Melanoma
Medically reviewed by Drugs.com. Last updated on Jun 1, 2023.
What is Melanoma?

Melanoma is cancer of the cells ("melanocytes") that give skin its color. It develops when these cells change and reproduce aggressively. The number of cases of melanoma, the deadliest form of skin cancer, is increasing faster than any other cancer.
Doctors aren't completely sure why melanoma rates are soaring. It could be from spending too much time in the sun during outdoor activities. It could also be due to global changes, such as the depletion of the ozone, which absorbs many of the sun's harmful rays.
Your pattern of sun exposure appears to affect your risk of developing melanoma more than the total amount of sun exposure in your lifetime. Short bursts of intense sun seem most dangerous, especially if you get sunburned. Being out in the sun can cause changes (mutations) in skin cells' genes. Researchers have recently found several gene mutations shared by many melanoma tumor cells. It is likely that one or more of these mutations starts the cancer.
The most common type of melanoma spreads on the skin's surface. It is called superficial spreading melanoma. It may stay on the surface or grow down into deeper tissues. Other types of melanoma can start anywhere on or inside the body.
|
|
Your risk of developing melanoma is higher if you have:
- Red or blond hair
- Green or blue eyes
- Fair skin
- A history of being in the sun a lot, especially as a child
- A mother, father, sister or brother with melanoma. If one of these relatives has melanoma, you are eight times more likely to develop it.
Features of freckles or moles that raise your risk of melanoma include:
- A new mole appearing after age 30
- A new mole at any age if it is in an area rarely exposed to the sun
- A change in an existing mole
- One or more atypical moles—moles that look like a fried egg or moles that are darker than others or have irregular borders or an irregular shape.
- 20 or more moles larger than 2 millimeters across
- 5 or more moles larger than 5 millimeters across (larger than a pencil eraser)
- Freckles caused by being in the sun
Symptoms
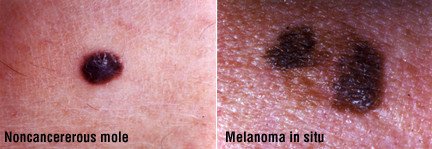
Melanoma is usually visible as a single dark skin spot. It may appear anywhere on the body, but it most commonly develops on the back, chest, and legs. Most of the time, melanoma develops on normal-looking skin, but it can grow out of an existing mole.
Watch a mole for the A, , C, D and Es of melanoma:
- Asymmetry (one side doesn't match the other)
- order irregularities
- Colors or shades of skin that are different within the same mole
- Diameter larger than 6 millimeters (larger than a pencil eraser)
- Evolving (a newly developing mole)
A mole that bleeds, feels numb, or has a crusty surface may also hint at melanoma.
|
|
Diagnosis
If your doctor thinks a mole may be melanoma, he or she will do a biopsy of the skin or refer you to a specialist for the procedure.
Before the biopsy, your doctor will check for enlarged lymph nodes close to the mole. If you have a melanoma, enlarged lymph nodes can mean that the cancer has spread. After a skin biopsy, nearby lymph nodes can swell because the skin incision is healing.
In a biopsy, a doctor removes a piece of tissue and examines it in a laboratory. Based on this report, your doctor can then determine the thickness of the melanoma and how deep the cancer has grown below the skin's surface. That's the most important factor in predicting whether it can be cured.
Melanomas deeper than 1 millimeter are more likely to have spread to other parts of the body. Your doctor may suggest additional tests including:
- Blood tests
- A chest x-ray
- Computed tomography (CT)scans
- Additional biopsies
If the cancer is advanced, the biopsy sample of your melanoma may be tested to see if it has one of the gene mutations common in melanoma. Some melanoma treatments have been designed to attack specific genetic subtypes of this cancer.
Expected duration
Melanoma can usually be cured if it is removed when the tumor has not gone deep into the skin. More advanced melanoma requires longer treatment. If you have one melanoma, you are at risk of developing another, so have a doctor examine your skin regularly. About 1 out of 20 people who have a melanoma will develop a second melanoma within 20 years.
Prevention
To reduce your risk of melanoma, stay out of the sun. A bad sunburn is a major risk factor. Spending a lot of time in the sun as a child may pose the greatest risk. To be safe in the sun, take these steps:
- Apply plenty of sunscreen and apply it frequently. It should:
- Have a sun protection factor (SPF) of at least 30.
