Ventricular Septal Defect in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
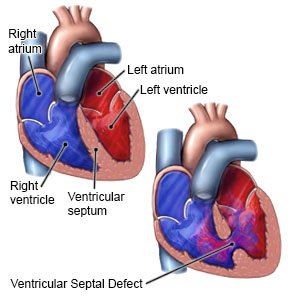
What is a ventricular septal defect (VSD)?
A VSD is a common kind of heart defect. An opening between the 2 lower chambers (ventricles) of your child's heart stays open. Normally, this opening closes before a baby is born. A VSD can cause blood to flow back into the right side of the heart instead of to the rest of your child's body. A VSD can lead to heart or lung problems or to low oxygen levels in your child's blood.
 |
What are the signs and symptoms of a VSD?
Your child may not have any signs and symptoms if the opening is small. The following are common signs and symptoms that may develop:
- A heart murmur (abnormal sound)
- Sweating, especially after eating
- Trouble breathing, fast breathing, or a fast heart rate
- Pale skin or blue lips and fingernails
- Poor weight gain or failure to thrive
- Easily fatigued
How is a VSD diagnosed?
Your child's healthcare provider will listen to your child's heart for a murmur. Your child may also need any of the following:
- A pulse oximeter measures the amount of oxygen in your child's blood.
- A chest x-ray is taken to look at your child's heart and lungs.
- An EKG test records your child's heart rhythm and how fast his or her heart beats.
- An echocardiogram is a type of ultrasound. Sound waves are used to show the structure and function of your child's heart.
- Cardiac catheterization is a procedure to look at your child's heart or measure pressure in his or her heart. Your child's healthcare provider will insert a catheter into a blood vessel in his or her arm, leg, or neck. Contrast liquid may be given to help healthcare providers see your child's heart and blood vessels better. Tell your child's healthcare provider if he or she has ever had an allergic reaction to contrast liquid.
How is a VSD treated?
Your child's healthcare provider may recommend that he or she have regular tests and follow-up visits to see if the opening closes. Your child may also need any of the following:
- Medicines help your child's body get rid of extra fluid, which can help your child breathe easier. Your child may also need medicine to help his or her heart beat more strongly or more regularly.
- A nasogastric (NG) tube may be needed if your baby has trouble feeding. An NG tube is used to give liquid nutrition and medicine. The tube is put into your baby's nose and guided down into his or her stomach.
- Respiratory support includes oxygen, an endotracheal (ET) tube, or a ventilator. These can help your child breathe.
- Surgery may be needed to close the VSD in your child's heart. Surgery may be done as open heart surgery. It may also be done by inserting a catheter into a blood vessel in your child's groin. A small device will be inserted through the catheter to close the VSD.
Call your local emergency number (911 in the US) for any of the following:
- Your child has sudden trouble breathing.
- Your child has weakness or numbness in an arm, leg, or on his or her face.
When should I seek immediate care?
- Your child's lips or fingernails are blue or pale.
- Your child coughs up blood.
When should I call my child's doctor?
- Your child has a fever.
- Your child has chills, a cough, or feels weak and achy.
- Your child has swelling in his or her arms or legs.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Ventricular Septal Defect
- Atorvastatin (Lipitor): Top 12 Drug Facts You Need to Know
- Do blood pressure drugs interact with alcohol?
- Side Effects of Weight Loss Drugs
Treatment options
Care guides
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
