Total Knee Replacement
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
What do I need to know about total knee replacement (TKR)?
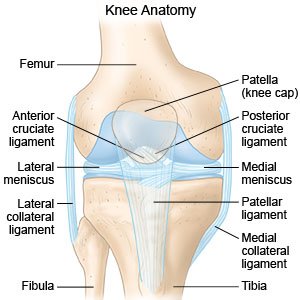
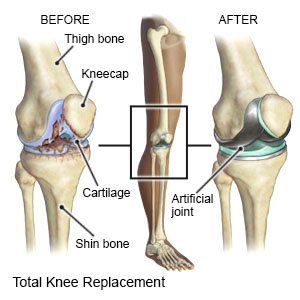
TKR, or knee arthroplasty, is surgery to replace all or part of your knee joint.
 |
How do I prepare for TKR?
- Your surgeon will tell you how to prepare. Your surgeon may tell you not to eat or drink anything after midnight on the day of your surgery. Arrange to have someone drive you home when you are discharged.
- Tell your surgeon about all medicines you currently take. Your surgeon will tell you if you need to stop any medicine for the surgery, and when to stop. Your surgeon will tell you which medicines to take or not take on the day of surgery.
- Tell your surgeon about any allergies you have, including anesthesia or medicines. You may be given an antibiotic to help prevent a bacterial infection.
- Your surgeon will tell you if you need any tests before your surgery, and when to have them.
- You may need blood and urine tests before your surgery. These tests show how well your kidneys are functioning and your blood is clotting. You may also need x-rays or an ultrasound.
What will happen during TKR?
- You may be given general anesthesia to keep you asleep and free from pain during surgery. You may instead be given spinal, or regional, anesthesia. This type will numb you from the waist down. You may still feel pressure or pushing, but you should not feel any pain.
- Your surgeon will make an incision over your knee joint. The damaged parts of your knee joint will be removed and replaced with a knee implant. The knee implant may be made of metal and plastic. Your surgeon may secure it with medical cement.
- Your surgeon will move the muscles and other tissues around your joint back into place. Your incision will be closed with stitches or staples. You may have strips of medical tape and a bandage to cover your incision area.
 |
What should I expect after TKR?
You may have increased pain or stiffness after surgery. This will get better with movement and exercise. Providers will teach you how to sit up and move without damaging your knee. A physical therapist will help you get up and walk after surgery. You may need a walker.
What are the risks of TKR?
You may bleed more than expected or get an infection. Nerves or blood vessels may be damaged during surgery. After surgery, your knee may be stiff or numb. You may continue to have knee pain. Your implant may get loose or move out of place. The implant may get worn out over time and need to be replaced. You may get a blood clot in your limb. This may become life-threatening.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
