Acalabrutinib (Monograph)
Brand name: Calquence
Drug class: Antineoplastic Agents
Introduction
Antineoplastic agent; small-molecule inhibitor of Bruton's tyrosine kinase (BTK).
Uses for Acalabrutinib
Mantle Cell Lymphoma
Treatment of mantle cell lymphoma in patients who have received at least 1 prior therapy; designated an orphan drug by FDA for this use.
Current indication based on overall response rate; clinical benefit (e.g., increased survival) not established. Continued FDA approval for this indication may be contingent on verification and description of clinical benefit in additional trials.
Chronic Lymphocytic Leukemia (CLL)/Small Lymphocytic Lymphoma (SLL)
Treatment of CLL or SLL; designated an orphan drug by FDA for treatment of CLL.
Experts generally recommend BTK inhibitors, including acalabrutinib and ibrutinib, among first-line treatment options in patients with symptomatic or progressive CLL.
Acalabrutinib Dosage and Administration
General
Pretreatment Screening
-
Verify pregnancy status in females of reproductive potential prior to initiation of therapy.
Patient Monitoring
-
Monitor for signs and symptoms of infection during therapy and treat promptly if infection occurs.
-
Monitor patients for signs of bleeding and manage appropriately.
-
Monitor CBC counts during therapy.
-
Monitor for development of skin cancers.
-
Monitor for symptoms of arrhythmias and manage appropriately.
Premedication and Prophylaxis
-
In patients at increased risk for opportunistic infections, consider antimicrobial prophylaxis.
Other General Considerations
-
Consider potential benefits and risks of withholding acalabrutinib therapy for 3–7 days prior to and following surgery (based on the type of surgery and bleeding risk).
-
Use sun protection.
Administration
Oral Administration
Administer acalabrutinib tablets orally twice daily, approximately 12 hours apart, without regard to meals.
Swallow tablets whole with water; do not chew, crush, dissolve, or cut.
If a dose is missed by >3 hours, skip that dose and take the next dose at the regularly scheduled time. Do not take extra tablets to make up for missed dose.
Dosage
Adults
Mantle Cell Lymphoma
Oral
100 mg twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Chronic Lymphocytic Leukemia (CLL)/Small Lymphocytic Lymphoma (SLL)
Monotherapy
Oral100 mg twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Combination Therapy with Obinutuzumab
OralPreviously untreatedCLL or SLL: 100 mg twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Initiate acalabrutinib at cycle 1; initiate obinutuzumab at cycle 2, for a total of six 28-day cycles.
Consult obinutuzumab prescribing information for recommended dosage.
When given on the same day, administer acalabrutinib prior to obinutuzumab.
Dosage Modification for Toxicity
If grade 3 or greater nonhematologic toxicity, grade 3 thrombocytopenia with bleeding, grade 4 thrombocytopenia, or grade 4 neutropenia lasting >7 days occurs, interrupt therapy. Following recovery from toxicity (i.e., return to baseline or resolution to grade 1), resume (or discontinue) therapy as described in Table 1. Consult obinutuzumab prescribing information for management of obinutuzumab toxicities.
|
Toxicity Occurrence |
Recommended Dosage after Recovery from Toxicity – (Starting Dosage = 100 mg twice daily) |
|---|---|
|
First |
Restart at 100 mg twice daily |
|
Second |
Restart at 100 mg twice daily |
|
Third |
Restart at 100 mg once daily |
|
Fourth |
Discontinue acalabrutinib |
Concomitant Use with Drugs Affecting Hepatic Microsomal Enzymes
Avoid concomitant use with potent inhibitors of CYP3A; if short-term (e.g., anti-infective therapy for ≤7 days) therapy is necessary, withhold acalabrutinib during such therapy. After discontinuance of the potent CYP3A inhibitor for ≥24 hours, resume previous acalabrutinib dosage.
If used concomitantly with a moderate CYP3A inhibitor, reduce acalabrutinib dosage to 100 mg once daily.
