Supraventricular Tachycardia
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
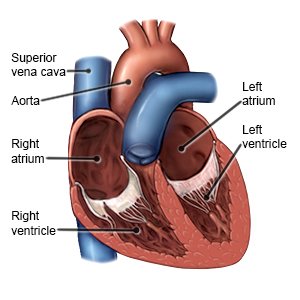
Supraventricular tachycardia (SVT) is a condition that causes your heart to beat much faster than it should. SVT is a type of abnormal heart rhythm, called an arrhythmia, that starts in the upper part of your heart. It may last a few seconds or hours to several days.
 |
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
Activity:
You may need to rest until your heart rhythm is under control. Your healthcare provider will tell you when it is okay to get out of bed. Tell your healthcare provider before your get up for the first time. If you ever feel weak or dizzy, sit or lie down right away.
Medicines:
Healthcare providers may give you heart medicine to help control your heart rate or rhythm. You may need more than one medicine to treat your symptoms.
Tests:
- An EKG is a test to record your heart rhythm and how fast your heart beats. It is used to check for problems with your heart. Your healthcare provider may do an EKG when you are resting, then again after you exercise.
- A chest x-ray shows a picture of your heart and lungs.
- An echocardiogram is a type of ultrasound. Sound waves are used to show the structure and function of your heart.
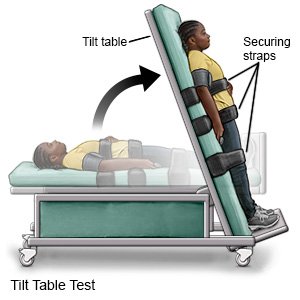
- A tilt table test checks your heart and blood pressure when your body changes positions.
- An electrophysiology study is a procedure to map the electrical pathways in your heart that control your heartbeat.
Treatment:
- You may need extra oxygen if your blood oxygen level is lower than it should be. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils. Ask your healthcare provider before you take off the mask or oxygen tubing.
- Vagal maneuvers are ways to use your own body to slow down your heart rate. Your healthcare provider may have bear down like you are having a bowel movement.
- Carotid sinus massage is a type of massage to help slow your heart rate. Your healthcare provider will apply steady pressure to a blood vessel on one side of your neck. Do not do a carotid sinus massage on yourself or anyone else.
- Cardioversion is a procedure to return your heart rate and rhythm to normal. It can be done with medicine or an electric shock. You may need cardioversion if medicine does not work.
- Ablation is a procedure that uses a catheter to damage the small area of your heart that is causing abnormal electrical signals. This will stop the electrical problem and allow your heart to beat regularly.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
RISKS:
SVT may cause heart failure.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Supraventricular Tachycardia
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
