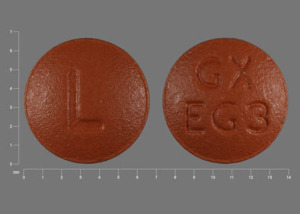
Chlorambucil (Monograph)
Brand name: Leukeran
Drug class: Antineoplastic Agents
- Alkylating Agents
VA class: AN100
CAS number: 305-03-3
Warning
-
May severely suppress bone marrow function. (See Hematologic Effects under Cautions.)
-
Known carcinogen. (See Carcinogenicity under Cautions.)
-
May cause fetal harm. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
-
May cause male or female infertility. (See Fertility under Cautions.)
Introduction
Antineoplastic agent; nitrogen mustard derivative; alkylating agent.
Uses for Chlorambucil
Chronic Lymphocytic Leukemia (CLL)
Treatment of choice (with or without corticosteroids) for adult CLL.
Hodgkin’s Disease
Treatment of adult Hodgkin’s disease; combination regimen that does not include chlorambucil currently is preferred.
Non-Hodgkin’s Lymphoma
Treatment (with or without corticosteroids) of indolent, noncontiguous stage II–IV adult non-Hodgkin’s lymphomas (e.g., follicular lymphoma).
Not curative; rate of relapse is constant over time, even in complete responders.
Optimal treatment as yet unknown; defer treatment in asymptomatic patient and monitor carefully.
Waldenström’s Macroglobulinemia
Drug of choice (with or without prednisone) for Waldenström’s macroglobulinemia† [off-label].
Minimal-change Nephrotic Syndrome
Has been used for the treatment of childhood minimal-change nephrotic syndrome† [off-label].
Second-line agent; use only in those with severe, corticosteroid-dependent or frequently relapsing disease who are intolerant of corticosteroid therapy or whose disease is corticosteroid resistant.
Some clinicians prefer cyclophosphamide to chlorambucil.
Chlorambucil Dosage and Administration
General
-
Optimize results and minimize adverse effects by basing dose on clinical and hematologic response, patient tolerance, and other chemotherapy or irradiation being used.
-
Consult specialized references for procedures for proper handling and disposal of antineoplastic drugs.
Administration
Oral Administration
Administer continuously (as single daily doses) or intermittently (daily for 7 or 10 days every 6 weeks or as biweekly or once-monthly pulse doses).
May administer high doses in intermittent regimens at bedtime with antiemetics to minimize adverse GI effects.
Dosage
Pediatric Patients
Minimal-change Nephrotic Syndrome† [off-label]
Oral
Usual dosage: 0.1–0.2 mg/kg once daily with varying dosages of prednisone for 8–12 weeks; additional course of therapy may be necessary.
Adults
Reduce initial dosage if administered within 4 weeks after full course of radiation therapy or myelosuppressive drugs or if pretreatment leukocyte or platelet counts are depressed from bone marrow disease.
CLL
Oral
Continuous regimen: 0.1–0.2 mg/kg (4–10 mg daily for average patient) given as a single daily dose; usually requires only 0.1 mg/kg daily.
Biweekly (once every 2 weeks) regimen: initially, 0.4 mg/kg; increase doses by 0.1 mg/kg every 2 weeks until a response and/or myelosuppression occurs. Adjust subsequent dosages to produce mild myelosuppression.
Once-monthly regimen: initially, 0.4 mg/kg; increase doses by 0.2 mg/kg every 4 weeks until a response and/or myelosuppression occurs. Adjust subsequent dosages to produce mild myelosuppression.
Therapy usually continued for 3–12 months regardless of regimen and schedule used. Generally discontinued after 1 year and restarted when the disease relapses (in patients who achieved a complete remission) or continued as needed (in those who achieved only a partial response).
Hodgkin’s Disease
Oral
Usual dosage: 0.1–0.2 mg/kg given as a single daily dose for 3–6 weeks; usually requires 0.2 mg/kg daily.
Non-Hodgkin’s Lymphoma
Oral
Usual dosage: 0.1–0.2 mg/kg given as a single daily dose for 3–6 weeks; usually requires only 0.1 mg/kg daily.
Waldenström’s Macroglobulinemia† [off-label]
Oral
Continuous therapy: 0.1 mg/kg daily.
Intermittent therapy: 0.3 mg/kg daily for 7 days every 6 weeks.
Combination therapy: chlorambucil (8 mg/m2 daily) and prednisone (40 mg/m2 daily) for 10 days every 6 weeks.
Therapy usually continued for at least several months regardless of regimen used; optimal duration unknown.
Prescribing Limits
Pediatric Patients
Minimal-change Nephrotic Syndrome† [off-label]
Oral
Maximum total dosage during a single course of therapy: 8.2–14 mg/kg.