Avoid concomitant use with potent inducers of CYP3A. If concomitant use cannot be avoided, increase acalabrutinib dosage to 200 mg twice daily.
Special Populations
Hepatic Impairment
No dosage adjustments necessary in patients with mild (Child-Pugh class A) or moderate (Child-Pugh class B) hepatic impairment.
Avoid use in patients with severe (Child-Pugh class C) hepatic impairment.
Renal Impairment
No specific dosage recommendations.
Geriatric Patients
No specific dosage recommendations.
Related/similar drugs
Calquence, Imbruvica, Venclexta, rituximab, cyclophosphamide, Revlimid, Rituxan
Cautions for Acalabrutinib
Contraindications
-
None.
Warnings/Precautions
Serious and Opportunistic Infections
Serious and sometimes fatal infections, including bacterial, fungal, viral, or other opportunistic infections, observed.
Most commonly reported grade 3 or 4 infections were respiratory tract infections including pneumonia. Infections caused by hepatitis B reactivation, fungal pneumonia, Pneumocystis jiroveci pneumonia, Epstein-Barr virus reactivation, cytomegalovirus, and progressive multifocal leukoencephalopathy (PML) also observed.
Consider anti-infective prophylactic therapy in patients at increased risk for opportunistic infections.
Monitor for signs and symptoms of infection during therapy and treat promptly if infection occurs.
Hemorrhage
Serious hemorrhagic events, including fatal cases, observed. Major hemorrhage (serious or grade 3 or higher bleeding or any CNS system bleeding) reported in 3% of patients treated with acalabrutinib in clinical trials.
Increased risk of hemorrhagic events with concomitant use of acalabrutinib and antithrombotic agents. Consider risks and benefits and monitor patients for signs of bleeding during concurrent use.
Consider potential benefits and risks of withholding acalabrutinib therapy for 3–7 days prior to and following surgery (based on type of surgery and bleeding risk).
Cytopenias
Cytopenias, including neutropenia, anemia, thrombocytopenia, and lymphopenia, reported. Serious (grade 3 or 4) cytopenias observed.
Monitor CBC counts regularly. If myelosuppression occurs, interrupt therapy, reduce dosage, or discontinue therapy as appropriate.
Second Primary Malignancies
Second primary malignancies, including skin cancers and other solid tumors, reported in 12% of acalabrutinib-treated patients. Skin cancer was the most frequently reported second primary malignancy, occurring in 6% of acalabrutinib-treated patients.
Monitor patients for skin cancers and advise patients to avoid sun exposure.
Atrial Fibrillation and Flutter
Atrial fibrillation and atrial flutter observed.
Risk may be increased in patients with cardiac risk factors, hypertension, previous arrhythmias, or acute infection.
Monitor for symptoms of arrhythmias (e.g., palpitations, dizziness, syncope, dyspnea) and manage appropriately.
Specific Populations
Pregnancy
May cause fetal harm and dystocia based on animal findings.
Pregnancy testing recommended for females of reproductive potential prior to initiating acalabrutinib therapy. If used during pregnancy, apprise of potential fetal hazard.
Lactation
Acalabrutinib and its active metabolite (ACP-5862) distribute into milk in animals. Not known whether the drug or its active metabolite distributes into human milk or if drug has any effect on milk production or the nursing infant. Females should not breast-feed during acalabrutinib therapy and for ≥2 weeks after the last dose of the drug.
Females and Males of Reproductive Potential
Pregnancy testing recommended for females of reproductive potential prior to initiating acalabrutinib therapy.
Advise female patients of reproductive potential to use effective contraception during treatment with acalabrutinib and for ≥1 week following the last dose of the drug.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
In clinical studies in patients with mantle cell lymphoma or chronic lymphocytic leukemia, approximately 68% of patients were ≥65 years of age and approximately 24% were ≥75 years of age. No clinically important differences in efficacy compared with younger adults.
