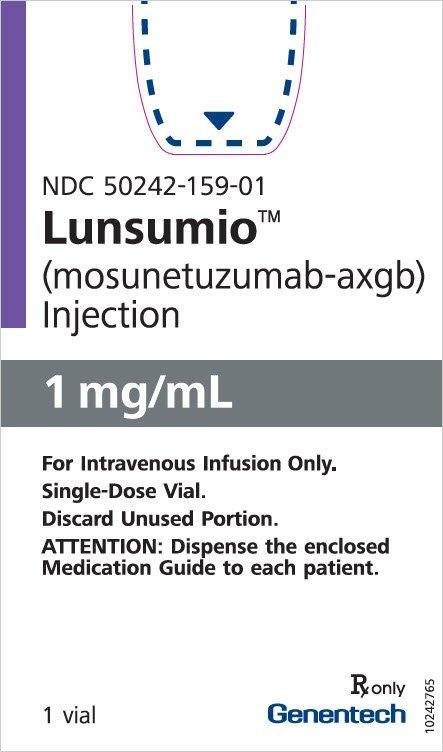
Lunsumio Injection Dosage
Generic name: MOSUNETUZUMAB 30mg in 30mL
Dosage form: injection, concentrate
Drug class: Miscellaneous antineoplastics
Medically reviewed by Drugs.com. Last updated on Dec 22, 2022.
Important Dosing Information
- Administer LUNSUMIO to well-hydrated patients.
- Premedicate before each dose in Cycle 1 and Cycle 2 [see Dosage and Administration (2.2)].
- Administer only as an intravenous infusion through a dedicated infusion line. Do not use an in-line filter to administer LUNSUMIO. Drip chamber filters can be used to administer LUNSUMIO.
- LUNSUMIO should only be administered by a qualified healthcare professional with appropriate medical support to manage severe reactions such as cytokine release syndrome and neurologic toxicity [see Warnings and Precautions (5.1 and 5.2)].
Recommended Dosage
The recommended dosage for LUNSUMIO is presented in Table 1.
Administer for 8 cycles, unless patients experience unacceptable toxicity or disease progression.
For patients who achieve a complete response, no further treatment beyond 8 cycles is required. For patients who achieve a partial response or have stable disease in response to treatment with LUNSUMIO after 8 cycles, an additional 9 cycles of treatment (17 cycles total) should be administered, unless a patient experiences unacceptable toxicity or disease progression.
| Day of Treatment | Dose of LUNSUMIO | Rate of Infusion | |
|---|---|---|---|
| Cycle 1 | Day 1 | 1 mg | Administer over a minimum of 4 hours. |
| Day 8 | 2 mg | ||
| Day 15 | 60 mg | ||
| Cycle 2 | Day 1 | 60 mg | Administer over 2 hours if infusions from Cycle 1 were well-tolerated. |
| Cycles 3+ | Day 1 | 30 mg | |
| Last Dose Administered | Time Since the Last Dose Administered | Action for Next Dose(s) |
|---|---|---|
| 1 mg Cycle 1 Day 1 |
1 to 2 weeks | Administer 2 mg (Cycle 1 Day 8), then resume the planned treatment schedule. |
| Greater than 2 weeks | Repeat 1 mg (Cycle 1 Day 1), then administer 2 mg (Cycle 1 Day 8) and resume the planned treatment schedule. | |
| 2 mg Cycle 1 Day 8 |
1 to 2 weeks | Administer 60 mg (Cycle 1 Day 15), then resume the planned treatment schedule. |
| Greater than 2 weeks to less than 6 weeks | Repeat 2 mg (Cycle 1 Day 8), then administer 60 mg (Cycle 1 Day 15) and resume the planned treatment schedule. | |
| Greater than or equal to 6 weeks | Repeat 1 mg (Cycle 1 Day 1) and 2 mg (Cycle 1 Day 8), then administer 60 mg (Cycle 1 Day 15) and resume the planned treatment schedule. | |
| 60 mg Cycle 1 Day 15 |
1 week to less than 6 weeks | Administer 60 mg (Cycle 2 Day 1), then resume the planned treatment schedule. |
| Greater than or equal to 6 weeks | Repeat 1 mg (Cycle 2 Day 1) and 2 mg (Cycle 2 Day 8), then administer 60 mg (Cycle 2 Day 15), followed by 30 mg (Cycle 3 Day 1) and then resume the planned treatment schedule. | |
| 60 mg Cycle 2 Day 1 |
3 weeks to less than 6 weeks | Administer 30 mg (Cycle 3 Day 1), then resume the planned treatment schedule. |
| Greater than or equal to 6 weeks | Repeat 1 mg (Cycle 3 Day 1) and 2 mg (Cycle 3 Day 8), then administer 30 mg (Cycle 3 Day 15)*, followed by 30 mg (Cycle 4 Day 1) and then resume the planned treatment schedule. | |
| 30 mg Cycle 3 onwards |
3 weeks to less than 6 weeks | Administer 30 mg, then resume the planned treatment schedule. |