Adults
Oral
Daily dose should not exceed 0.1 mg/kg (about 6 mg for average patient) in the presence of lymphocytic infiltration of the bone marrow or hypoplastic bone marrow.
Cautions for Chlorambucil
Contraindications
-
Known hypersensitivity to chlorambucil or any ingredient in the formulation.
-
Disease resistant to prior chlorambucil therapy.
Warnings/Precautions
Warnings
Carcinogenicity
Possible leukemia or secondary malignancies; assess risk/benefits of therapy.
Not recommended by manufacturer for the treatment of nonmalignant diseases.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm (e.g., unilateral renal agenesis); avoid pregnancy during therapy. If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.
Fertility
High incidence of sterility (generally irreversible ) in prepubertal and pubertal males; potential for prolonged or permanent azoospermia in adult males.
Amenorrhea reported in females.
Sensitivity Reactions
Possible angioedema, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, and urticaria.
Potential for cross-sensitivity (rash) between chlorambucil and other alkylating agents.
Discontinue promptly if skin reaction develops.
General Precautions
Hematologic Effects
Slowly progressive lymphopenia is common; return to normal lymphocyte counts generally occurs rapidly after completion of therapy.
Possible dose-dependent, reversible neutropenia after third week of continuous therapy and continuing for up to 10 days after last dose.
Risk of irreversible bone marrow damage increases rapidly with total dose ≥6.5 mg/kg in 1 course of continuous dosing regimen.
Adverse hematologic effects may be less severe with intermittent dosing than with continuous dosing.
If leukocyte count falls abruptly or leukocyte or platelet counts fall below normal values, decrease chlorambucil dosage; discontinue drug for more severe depression.
Seizures
Possible increased risk of seizures in children with nephrotic syndrome and patients receiving high pulse doses of chlorambucil.
Use with caution in patients with a history of seizures or head trauma or those receiving other potentially epileptogenic drugs.
Prior Irradiation or Myelosuppressive Therapy
Possible additive myelosuppressive effects; do not administer at full dosages within 4 weeks after a full course of radiation therapy or myelosuppressive drugs.
Adequate Patient Evaluation and Monitoring
Monitor hematologic status carefully.
Perform weekly CBC; do not allow >2 weeks to elapse between clinical/hematologic evaluations. During first 3–6 weeks of continuous therapy, obtain WBC count 3 or 4 days after each weekly CBC.
Immunization
Avoid administration of live vaccines to immunocompromised patients.
Specific Populations
Pregnancy
Category D. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Lactation
Not known whether chlorambucil is distributed into milk; discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in pediatric patients; however, has been used when benefits thought to outweigh risks.
Possible increased risk of seizures in children with nephrotic syndrome; use with caution in those with a history of seizure disorder or head trauma or receiving concomitant therapy with drugs that lower seizure threshold.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults; titrate dosage carefully, due to greater frequency of decreased hepatic, renal, and/or cardiac function and of concomitant disease and drug therapy observed in the elderly.
Common Adverse Effects
Bone marrow suppression.
Chlorambucil Pharmacokinetics
Absorption
Bioavailability
Rapidly and completely absorbed from GI tract.
Distribution
Extent
Not fully characterized.
Apparently crosses the placenta. Not known whether the drug or its metabolites are distributed into milk.
Plasma Protein Binding
Approximately 99% (mainly albumin).
Elimination
Metabolism
Rapidly and extensively metabolized in the liver, principally to phenylacetic acid mustard (pharmacologically active). Chlorambucil and phenylacetic acid mustard converted to mono- and dihydroxy derivatives.
Elimination Route
Excreted in urine (15–60%) almost completely as metabolites.
Half-life
Chlorambucil: 1.3–1.5 hours.
Phenylacetic acid mustard: 1.8 hours.
Stability
Storage
Oral
Tablets
2–8°C.
Actions
-
Interferes with DNA replication and transcription of RNA; ultimately results in disruption of nucleic acid function.
-
Possesses some immunosuppressive activity, principally due to suppression of lymphocytes.
-
The slowest acting and generally least toxic of the currently available nitrogen mustard derivatives.
Advice to Patients
-
Risk of hypersensitivity, drug fever, myelosuppression, hepatotoxicity, infertility, seizures, GI toxicity, and secondary malignancies.
-
Importance of informing clinicians if rash, bleeding, fever, jaundice, persistent cough, seizures, nausea, vomiting, amenorrhea, or unusual lumps or masses occur.
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed; necessity for clinicians to advise women to avoid pregnancy.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as concomitant illnesses.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
2 mg |
Leukeran |
GlaxoSmithKline |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 1, 2006. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about chlorambucil
- Check interactions
- Compare alternatives
- Reviews (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: alkylating agents
- Breastfeeding
- En español