Among patients ≥65 years of age, 59% had grade 3 or higher adverse reactions and 39% had serious adverse reactions. Among patients <65 years of age, 45% had grade 3 or higher adverse reactions and 25% had serious adverse reactions.
Hepatic Impairment
Mild or moderate hepatic impairment does not substantially alter pharmacokinetics.
Safety not evaluated in patients with moderate or severe hepatic impairment. Avoid use in patients with severe hepatic impairment.
Renal Impairment
Mild to moderate renal impairment does not substantially alter pharmacokinetics of acalabrutinib.
Not studied in patients with severe renal impairment or in patients with renal impairment undergoing dialysis.
Common Adverse Effects
Adverse effects (reported in ≥30% of patients): Anemia, neutropenia, upper respiratory tract infection, thrombocytopenia, headache, diarrhea, musculoskeletal pain.
Drug Interactions
Principally metabolized by CYP3A and, to a minor extent, by glutathione conjugation and amide hydrolysis. Metabolism to the principal active metabolite (ACP-5862) mediated principally by CYP3A.
Acalabrutinib is an inhibitor of CYP3A4/5, 2C8, and 2C9; does not inhibit CYP isoenzymes 1A2, 2B6, 2C19, and 2D6; and is an inducer of CYP isoenzymes 3A4, 1A2, and 2B6.
ACP-5862 is an inhibitor of CYP isoenzymes 2C8, 2C9, and 2C19; does not inhibit CYP isoenzymes 3A4/5, 1A2, 2B6, or2D6; and is an inducer of CYP3A4.
Acalabrutinib and ACP-5862 do not inhibit uridine 5'-diphospho-glucuronosyltransferase (UGT) 1A1 or UGT2B7.
Acalabrutinib is a substrate of P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP); not a substrate of organic anion transporter (OAT) 1, OAT3, organic cation transporter (OCT) 2, and organic anion transport proteins (OATP) 1B1 and OATP1B3. Inhibits BCRP. Does not inhibit P-gp, multidrug and toxin extrusion transporter (MATE) 1, OAT1, OAT3, OCT2, OATP1B1, OATP1B3, or MATE2-K.
ACP-5862 is a substrate of P-gp and BCRP but is not a substrate of OATP1B1 or OATP1B3. Inhibits MATE1. Does not inhibit BCRP, P-gp, OAT1, OAT3, OCT2, OATP1B1, OATP1B3, or MATE2-K.
CYP3A Inhibitors
Potent CYP3A inhibitors: Possible pharmacokinetic interaction (increased plasma acalabrutinib concentrations and risk of toxicity). Avoid concomitant use with potent CYP3A inhibitors. If short-term administration of a potent CYP3A inhibitor is required, withhold acalabrutinib during such administration. After discontinuance of the potent CYP3A inhibitor for ≥24 hours, resume previous acalabrutinib dosage.
Moderate CYP3A inhibitors: Possible pharmacokinetic interaction (increased plasma acalabrutinib concentrations and risk of toxicity). If used concomitantly with a moderate CYP3A inhibitor, reduce acalabrutinib dosage to 100 mg once daily.
CYP3A Inducers
Possible pharmacokinetic interaction (decreased plasma acalabrutinib concentrations and reduced efficacy).
