Peripheral Vascular Disease
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
Peripheral vascular disease (PVD) is a condition that causes decreased blood flow to your limbs because of blocked blood vessels. The blockage is usually caused by material such as cholesterol or a blood clot that sticks to the blood vessels and makes them narrow.
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) for any of the following:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
Return to the emergency department if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have leg pain that does not go away with rest.
- You have dark areas on the skin of your legs.
- You cannot see out of one or both eyes.
Call your doctor if:
- Your signs and symptoms get worse or do not get better, even after treatment.
- You have a sore or ulcer that is not healing or gets worse.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Cholesterol medicine helps decrease the amount of cholesterol in your blood.
- Antiplatelets help prevent blood clots. This medicine makes it more likely for you to bleed or bruise.
- Vasodilators help blood vessels dilate (open wider) and increase your blood flow.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Manage PVD:
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can damage your blood vessels. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Exercise as directed. Your healthcare provider can help you create a safe exercise plan. He or she may recommend walking. Walking is a low-impact way to exercise and increase your blood flow. Stop and rest if you have pain in your legs.
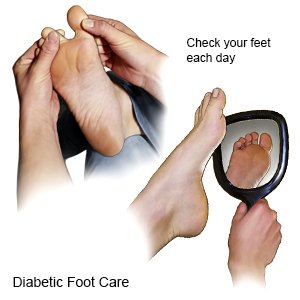
- Care for your feet. Look closely at your feet every day. Check for cracks or sores. Wash your feet daily with mild soap and dry them well. Do not walk barefoot in case you step on a hard or sharp object.
- Change your sleep position. You may have pain in your legs or feet when you sleep. Raise the head of your bed 4 inches, or use pillows to prop your upper body higher than your legs. This may help more blood go to your feet, decreasing pain.
- Protect and cushion your feet and hands. If you have ulcers on your feet, you may need to wear bandages with heel pads. You may also wear foam rubber booties. Hand or foot warmers may decrease pain in your hands or feet.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Prevent PVD:
- Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Ask if you need to be on a special diet.
- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. Ask him or her to help you create a weight loss plan if you are overweight.
- Manage diabetes. Keep your blood sugar level in the range recommended by your healthcare provider. Check your blood sugar level as often as directed. Ask your provider if you should make nutrition, exercise, or medicine changes.

Follow up with your doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Peripheral Vascular Disease
Treatment options
- Medications for Peripheral Arterial Disease
- Medications for Renal Artery Atherosclerosis
- Medications for Thromboangiitis Obliterans
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
