Self Care Measures after a Stroke
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
Self-care measures are ways to help yourself manage the physical, mental, and emotional effects of a stroke. The effects of a stroke depend on where the stroke happened in your brain and how much damage occurred. You will learn self-care measures during stroke rehabilitation (rehab) sessions. Rehab is a program run by specialists who will help you recover abilities you may have lost. Specialists include physical, occupational, and speech therapists. They will help you develop a plan to care for yourself at home and at work.
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
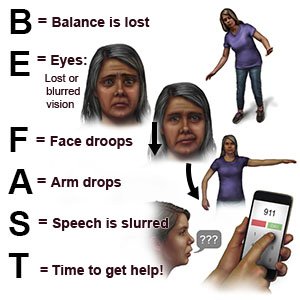
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have trouble breathing.
- You have a seizure.
Return to the emergency department if:
- You fall and hit your head or get injured.
- You have new symptoms, or your symptoms are getting worse.
- You have pain that does not go away, even after you take pain medicine.
Call your doctor or neurologist if:
- You feel depressed or anxious.
- You have a sore on your skin that does not go away.
- You have questions or concerns about your condition or care.
Manage physical effects:
You may have balance or walking problems. You may have numb areas or trouble moving your arm or leg. You may have weak muscles, spasms, or contractures (muscles stay in one position).
- Take your medicines as directed. Medicines will help you manage pain and problems with movement.
- Stretch and do range of motion exercises to prevent a contracture. Contractures limit movement of a joint, such as your wrist, elbow, shoulder, or ankle. Contractures can start to develop as soon as 1 week after your stroke. Your healthcare provider may show you or your caregiver how to stretch and do ROM exercises.
- Prevent falls. Remove objects from walkways in and around your home. Install devices to prevent falls, such as handrails or a raised toilet seat. Use assistive devices when you walk, such as a cane or walker. Wear nonslip shoes or socks at all times.

Manage mental effects:
You may have trouble paying attention, thinking clearly, or remembering facts. You may lose track of the date or not know where you are. It may be hard to find a familiar object.
- Calendars and planners can help you remember events and important dates. A calendar on an electronic device can be programed to alert you about an upcoming event. You may want to use a paper calendar so you can cross off days or circle important events.
- A medicine organizer can help you remember to take your medicine each day. Organizers can also blink or sound an alarm when it is time to take the medicine. Someone may need to help you program the organizer to remind you at certain times of the day.
- Lists can help you remember events or activities you need to do each day. Choose a kind of list that makes it easy for you to add new items and delete or cross off items that are done. It may help to put a list in a place you will see it often. An example is on the refrigerator. You may want to keep lists on a computer, tablet, smart phone, or other electronic device.
- Timers can help you remember to do a task, such as brushing your teeth.
- Labels can help you recognize items and remind you what they are for. Labels can include words or pictures.
Manage emotional effects:
You may have trouble controlling emotions after the stroke. This may be caused by damage to the brain. It may also be caused by the loss of body functions or independence. Depression is common after a stroke. You may also feel sad, irritable, or hopeless. You may have anger, frustration, or anxiety. Your moods may change quickly. You may laugh or cry, even if it is not the right emotion.
- Therapy or counseling may help you manage depression or anxiety after a stroke. Therapy or counseling may also help you control emotional outbursts or inappropriate emotions. Ask your healthcare provider how you can receive therapy or counseling.
- Medicine may be needed to treat depression, anxiety, or problems controlling your emotions.
- Support groups will allow you to talk about your feelings and concerns with others who have had a stroke. It may be helpful to hear from others who have gone through stroke rehab. You may learn ways to cope with your feelings and emotions.
- Talk to your healthcare provider if you have depression that continues or is getting worse. Your provider may be able to help treat your depression. It may also help to talk to friends and family members about how you are feeling. Tell your family and friends to let your healthcare provider know if they see any signs of depression:
- Extreme sadness
- Avoiding social interaction with family or friends
- A lack of interest in things you once enjoyed
- Irritability
- Trouble sleeping
- Low energy levels
- A change in eating habits or sudden weight gain or loss
Manage bladder or bowel problems:
A stroke can make it hard to control when you urinate or have a bowel movement. You may feel like you have to urinate even when your bladder is empty. You may have constipation or trouble emptying your bladder.
- Bladder and bowel movement training helps you control when you urinate and plan for bowel movements. This training can help your skin stay clean and dry, and help prevent skin breakdown. Your program may include using the bathroom at certain times each day, even if you do not feel the need.
- Medicines can help prevent urine leakage. Medicines such as stool softeners can help prevent or treat constipation. Some medicines are available without a prescription.
Manage energy and sleep problems:
You may feel tired during the day. You may not have the energy to do activities or spend time with others. It may be hard to fall asleep at night or to stay asleep.
- Talk to your healthcare provider about your medicines. Some medicines can make you feel tired or groggy. Your provider may make changes to your medicine or when you take it.
- Work with healthcare providers to create an exercise plan. Exercise can help increase your energy level during the day. Exercise can also help you sleep better at night. A short nap during the day can also help you manage fatigue.
- Schedule rest periods. You may need to rest after exercise or other activities. A short nap can help increase your energy. A nap can be for 15 to 30 minutes during the day. Do not nap for longer than 1 hour. Long naps can make it harder to fall asleep at night.
- Create a sleep schedule. Go to bed and wake up at the same times each day. This will help you develop healthy sleep patterns. Do activities that help you relax before bed. Read a book, take a warm bath, or listen to music.
- Limit liquids for 2 hours before bed. This helps prevent nighttime waking to empty your bladder. You may need to stop having caffeine in the afternoon if it affects your sleep.
- Talk to your healthcare provider about sleep apnea. This is a condition that causes you to stop breathing for 10 seconds or more while you are sleeping. A stroke increase your risk for sleep apnea. Treatment can also lower your risk for another stroke.
Follow up with your doctor or neurologist as directed:
Write down your questions so you remember to ask them during your visits.
For support and more information:
- American Stroke Association
Phone: 1- 888 - 478-7653
Web Address: http://www.stroke.org
© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Self Care Measures after a Stroke
Treatment options
Care guides
- AIDS
- HIV Infection
- Intracerebral Hemorrhage
- Leg Exercises for ACL Injury
- Pulmonary Rehabilitation
- Self Care Measures after a Stroke
- Self Care Measures with Cancer
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
