Patellar Tendon Repair
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about patellar tendon repair?
Patellar tendon repair is surgery to fix your torn patellar tendon. The patellar tendon attaches the bottom of your kneecap to your shin bone. The tendon works together with your muscles and ligaments to bend and extend your leg.
How do I prepare for surgery?
- Your surgeon will tell you how to prepare. He or she may tell you not to eat or drink anything after midnight before surgery. Arrange to have someone drive you home after surgery.
- Your surgeon will tell you if you need to stop any medicine for surgery, and when to stop. He or she will tell you which medicines to take or not take on the day of surgery.
- Tell your surgeon about any allergies you have. Tell him or her if you had an allergic reaction to anesthesia or any medicine.
- You may need blood or urine tests before your surgery. You may also need x-rays, a CT scan, or an MRI of your knee. Talk to your healthcare provider about these or other tests you may need. Write down the date, time, and location for each test.
What will happen during surgery?
- An incision will be made in the front of your knee. Your surgeon will find the torn ends of the tendon and trim them. He or she will sew the ends back together. If the tendon is not attached to bone, your surgeon will drill small holes in the end of your thigh bone. He or she will sew stitches onto the tendon, insert the stitches through the holes, and tie them. A tendon from another part of your body may be used. This tendon may be added to your patellar tendon so it reaches the bone where it will be attached. Wires or medical tape will also be passed through the drilled holes to add strength to the tendon.
- If a large piece of bone broke off with the tendon during the injury, it may be reattached with screws. Your surgeon will compare your knees to make sure the repaired knee is in the correct position. The incision will be closed with stitches and wrapped with a bandage. A brace, splint, or cast will be placed on your knee to keep it from moving while it heals.
What should I expect after surgery?
- Medicines may be given to prevent or treat pain, nausea, or a bacterial infection.
- You will be helped to walk around after surgery. Movement will help prevent blood clots.
- You may need physical therapy. A physical therapist teaches you exercises to help improve movement and strength and to decrease pain. Physical therapy may begin while you are in the hospital and continue when you get home.
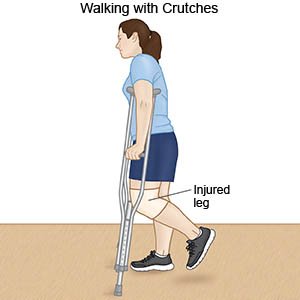
- You may need to use crutches or a cane so you do not put any weight on your knee. Your healthcare provider will tell you when you can walk on your injured leg again.
What are the risks of patellar tendon repair?
You may bleed more than expected or get an infection. Your knee function may not return to the way it was before surgery. You may get a blood clot in your leg. This may become life-threatening.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
