Revision Total Joint Arthroplasty
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
Revision total joint arthroplasty is surgery to fix or replace an artificial joint. You may need a revision arthroplasty if your artificial joint becomes loose, moves out of place, or breaks. You may need this surgery if the bone around your artificial joint gets weak or damaged over time. You may also need this surgery if you have severe pain or an infection in your joint.
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) for any of the following:
- You suddenly feel lightheaded and short of breath.
- You have chest pain when you take a deep breath or cough.
- You cough up blood.
Seek care immediately if:
- Blood soaks through your bandage.
- Your stitches come apart.
- Your wound is red, swollen, and draining pus.
- Your leg feels warm, tender, and painful. It may look swollen and red.
Call your orthopedist or surgeon if:
- You have a fever or chills.
- You have a cough, or you feel weak and achy.
- You have more pain and swelling, even after treatment.
- Your skin is itchy and swollen or you have a rash.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Antibiotics help prevent or treat an infection caused by bacteria.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for the surgery area as directed:
Do not let the area get wet until your surgeon tells you it is okay. Then take showers instead of baths. Cover the surgery area when you shower. Gently pat the area dry and put on new, clean bandages as directed. Change your bandages when they get wet or dirty. Do not swim or soak in a hot tub or bath tub until your surgeon says it is okay.
Go to physical therapy, if directed:
A physical therapist teaches you exercises to help improve movement and strength, and to decrease pain.
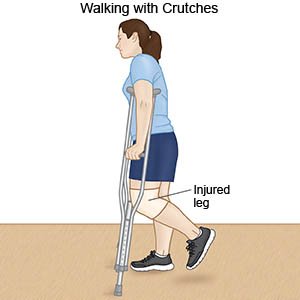
Use crutches, a cane, or a walker as directed:
These devices help you move around easier and may prevent a fall.
 |
Follow up with your orthopedist or surgeon as directed:
You may need to return to have your wound checked and stitches removed. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
