moderate CYP3A4 inducer) decreased flibanserin exposure by about 21% |
Concomitant use not recommended |
|
Ginkgo |
Possible increased flibanserin exposure with multiple weak CYP3A4 inhibitors |
Advise patients of the increased risk for adverse effects |
|
Grapefruit |
Grapefruit juice (moderate CYP3A4 inhibitor) increased flibanserin AUC and peak concentrations by 1.4- and 1.1-fold, respectively; concomitant use may lead to hypotension and syncope |
Concomitant use contraindicated; advise patients to avoid grapefruit during flibanserin therapy |
|
Histamine H2-receptor antagonists (cimetidine, ranitidine) |
Possible increased flibanserin exposure with multiple weak CYP3A4 inhibitors |
Advise patients of the increased risk for adverse effects |
|
HIV protease inhibitors (PIs) (atazanavir, fosamprenavir, nelfinavir, ritonavir, saquinavir) |
Possible increased flibanserin exposure; may lead to hypotension and syncope |
Concomitant use contraindicated If treatment with the HIV PI is necessary, discontinue flibanserin ≥2 days prior to initiation of the HIV PI If benefit of initiating HIV PI therapy within 2 days of flibanserin discontinuance clearly outweighs risk of hypotension and syncope, monitor for hypotension and syncope Allow ≥2 weeks to elapse between discontinuance of the HIV PI and reinitiation of flibanserin |
|
Macrolides (clarithromycin, erythromycin, telithromycin) |
Possible increased flibanserin exposure; may lead to hypotension and syncope |
Concomitant use contraindicated If treatment with the macrolide is necessary, discontinue flibanserin ≥2 days prior to initiation of the macrolide antibiotic If benefit of initiating macrolide therapy within 2 days of flibanserin discontinuance clearly outweighs risk of hypotension and syncope, monitor for hypotension and syncope Allow ≥2 weeks to elapse between discontinuance of the macrolide and reinitiation of flibanserin |
|
Nefazodone |
Possible increased flibanserin exposure; may lead to hypotension and syncope |
Concomitant use contraindicated If treatment with nefazodone is necessary, discontinue flibanserin ≥2 days prior to initiation of nefazodone If benefit of initiating nefazodone therapy within 2 days of flibanserin discontinuance clearly outweighs risk of hypotension and syncope, monitor for hypotension and syncope Allow ≥2 weeks to elapse between discontinuance of nefazodone and reinitiation of flibanserin |
|
Proton-pump inhibitors (PPIs) |
Possible increased flibanserin exposure with PPIs that are potent CYP2C19 inhibitors |
Advise patients of the increased risk for adverse effects |
|
Resveratrol |
Possible increased flibanserin exposure with multiple weak CYP3A4 inhibitors |
Advise patients of the increased risk for adverse effects |
|
Simvastatin |
AUC and peak concentrations of simvastatin (CYP3A4 substrate) increased by 1.3- and 1.2-fold, respectively, and AUC and peak concentrations of simvastatin acid increased by 1.5- and 1.4-fold, respectively |
|
|
Sirolimus |
Possible increased sirolimus (P-gp substrate) exposure and risk of toxicity |
|
|
St. John's wort (Hypericum perforatum) |
Possible decreased flibanserin exposure |
Concomitant use not recommended |
|
Verapamil |
Possible increased flibanserin exposure; may lead to hypotension and syncope |
Concomitant use contraindicated If treatment with verapamil is necessary, discontinue flibanserin ≥2 days prior to initiation of verapamil If benefit of initiating verapamil therapy within 2 days of flibanserin discontinuance clearly outweighs risk of hypotension and syncope, monitor for hypotension and syncope Allow ≥2 weeks to elapse between discontinuance of verapamil and reinitiation of flibanserin |
Flibanserin Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed following oral administration; peak concentrations attained within approximately 45 minutes (range: 0.75–4 hours).
Undergoes extensive first-pass metabolism; absolute oral bioavailability is 33%.
Steady-state concentrations achieved after 3 days. Exhibits dose-proportional pharmacokinetics. Exposure with once-daily dosing is 1.4-fold higher compared with single-dose administration.
Food
Administration with food delays time to achieve peak concentrations and increases peak concentrations and AUC.
Special Populations
Mild hepatic impairment: AUC increased 4.5-fold.
Renal impairment: AUC slightly increased in patients with mild or moderate and severe renal impairment (by 1.1- and 1.2-fold, respectively).
Effect of age on exposure not systematically evaluated.
Poor CYP2C19 metabolizers: Peak concentrations and AUC are 1.5- and 1.3-fold higher, respectively, than in extensive CYP2C19 metabolizers.
Race: Approximately 1.4-fold higher exposure observed among Japanese women compared with Caucasian women; however, weight-adjusted AUCs were similar, suggesting that difference is likely related to weight rather than race.