Avoid concomitant use with potent CYP3A inducers; if concomitant use cannot be avoided, increase acalabrutinib dosage to 200 mg twice daily.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticoagulants |
Increased risk of hemorrhagic events |
Monitor for signs of bleeding/hemorrhage |
|
Antiplatelet agents |
Increased risk of hemorrhagic events |
Monitor for signs of bleeding/hemorrhage |
|
Diltiazem |
Peak plasma concentration and AUC of acalabrutinib predicted to increase by approximately two- to three-fold |
Reduce acalabrutinib dosage to 100 mg once daily |
|
Erythromycin |
Peak plasma concentration and AUC of acalabrutinib predicted to increase by approximately two-fold |
Reduce acalabrutinib dosage to 100 mg once daily |
|
Fluconazole |
Peak plasma concentration and AUC of acalabrutinib predicted to increase by approximately two- to three-fold |
Reduce acalabrutinib dosage to 100 mg once daily |
|
Itraconazole |
Increased acalabrutinib peak plasma concentrations and AUC by 3.9- and 5.1-fold, respectively |
Avoid concomitant use; if concomitant use required, withhold acalabrutinib therapy during administration of itraconazole; after discontinuance of itraconazole for ≥24 hours, resume previous acalabrutinib dosage |
|
Rabeprazole |
No clinically important differences in acalabrutinib pharmacokinetics |
|
|
Rifampin |
Decreased acalabrutinib peak plasma concentration and AUC by 68% and 77%, respectively |
Avoid concomitant use; if concomitant use unavoidable, increase acalabrutinib dosage to 200 mg twice daily |
Acalabrutinib Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed following oral administration, with median time to peak plasma concentrations of 0.5 hours for acalabrutinib and 0.75 hours for ACP-5862, the active metabolite. Mean absolute bioavailability is 25%.
Exhibits dose-proportionality; exposures of both acalabrutinib and ACP-5862 increase with dose over a dosage range of 75–250 mg. Accumulation does not appear to occur with repeated dosing.
Duration
Median steady-state binding of acalabrutinib to BTK (BTK occupancy) of ≥95% is maintained over a 12-hour dosing interval.
Food
High-fat, high-calorie meal did not substantially alter AUC; peak plasma concentrations decreased by 54% and time to achieve peak concentrations delayed by 1–2 hours compared with administration under fasting conditions.
Special Populations
Mild (Child-Pugh class A) or moderate (Child-Pugh class B) hepatic impairment: Systemic exposure increased by 1.9-fold or 1.5-fold in individuals with mild or moderate hepatic impairment, respectively. Pharmacokinetics of acalabrutinib or ACP-5862 (active metabolite) did not differ in individuals with mild or moderate hepatic impairment (total bilirubin concentrations ≤ULN with AST concentration >ULN or total bilirubin concentrations >ULN with any AST concentration) compared with individuals with normal hepatic function.
Severe hepatic impairment (Child-Pugh class C): Systemic exposure increased by 5.3-fold. No clinically important differences in pharmacokinetics of ACP-5862 (active metabolite) observed.
Mild to moderate renal impairment (estimated GFR ≥30 mL/minute per 1.73 m2 and <89 mL/minute per 1.73 m2 ): Pharmacokinetics not substantially affected.
Severe renal impairment (estimated GFR <29 mL/minute per 1.73 m2) or renal impairment requiring dialysis: Not studied.
Age, body weight, sex, and race: No clinically important effects on pharmacokinetics.
Distribution
Extent
Acalabrutinib and its active metabolite ACP-5862 distribute into milk in animals; not known whether the drug and/or its active metabolite distributes into human milk.
Plasma Protein Binding
Acalabrutinib: 97.5%.
ACP-5862 (active metabolite): 98.6%.
Elimination
Metabolism
Metabolized principally by CYP3A and, to a minor extent, by glutathione conjugation and amide hydrolysis. Principal active metabolite is ACP-5862. Exposure to ACP-5682 is approximately two- to three-fold higher than acalabrutinib exposure. ACP-5862 is approximately 50% less potent than acalabrutinib as a Bruton tyrosine kinase inhibitor.
Elimination Route
Eliminated in feces (84%) and urine (12%), mainly as metabolites; <2% excreted in urine and feces as unchanged drug.
Half-life
Acalabrutinib: Mean of 1.4 hours.
ACP-5862 (active metabolite): Mean of 6.4 hours.
Stability
Storage
Oral
Tablets, Film-Coated
20–25°C (excursions permitted between 15–30°C).
