Pressure Injury
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is a pressure injury?
A pressure injury is an injury to the skin and tissue under the skin. A pressure injury is also called a pressure sore, bedsore, wound, or decubitus ulcer. Pressure injuries can form over any area but are most common on the back, buttocks, hips, and heels. Pressure injuries can also happen in your mouth.
What causes pressure injuries?
- Continuous pressure builds when you sit or lie on an area for too long. Continuous pressure also builds when medical equipment such as oxygen or IV tubing stays in one place too long. Pressure slows or stops the blood from flowing to the skin. This may hurt the skin and cause tissue damage. Pressure can start to cause damage to your skin and tissue about 2 hours after staying in the same position.
- Shearing or friction happens when delicate skin is dragged across a surface, such as sheets. This may cause your skin to tear or a blister to form. Sliding up or down in bed or moving from the bed to a chair may tear your skin. Muscle spasms may cause your arms or legs to jerk and rub the sheets, causing tears in your skin.
What increases my risk for a pressure injury?
- Long periods of time in one position
- Medical equipment, such as IV lines and tubing, in one position too long
- Short periods of increased pressure, such as sitting in a wheelchair
- Not being able to control your urine or bowel movements
- Dehydration or poor nutrition
- Numbness
- Poor blood flow to your limbs
- Age over 65 years
- Previous pressure injury
What are the stages of a pressure injury?
- With a deep tissue injury , your skin is not broken. You may see purple or red skin, or a blister. Your skin may feel warm, spongy, or tight when you touch it.
- At stage 1 , your skin is not broken, but it may itch or hurt. Your skin may feel warm, spongy, or tight when you touch it. The skin may stay red for more than an hour after pressure is removed from the bony area.
- At stage 2 , the skin has broken. You may have an open sore and the area around it may be red and raw. Your skin may sink inward and look shiny or dry.
- At stage 3 , the tissue below your skin is damaged. The area looks like a deep crater, or bowl-shaped hole. There may be more damage hidden under the skin than what you can see.
- At stage 4 , the sore is very deep and your tendons, muscle, and bone may be damaged. You may be able to see the tendons, muscle, and bone in the wound.
- With an unstageable wound , it is hard for healthcare providers to see what stage your pressure injury is in. This is usually because there is a lot of dead tissue or scabbing in the injury.
How is a pressure injury diagnosed?
Your healthcare provider will ask about your pressure injury and examine you. Tell him or her when your pressure injury started and if it is getting bigger or changing color. He or she may ask if you have pain or numbness over any bony areas. Tell him or her how you care for your skin at home. You may need a sample of tissue or fluid, blood tests, or an MRI to check for infection. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
How is a pressure injury treated?
You may need any of the following treatments depending on the stage of your pressure injury:
- Bandages may be need to protect your skin or injury. Your healthcare provider will choose the best bandage for your injury. Bandage changes may include cleaning the area with saline (saltwater). If your injury is deep, gauze that is wet with saline may be used to fill it. This is called packing the wound. A clean, dry dressing is placed over the packed wound to keep the skin dry. When the gauze dries, it is taken out and replaced with fresh, wet gauze.
- Medicines may be given to decrease pain or to help treat or prevent a bacterial infection. Ask how to take these medicines safely.
- Debridement is a procedure used to clean out dead tissue from a serious injury. Dead tissue may keep it from healing. Debridement allows healthy tissue to form so your injury can heal.
- Negative pressure wound therapy (NPWT) uses a machine called a wound vac, wound vacuum, or pump to help with wound healing. Suction from the machine removes drainage from your injury and pulls the edges closer together. NPWT promotes healthy tissue growth by increasing blood flow to the injury. NPWT also reduces bacteria that cause infections.
- Surgery may be needed to close your injury. This is called a flap closure. A skin flap (piece of skin) is usually taken from an area close to the injury. One end of the skin flap often remains attached while the other end is moved to cover your injury. The skin flap is secured with stitches or staples.
What can I do to manage my condition?
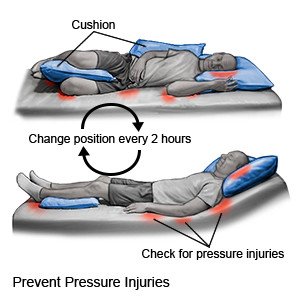 |
- Change your position often. Change your position every 2 hours if you are in a bed all day. Change your position every hour if you are in a wheelchair all day. Set an alarm to help remind you when it is time to turn. Keep a written turning schedule to help you remember to turn. If you are helping a person move in bed, lift him or her. Do not slide him or her. Keep the head of the bed as low as possible. This may help prevent damage to the skin from sliding down in bed.
- Protect your skin from tubes and medical devices, such as oxygen. Use a dressing to cushion the areas of skin where tubing or devices may be laid. Move the tubing or device and look at the skin every day. You may need to remove or move the tubing or device to another place.
- Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, and fish. Foods that are high in protein may help your pressure injury heal. This includes lean meats, beans, milk, yogurt, and cheese. Nutrition shakes may also give you extra calories and protein if you have trouble eating or are underweight.

- Do not smoke. Nicotine can damage your skin and slow wound healing. Do not use e-cigarettes or smokeless tobacco in place of cigarettes or to help you quit. They still contain nicotine. Ask your healthcare provider for information if you currently smoke and need help to quit.
How do I care for my skin?
- Clean and cover your injury. You may need to keep a bandage over your injury to protect the skin from more damage. You may also need to clean it with saline. Ask your healthcare provider for more information about when and how to change your bandages.
- Keep your skin clean, dry, and moisturized. Use mild soap and warm water to clean your skin. Do not rub or scrub when you wash. Do not use products that contain alcohol, because they can dry out your skin. Gently pat your skin dry. Do not rub your skin with a towel. Apply lotion or a moisturizer on your skin often.
- Protect the skin over bony areas. Use pillows or foam wedges to keep bony areas from touching, and to relieve pressure. For example, put a pillow or foam wedge between your knees to keep them from pressing on one another. Place a pillow or foam wedge under you to keep your hip raised when you lie on your side. Do not rest directly on your hipbone. Put a foam pad or pillow under your legs from calf to ankle when you lie on your back. The pad or pillow should raise your heels so that they are not touching the bed.
- Use specialty equipment, mattresses, or pads to decrease pressure. A draw sheet or large pad under you may help others move you up in bed. An overhead trapeze can help you change positions in bed. Mattresses and overlays made to provide more cushioning may help decrease the risk of pressure injuries. Examples include a foam mattress pad and air or water mattresses. Ask about equipment that may be right for you and how you use it.
When should I call my doctor or specialist?
- You have a fever.
- You have green or yellow drainage or a bad smell coming from your pressure injury.
- An area of your skin is very red and firm.
- You have new pain, or pain that is getting worse.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