Distribution
Extent
Distributed into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
Approximately 98%, mainly to albumin.
Elimination
Metabolism
Extensively metabolized, principally by CYP3A4 and, to a lesser extent, by CYP2C19; CYP isoenzymes 1A2, 2B6, 2C8, 2C9, and 2D6 contribute minimally (<10%).
Metabolized to at least 35 metabolites, mostly in low concentrations; 2 of these appear in substantial concentrations in plasma but are pharmacologically inactive.
Elimination Route
44 and 51% recovered in urine and feces, respectively.
Half-life
Approximately 11 hours.
Special Populations
Mild hepatic impairment: Half-life is prolonged (26 hours).
Poor CYP2C19 metabolizers: Half-life is prolonged to 13.5 hours compared with 11.1 hours in extensive metabolizers.
Stability
Storage
Oral
Tablets
25°C (may be exposed to 15–30°C).
Actions
-
5-HT1A receptor agonist and 5-HT2A receptor antagonist. Also a moderate antagonist at 5-HT2B, 5-HT2C, and dopamine D4 receptors.
-
Precise mechanism of action in treating HSDD in premenopausal women not fully understood, but thought to be related to enhancement of dopaminergic and noradrenergic activity and reduction of serotonergic activity in the prefrontal cortex.
-
Generally, dopamine and norepinephrine are thought to be excitatory and serotonin inhibitory to sexual desire and arousal. Flibanserin-induced activation of inhibitory 5-HT1A receptors and inhibition of excitatory 5-HT2A receptors may result in decreased serotonin release and increased dopamine and norepinephrine concentrations in areas of the prefrontal cortex thought to be involved in sexual interest and desire.
Advice to Patients
-
Importance of advising patients to read the manufacturer's medication guide prior to initiating flibanserin therapy and each time the prescription is refilled.
-
Importance of advising patients to take the prescribed dose exactly as directed (once daily at bedtime) and not to take the drug at any other time of the day, since taking flibanserin during waking hours increases the risk of hypotension, syncope, accidental injury, and CNS depression.
-
If a dose of flibanserin is missed at bedtime, the missed dose should be skipped and the next dose taken at bedtime on the following day. Importance of advising patients not to take the missed dose the next morning or 2 doses of the drug at the same time.
-
Importance of informing patients that taking flibanserin concomitantly or close together in time (i.e., within 2 hours) with alcohol increases the risk of severe hypotension and syncope. To reduce this risk, advise patients to wait at least 2 hours if they consumed 1–2 standard alcoholic drinks before taking flibanserin at bedtime. Also advise patients to skip the bedtime dose of flibanserin if they consumed ≥3 standard alcoholic drinks during that evening. After taking flibanserin at bedtime, advise patients that alcohol should not be consumed until the following day. (See Hypotension and Syncope with Alcohol under Cautions.)
-
Risk of severe hypotension and syncope, particularly when used concurrently with moderate or potent CYP3A4 inhibitors or used in patients with hepatic impairment. Importance of informing patients that use of moderate or potent CYP3A4 inhibitors is contraindicated during flibanserin therapy and that the drug also is contraindicated in patients with hepatic impairment. Counsel patients to ask about potential drug interactions before beginning any new prescription or OTC medication (e.g., cimetidine) or using other products that contain CYP3A4 inhibitors (e.g., grapefruit juice, ginkgo, resveratrol, St. John's wort). (See Interactions.) Importance of advising patients who experience presyncope or lightheadedness to lie down and to seek medical attention if symptoms persist.
-
Risk of somnolence or sedation. Importance of advising patients that concomitant use of other CNS depressants (e.g., alcohol, benzodiazepines, sedative and hypnotic drugs, opiates, diphenhydramine) and taking flibanserin during waking hours can increase the risk of CNS depression. Importance of advising patients not to drive, operate complex machinery, or engage in other activities requiring full alertness until at least 6 hours after taking a dose of flibanserin and until the effects of drug are known.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed; advise women to avoid breast-feeding during flibanserin therapy.
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription, OTC, and recreational drugs and dietary or herbal supplements, as well as any concomitant illnesses (e.g., psychiatric disorders, liver disease, conditions that may predispose to hypotension).
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
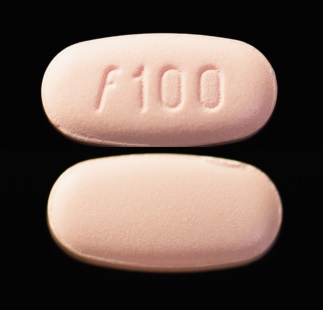
Oral |
Tablets, film-coated |
100 mg |
Addyi |
Sprout |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 26, 2020. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about flibanserin
- Check interactions
- Compare alternatives
- Reviews (75)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous central nervous system agents
- En español