| Greater than or equal to 6 weeks | Repeat 1 mg on Day 1 and 2 mg on Day 8 during the next cycle, then administer 30 mg on Day 15*, followed by 30 mg on Day 1 of subsequent cycles. | |
Recommended Premedication and Prophylactic Medication
Premedication to reduce the risk of cytokine release syndrome and infusion-related reactions are outlined in Table 3 [see Warnings and Precautions (5.1)].
| Treatment Cycle | Patients Requiring Premedication | Premedication | Dosage | Administration |
|---|---|---|---|---|
| Cycle 1 and Cycle 2 | All patients | Corticosteroid | Dexamethasone 20 mg intravenous or methylprednisolone 80 mg intravenous | Complete at least 1 hour prior to infusion |
| Antihistamine | Diphenhydramine hydrochloride 50 mg – 100 mg or equivalent oral or intravenous antihistamine | At least 30 minutes prior to infusion | ||
| Antipyretic | Oral acetaminophen (500 mg – 1,000 mg) | At least 30 minutes prior to infusion | ||
| Cycles 3+ | Patients who experienced any grade CRS with the previous dose | Corticosteroid | Dexamethasone 20 mg intravenous or methylprednisolone 80 mg intravenous | Complete at least 1 hour prior to infusion |
| Antihistamine | Diphenhydramine hydrochloride 50 mg – 100 mg or equivalent oral or intravenous antihistamine | At least 30 minutes prior to infusion | ||
| Antipyretic | Oral acetaminophen (500 mg – 1,000 mg) | At least 30 minutes prior to infusion |
Dosage Modifications for Adverse Reactions
See Tables 4 and 5 for the recommended dosage modifications for adverse reactions of CRS and neurologic toxicity, including Immune Effector Cell Associated Neurotoxicity (ICANS). See Table 6 for the recommended dosage modifications for other adverse reactions following administration of LUNSUMIO.
Dosage Modifications for Cytokine Release Syndrome
Identify cytokine release syndrome (CRS) based on clinical presentation [see Warnings and Precautions (5.1)]. Evaluate for and treat other causes of fever, hypoxia, and hypotension.
If CRS is suspected, withhold LUNSUMIO until CRS resolves, manage according to the recommendations in Table 4 and per current practice guidelines. Administer supportive therapy for CRS, which may include intensive care for severe or life-threatening CRS.
| Grade* | Presenting Symptoms | Actions† |
|---|---|---|
|
||
| Grade 1 | Fever ≥ 100.4°F (38°C)‡ |
|
| Grade 2 | Fever ≥ 100.4°F (38°C)‡ with: Hypotension not requiring vasopressors and/or hypoxia requiring low-flow oxygen# by nasal cannula or blow-by. |
|
Recurrent Grade 2 CRS
|
||
| Grade 3 | Fever ≥ 100.4°F (38°C)‡ with: Hypotension requiring a vasopressor (with or without vasopressin) and/or hypoxia requiring high flow oxygen# by nasal cannula, face mask, non-rebreather mask, or Venturi mask. |
|
Recurrent Grade 3 CRS
|
||
| Grade 4 | Fever ≥ 100.4°F (38°C)‡ with: Hypotension requiring multiple vasopressors (excluding vasopressin) and/or hypoxia requiring oxygen by positive pressure (e.g., CPAP, BiPAP, intubation and mechanical ventilation). |
|
Dosage Modifications for Neurologic Toxicity, including ICANS
Management recommendations for neurologic toxicity, including ICANS, is summarized in Table 5. At the first sign of neurologic toxicity, including ICANS, withhold LUNSUMIO and consider neurology evaluation. Rule out other causes of neurologic symptoms. Provide supportive therapy, which may include intensive care.
