Shoulder Dislocation
What is a Shoulder Dislocation?

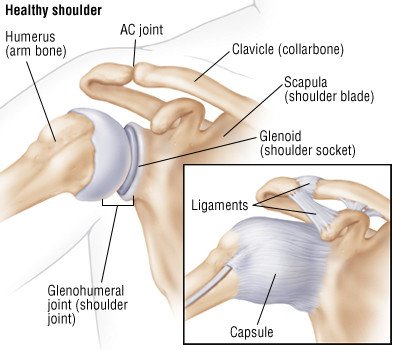
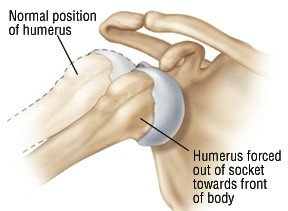
The shoulder joint is called a ball-and-socket joint. The ball is the rounded top of the bone in the upper arm (humerus), which fits into the socket — the cup-shaped outer part of the shoulder blade. When the top of the humerus moves out of its usual location in the shoulder joint, the shoulder is said to be dislocated. A related injury called a shoulder subluxation occurs when the top of the humerus is only partially displaced and not totally out of its socket.
|
|
In some cases, a shoulder is dislocated when the arm is pulled or twisted with extreme force in an outward, upward or backward direction. This extreme force literally pops the top of the humerus out of its socket. In other cases, a shoulder dislocation is the result of a fall on an outstretched arm, a direct forceful blow to the shoulder, a seizure or a severe electric shock. Seizures and shock can cause shoulder dislocations because they produce extreme, unbalanced muscle contractions that can wrench the humerus out of place.
Doctors classify shoulder dislocations into three types, depending on the direction of the dislocation:
- Anterior dislocation — The top of the humerus is displaced forward, toward the front of the body. This is the most common type of shoulder dislocation, accounting for more than 95% of cases. In young people, the cause is typically sports-related. In older people, it usually is caused by a fall on an outstretched arm.
|
|
- Posterior dislocation — The top of the humerus is displaced toward the back of the body. Posterior dislocations account for 2% to 4% of all shoulder dislocations and are the type most likely to be related to seizures and electric shock. Posterior dislocations also can happen because of a fall on an outstretched arm or a blow to the front of the shoulder.
- Inferior dislocation — The top of the humerus is displaced downward. This type of shoulder dislocation is the rarest, occurring in only one out of every 200 cases. It can be caused by various types of trauma in which the arm is pushed violently downward.
Almost all shoulder dislocations are related to trauma. Occasionally, the dislocation occurs after ordinarily harmless motions, such as raising an arm or rolling over in bed. In these mysterious cases, the real cause may be that the shoulder ligaments are abnormally loose. Loose ligaments are sometimes due to an inherited condition that can increase a person's risk of dislocation in other body joints as well.
Shoulder dislocations are the most common joint dislocation seen by emergency room doctors, accounting for more than 50% of all dislocations treated in hospitals. Young adult men and older women tend to be the groups with the highest rate of shoulder dislocations.
Symptoms
Symptoms of a dislocated shoulder include:
- Severe shoulder pain
- Limited motion of the shoulder
- A distortion in the contour of the shoulder — In an anterior dislocation, the side silhouette of the shoulder has an abnormal squared-off appearance instead of its typical sloping, rounded contour. In a posterior dislocation, the front of the shoulder may look abnormally flat.
- A hard knob under the skin near the shoulder — This knob is the top of the humerus that has popped out of its socket.
- Shoulder bruising or abrasions if an impact has caused your injury
Diagnosis
The doctor will examine both shoulders, comparing your injured shoulder with your uninjured one. The doctor will check for swelling, shape changes, abrasions, bruising, pain when you move, tenderness and limited motion at the shoulder joint. The doctor will gently press and feel the area around your shoulder to locate the displaced head of the humerus under the skin. In addition, because many important blood vessels and nerves travel through your shoulder area, your doctor will check the strength of the pulses at your wrist and elbow and check your muscle strength and your response to touch on your arm, hand and fingers. In particular, your doctor will look for numbness on the outside of your upper arm, a sign of injury to the axillary nerve, which is vulnerable to injury in a shoulder dislocation.
If the results of your physical examination suggest that that you have a dislocated shoulder, your doctor will order shoulder X-rays to confirm the diagnosis.
Expected Duration
Once your displaced humerus is slipped back into its socket, your ability to move your shoulder probably will improve immediately, and the full range of motion should return fully within six to eight weeks if you faithfully follow an exercise program. Although most shoulder strength usually returns within three months, regaining full strength may take up to one year.
Prevention
If you have had a dislocated shoulder, you may be able to prevent a repeat injury by doing shoulder strengthening exercises recommended by your doctor or physical therapist. Once you have dislocated your shoulder, you are more likely to dislocate it again, particularly if you play a contact sport.
Treatment
When the arm bone is forced out of its socket, it remains attached to the muscles of the shoulder blade and upper chest. These muscles pull the arm bone against the shoulder and chest, even when the bone is out of its socket and off center. If these muscles are in spasm, they need to be relaxed before the doctor can move the arm bone back into its socket. Your doctor may give you medications to ease your pain and relax your shoulder muscles. Then the doctor will pull carefully against these muscles until the head of your humerus slips back into its socket. Sometimes, doctors use arm weights on the side of the dislocation to make it easier to extend these tight muscles. This treatment, with or without the weights, is called closed reduction.
Once your shoulder joint is back in its normal position, you will rest your arm in a sling for one to four weeks. Teenagers tend to need the sling longer than older people. You also will begin a physical therapy program to restore the normal strength and range of motion in your shoulder joint.
If you continue to have severe shoulder pain after closed reduction or if your injured shoulder is loose and unstable in spite of physical therapy, you may need surgery to repair the fibrous tissues that support your shoulder joint.
When To Call a Professional
Call your doctor immediately if you cannot move your shoulder after a fall or other traumatic injury or if your shoulder is painful, swollen, tender or unusually shaped.
Prognosis
The outlook depends on many factors, including the severity of your shoulder injury, your age and your participation in athletic activity. For example, if you are a teenaged athlete and you play contact sports, such as football or hockey, after a shoulder dislocation, your overall risk of a second shoulder dislocation may be as high as 90%. Repeat injury may make your shoulder unstable enough that it needs to be repaired with surgery. Surgery usually restores the shoulder's stability and reduces the risk of future dislocation to 5% or less.
If you are an adult and have an uncomplicated shoulder dislocation, your risk of a second dislocation is low, with repeat dislocations occurring only about 25% of the time for people in their 30s and even less often for older age groups.
Additional Info
National Institute of Arthritis and Musculoskeletal and Skin Diseases
http://www.niams.nih.gov/
National Rehabilitation Information Center (NARIC)
http://www.naric.com/
National Athletic Trainers' Association
http://www.nata.org/
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.