Peripheral Vascular Stent Placement
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
What do I need to know about a peripheral vascular stent placement?
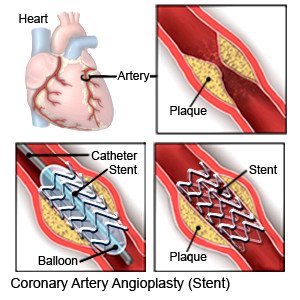
A peripheral vascular stent placement is a procedure to widen a narrowed artery in your leg or arm. A stent is a wire mesh tube that helps hold your artery open. Some stents have medicine that helps prevent blockages in your artery.
How do I prepare for a peripheral vascular stent placement?
- Your healthcare provider will tell you how to prepare for your procedure. Your provider may tell you not to eat or drink anything after midnight on the day of your procedure. Arrange to have someone drive you home when you leave the hospital.
- Tell your provider about all your current medicines. Your provider will tell you if you need to stop any medicine for the procedure and when to stop. Your provider will tell you which medicines to take or not take on the day of your procedure.
- You may be given an antibiotic to help prevent a bacterial infection. Contrast liquid may be used during your procedure. Tell your provider if you have ever had an allergic reaction to antibiotics or contrast liquid.
- You may need blood tests and a stress test before your procedure. Talk to your provider about these or other tests you may need.
What will happen during a peripheral vascular stent placement?
- You may be given general anesthesia to keep you asleep and free from pain during your procedure. You may instead be given IV sedation to make you feel calm and relaxed during the procedure. You may also be given local anesthesia to numb the area. With local anesthesia, you may still feel pressure or pushing but you should not feel any pain.
- Your healthcare provider will insert a catheter and wire into a blood vessel in your groin, arm, or wrist. Your provider will move a wire through the catheter and up into your blocked artery. Contrast liquid may be used to help your provider see your artery more clearly on the x-ray. You may feel warm when the contrast liquid is injected. Your provider may use a balloon to help open your artery. A stent will be inserted through the catheter and into your artery.
- Your provider will remove the catheter and wire. Clamps, stitches, or other devices may be used to close the catheter site. Pressure will be applied to the site for several minutes to stop any bleeding. A pressure bandage or other pressure device may be placed over the site to help prevent more bleeding.
What should I expect after a peripheral vascular stent placement?
- You will be attached to a heart monitor until you are fully awake. A heart monitor is an EKG that stays on continuously to record your heart's electrical activity. Healthcare providers will monitor your vital signs and pulses in your arm or leg. They will check your pressure bandage for bleeding or swelling. You may be able to go home or you may need to spend a night in the hospital.
- You will need to lie flat with your leg or arm straight for 2 to 4 hours. Do not get out of bed until your healthcare provider says it is okay. Arm or leg movements can cause serious bleeding. If you need to cough, support the catheter site with your hand.
What are the risks of a peripheral vascular stent placement?
You may bleed more than expected or get an infection. You may have bruising or pain where the catheter was. You may need surgery to repair damage from the catheter to your blood vessels or to stop heavy bleeding. You may get a blood clot in your arm or leg. The blood clot may break off and travel to your lungs, heart, or brain. This may cause a heart attack or stroke. The contrast liquid may cause kidney damage or an allergic reaction.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