| Adverse Reaction | Severity*,† | Actions |
|---|---|---|
|
||
| Neurologic Toxicity* (Including ICANS†) |
Grade 2 |
|
| Grade 3 |
|
|
| Grade 4 |
|
|
| Adverse Reactions* | Severity* | Actions |
|---|---|---|
|
||
| Infections [see Warnings and Precautions (5.3)] | Grades 1 – 4 |
|
| Neutropenia [see Warnings and Precautions (5.4)] | Absolute neutrophil count less than 0.5 × 109/L |
|
| Other Adverse Reactions [see Warnings and Precautions (5.5) and Adverse Reactions (6.1)] | Grade 3 or higher |
|
Preparation and Administration
Preparation
Use aseptic technique to prepare LUNSUMIO.
- Inspect the vial visually for any particulate matter, prior to administration. Do not use if the solution is discolored, or cloudy, or if foreign particles are present.
- Determine the dose, the total volume of LUNSUMIO solution required, and the number of LUNSUMIO vials needed.
Dilution
- 1.
- Withdraw the volume from an infusion bag of 0.9% Sodium Chloride Injection, USP or 0.45% Sodium Chloride Injection, USP equal to the volume of the LUNSUMIO required for the patient's dose and discard. Only use infusion bags made of polyvinyl chloride (PVC) or polyolefin (PO) such as polyethylene (PE) and polypropylene.
- 2.
- Withdraw the required volume of LUNSUMIO from the vial using a sterile needle and syringe and dilute into the infusion bag of 0.9% Sodium Chloride Injection, USP or 0.45% Sodium Chloride Injection, USP according to Table 7. Discard any unused portion left in the vial.
| Dose of LUNSUMIO | Volume of LUNSUMIO in 0.9% or 0.45% Sodium Chloride Solution | Size of Infusion Bag |
|---|---|---|
| 1 mg | 1 mL | 50 mL or 100 mL |
| 2 mg | 2 mL | 50 mL or 100 mL |
| 60 mg | 60 mL | 100 mL or 250 mL |
| 30 mg | 30 mL | 50 mL, 100 mL, or 250 mL |
- 3.
- Gently mix the intravenous bag by slowly inverting the bag. Do not shake.
- 4.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use if visibly opaque particles, discoloration, or foreign particles are observed.
- 5.
- Apply the peel-off label from the package insert to the infusion bag.
- 6.
- Immediately use diluted LUNSUMIO infusion solution. If not used immediately, the diluted solution can be stored refrigerated at 2°C to 8°C (36°F to 46°F) for up to 24 hours and at ambient temperature 9°C to 30°C (48°F to 86°F) for up to 16 hours. Prior to administration, ensure the infusion solution comes to reach room temperature.
Administration
- Administer as an intravenous infusion only.
- Do not use an in-line filter to administer LUNSUMIO.
- Do not mix LUNSUMIO with, or administer through the same infusion line, as other medicinal products.
- No incompatibilities have been observed between LUNSUMIO and intravenous infusion bags with product contacting materials of polyvinyl chloride (PVC), or polyolefins (PO) such as polyethylene (PE) and polypropylene (PP). In addition, no incompatibilities have been observed with infusion sets or infusion aids with product contacting materials of PVC, PE, polyurethane (PUR), polybutadiene (PBD), silicone, acrylonitrile butadiene styrene (ABS), polycarbonate (PC), polyetherurethane (PEU), fluorinated ethylene propylene (FEP), or polytetrafluorethylene (PTFE), or with drip chamber filter membrane composed of polyamide (PA).
Frequently asked questions
More about Lunsumio (mosunetuzumab)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1)
- Drug images
- Side effects
- During pregnancy
- FDA approval history
- Drug class: miscellaneous antineoplastics
- Breastfeeding
Patient resources
Professional resources
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.