RSV (Respiratory Syncytial Virus) Infection in Children
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
Respiratory syncytial virus (RSV) causes infection in your child's lungs and airways. The small airways become swollen and filled with fluid and mucus. This may make it hard for your child to breathe. This virus is the most common cause of lung infections in infants and young children. Most children have had the virus by age 2 years. RSV infection is most common from fall through spring. An RSV infection may lead to other lung problems, such as pneumonia or bronchiolitis.
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that your child may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your child's medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done to your child. Make sure all of your questions are answered.
Stay with your child for comfort and support
as often as possible while he or she is in the hospital. Ask another family member or someone close to the family to stay with your child when you cannot be there. Bring items from home that will comfort your child, such as a favorite blanket or toy.
Isolation safety measures
may be used if your child has an infection that can be passed from person to person. Healthcare providers and visitors may need to wear gloves, a face mask, or a gown. Visitors should wash their hands before leaving to keep from spreading germs.
An IV
is a small tube placed in your child's vein that is used to give medicine or liquids.
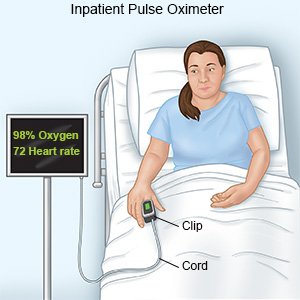
A pulse oximeter
measures how much oxygen is in your child's blood. A small clip or sticky strip will be placed on your child's finger, ear, or toe. A cord connects the oximeter to a machine. Do not remove the clip or sticky strip.
 |
Medicines:
- Antiviral medicine may be given to help decrease your child's symptoms.
- Acetaminophen may be given to decrease your child's pain and fever.
- Medicine to open your child's airway may be given. This medicine will decrease wheezing and make it easier for your child to breathe. The medicine is mixed with air or oxygen in a machine to change it into a mist. The mist makes it easier for your child to breathe the medicine into his or her lungs. The mist can be inhaled through a mouthpiece or mask.
Tests:
- Blood tests may be used to monitor your child's condition.
- A swab of the inside of your child's nose may show the infection. Providers may suction drainage from your child's nose. These samples are tested for infection.
- An x-ray may show fluid or swelling in your child's lungs.
Treatment:
- IV fluids may be given to treat or prevent dehydration.
- Oxygen may be needed if your child's blood oxygen level is lower than it should be. Your child may get oxygen through small tubes placed in his or her nostrils. Ask your child's healthcare provider before you take off the mask or oxygen tubing.
- Removal of mucus may be done by placing a small tube into your child's mouth or nose. This may help your child breathe easier. Saline drops may be put into your child's nose to help loosen the mucus. Your child may need this treatment more than 1 time.
RISKS:
Your child can get an RSV infection more than 1 time. An RSV infection may make it hard for your child to breathe. Your child may have trouble breastfeeding or bottle feeding. Your child may become dehydrated. Your child may need to stay in the intensive care unit (ICU) if the condition becomes severe. A young baby may develop an airway obstruction and need to stay in the ICU.
CARE AGREEMENT:
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about RSV Infection
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