- Provide broad spectrum coverage against both UVA and UVB rays
- Be water resistant
- Wear protective sunglasses, clothing (long sleeves and long pants) and wide-brimmed hats.
- Stay out of the sun when it is strongest (10 a.m. to 4 p.m.).
- Ask your doctor if any medications you take could make your skin more likely to be damaged by the sun.
- Avoid tanning salons. If you want to look tan, use sunless tanning creams. They are available in department and drug stores.
Melanoma is often easy to spot early, because it can be seen on your skin. If you are at risk of developing melanoma, ask your doctor to examine your skin. Also ask your doctor how often you should have your skin checked.
Your doctor will pay special attention to any atypical looking moles. Because some melanomas can arise from existing moles, your doctor may remove atypical moles. These moles may be more likely to become cancerous. Alternatively, your doctor may take pictures of your moles. He or she can compare the photos to your moles in the future to see if they have changed.
Examine your skin regularly, especially if you have risk factors for melanoma. Use a full-length and hand-held mirror. Have someone examine your scalp using a blow dryer to part your hair. That person can also examine your back and other areas that you can't easily see. Watch for new moles and changes in existing ones. Keep an eye on moles that you've had since birth; these moles may be more likely to turn into melanoma.
Treatment
Major advances have been made in the treatment of melanoma.
Surgery is the initial treatment for melanoma that appears in just one spot. The doctor removes the visible tumor along with 1 to 2.5 centimeters of healthy skin around the tumor, depending on the size of the tumor. (Nearby skin can contain microscopic bits of the cancer.)
In some cases, the doctor may perform a specialized procedure during which the tumor is shaved away one thin layer at a time. Each layer is examined under the microscope as it is removed. This technique helps the doctor remove as little healthy skin as possible.
If the melanoma is more than 1 millimeter deep, your doctor will want to know if the melanoma has spread to nearby lymph nodes. To do this, he or she may inject a radioactive liquid into the tumor. The liquid flows through the natural drainage pathway that connects the tumor to nearby lymph nodes.
The drainage path can be tracked, and the first lymph node along the path is called the sentinel node. This node is removed and examined for cancer cells. If the sentinel node has no cancer, the other nodes are most often cancer-free.
If cancer is found in the sentinel node, most often all the lymph nodes in the area will be removed. However, it's not been absolutely proven that removing all lymph nodes improves survival. Although spreading cancer cells might be removed, cells that are fighting the cancer also are removed.
When cancer has spread to one or two other sites only, surgical removal similar to what was done the first time can improve survival.
Additional therapies can often help people with thicker tumors that have grown deep into the skin and/or spread to more areas of the body. The cancer cells are tested for certain specific markers. The results guide the type of therapy that has the greatest chance of improving quality of life and survival.
Most often patients are treated with immunotherapy and/or drugs designed to block major pathways that allow cancers to grow. Radiation therapy and chemotherapy are less effective. But they can be used when other therapies don't work or stop working.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
When to call a professional
Early treatment of melanoma is crucial. If you detect any of the ABCDE signs or see any suspicious skin changes, call your doctor right away. If you delay, melanoma can spread. If melanoma runs in your family, of if you have other risk factors, be especially alert. Have your doctor examine your skin regularly.
Prognosis
Five key factors help to determine how serious melanoma is:
- Tumor thickness — How deep it goes into the skin.
- Location — Melanoma on the arms or legs may not be as serious as a tumor somewhere else on the body.
- Age — People older than 60 are in more danger.
- Gender — Males are more likely to die of the disease.
- Spreading of the tumor — Twenty percent of people with melanoma have cancer in lymph nodes when their cancer is diagnosed.
The thickness of the tumor is the most important factor in determining whether it can be treated. Tumors on the skin's surface usually can be cured. Deeper cancers are more difficult, sometimes impossible, to treat. If melanoma cells break away and spread to organs such as the lungs, liver or brain, the cancer can be cured in only a small number of patients.
If treatment begins when the tumor is less than 0.75 millimeters deep, the chance of a cure is excellent. More than 95% of people with small melanomas are cancer-free as long as 8 years later. However, for deeper melanomas, the survival rate is poor. Fewer than half of people with tumors thicker than 4 millimeters survive for 5 years. If melanoma cells are found in a lymph node, the 5-year survival rate is between 30% and 50%.
Additional information
National Cancer Institute (NCI)
http://www.cancer.gov/
American Cancer Society (ACS)
http://www.cancer.org/
Cancer Research Institute
http://www.cancerresearch.org/
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.