Actions
-
Selectively and irreversibly inhibits Bruton tyrosine kinase (BTK), an essential signaling molecule of the B-cell antigen receptor (BCR) and cytokine receptor pathways.
-
Acalabrutinib and its active metabolite (ACP-5862) bind covalently with a cysteine residue in the BTK active site resulting in inhibition of BTK enzymatic activity.
-
Within B cells, BTK signaling results in activation of pathways involved in cell proliferation, trafficking, chemotaxis, and adhesion. In nonclinical studies, acalabrutinib inhibited the BTK-mediated activation of downstream signaling proteins CD86 and CD69 resulting in decreased malignant B-cell proliferation and tumor growth in mouse xenograft models.
-
Inhibition of BTK also reduces plasma concentrations of cytokines and chemokines, which may lead to decreased cell adhesion and mobilization of cells from tissues. This redistribution of cells from tissues to peripheral blood may contribute to the transient increase in absolute lymphocyte count (lymphocytosis) observed in patients receiving BTK inhibitors (e.g., acalabrutinib, ibrutinib).
-
Unlike ibrutinib (another BTK inhibitor used to treat mantle cell lymphoma), acalabrutinib does not appear to irreversibly target kinases other than BTK, including epidermal growth factor receptor (EGFR), tyrosine kinase expressed in hepatocellular carcinoma (TEC), and interleukin 2-inducible T-cell kinase (ITK). The selective targeting of BTK by acalabrutinib may help explain, at least in part, certain tolerability differences observed between acalabrutinib and ibrutinib in clinical studies to date.
Advice to Patients
-
Advise patients to read the manufacturer's patient information.
-
Advise patients to take acalabrutinib as directed by their clinician. If a dose is missed, inform patients to take the next dose as soon as it is remembered. However, if it has been >3 hours, inform patients to skip the missed dose and to take the next dose at the regularly scheduled time. Inform patients that an extra dose should not be taken to make up for a missed dose.
-
Advise patients to swallow acalabrutinib tablets whole with a glass of water and not to chew, crush, cut, or dissolve the tablets.
-
Inform patients of the risk of bleeding/hemorrhage with acalabrutinib therapy. Advise patients to inform their clinician if signs or symptoms of bleeding occur. Inform patients that acalabrutinib therapy may need to be interrupted for major surgeries.
-
Inform patients of the risk of serious infection with acalabrutinib therapy. Advise patients to promptly report signs or symptoms of possible infection (e.g., fever, chills, flu-like symptoms).
-
Inform patients of the risk of myelosuppression with acalabrutinib therapy. Inform patients that periodic CBC counts are necessary during acalabrutinib therapy.
-
Inform patients of the possible risk of developing a second primary malignancy (e.g., skin cancer, other solid tumors). Advise patients to protect their skin from the sun.
-
Inform patients of the risk of atrial fibrillation and flutter with acalabrutinib therapy. Advise patients to inform their clinician if palpitations, dizziness, fainting, shortness of breath, or chest discomfort occurs.
-
Advise females to inform clinicians if they are or plan to become pregnant or plan to breast-feed. Apprise patient of potential hazard to the fetus and risk of dystocia if acalabrutinib used during pregnancy. Advise females to use effective contraception while receiving acalabrutinib and for ≥1 week after the last dose.
-
Advise females to avoid breast-feeding while receiving acalabrutinib and for ≥2 weeks after the last dose.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care. For further information on the handling of antineoplastic agents, see the ASHP Guidelines on Handling Hazardous Drugs at https://www.ahfsdruginformation.com.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
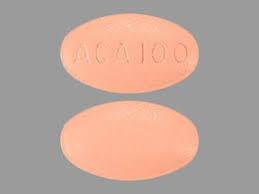
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
100 mg |
Calquence |
AstraZeneca |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
More about acalabrutinib
- Check interactions
- Compare alternatives
- Reviews (18)
- Side effects
- Dosage information
- During pregnancy
- Drug class: BTK inhibitors
- Breastfeeding
- En español