Mitral Valve Open Commissurotomy
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
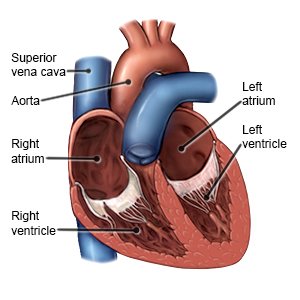
Mitral valve open commissurotomy is surgery to repair the mitral valve in your heart. The mitral valve normally opens and closes to let blood pass through the heart. If the valve does not open or close correctly, blood may not flow well through your heart.
 |
WHILE YOU ARE HERE:
Before your surgery:
- Informed consent is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
- An arterial line is a tube placed into an artery (blood vessel), usually in the wrist or groin. The line may be used for measuring your blood pressure or for taking blood.
- A CVP line is also called a central line. It is put into a large blood vessel near your collarbone, in your neck, or in your groin. The CVP line may be used to give medicines or IV fluids. It may also be hooked up to a monitor to take pressure readings. This information helps healthcare providers check your heart.
- General anesthesia will keep you asleep and free from pain during surgery. Anesthesia may be given through your IV. You may instead breathe it in through a mask or a tube placed down your throat. The tube may cause you to have a sore throat when you wake up.
During your surgery:
- Your surgeon will make an incision in the middle of your chest. You will be connected to a heart-lung bypass machine. This machine does the work of your heart and lungs during surgery. The valve will be repaired. Then your heart will be checked for bleeding. Wires may be put in your chest to improve your heartbeat. The wires will stay there in for a short time after surgery. The bypass machine will be removed, and your own heart and lungs will start working again.
- A transesophageal echocardiogram (TEE) will be done to see how well the valve and your heart are working. The incision in your chest will be closed with stitches or staples and covered with a bandage. The bandage keeps the area clean and dry to prevent infection.
After surgery:
You will be taken to the recovery room or an intensive care unit (ICU). Healthcare providers will watch you very closely. A healthcare provider may remove the bandage shortly after surgery to check the incision. Do not get out of bed until your healthcare provider says it is okay.
- Your blood oxygen and carbon dioxide levels will be checked. The results can tell healthcare providers how well your lungs are working.
- A chest tube will remove air, blood, or fluid from around your lungs or heart. The chest tube is attached to a container to collect the blood or fluid. You may need more than one chest tube.
- A temporary pacemaker may be placed for a short time. This is a machine that helps your heart beat at a normal speed and in a regular rhythm.
- Take deep breaths and cough 10 times each hour. This will decrease your risk for a lung infection. Take a deep breath and hold it for as long as you can. Let the air out and then cough strongly. Deep breaths help open your airway. You may be given an incentive spirometer to help you take deep breaths. Put the plastic piece in your mouth and take a slow, deep breath, then let the air out and cough. Repeat these steps 10 times every hour.
- Drains may be placed in the surgery area. Drains remove extra fluid or blood from the area.
- A Foley catheter is a tube put into your bladder to drain urine into a bag. Keep the bag below your waist. This will prevent urine from flowing back into your bladder and causing an infection or other problems. Also, keep the tube free of kinks so the urine will drain properly. Do not pull on the catheter. This can cause pain and bleeding, and may cause the catheter to come out.
- Intake and output may be measured. Healthcare providers will keep track of the amount of liquid you are getting. They also may need to know how much you are urinating. Ask healthcare providers if they need to measure or collect your urine.
- Help prevent blood clots. Move your legs, ankles, and feet as directed while you are in bed. Pressure stockings (long, tight stockings) are used to put pressure on your legs. Pressure increases blood flow and prevents clots. You may be asked to stand the same day of your surgery. You may start to walk the day after your surgery. If you feel weak or dizzy, sit or lie down right away.
- Medicines:
- Blood pressure medicine lowers your blood pressure.
- Blood thinners help prevent blood clots from forming. Your risk for bleeding and bruising is higher while you are taking blood thinners.
- Diuretics decrease edema (excess fluid) that collects in a part of your body, such as your legs. Diuretics can also remove excess fluid from around your heart or lungs and decrease your blood pressure. It is often called water pills. You may urinate more often when you take this medicine.
- Heart medicine helps strengthen or regulate your heartbeat.
- Antinausea medicine may be given to calm your stomach and to help prevent vomiting.
- Pain medicine may be given. Do not wait until the pain is severe before you ask for more medicine.
- Stool softeners make it easier for you to have a bowel movement. You may need this medicine to treat or prevent constipation.
- Antibiotics may be given to help prevent or treat a bacterial infection.
- Oxygen and a ventilator may be needed for a short time. You may need this when you wake up and for a day or two after surgery.
RISKS:
You may bleed, develop an infection, or have trouble breathing during or after surgery. Air bubbles in your blood could cause a stroke. The muscles or other valves in the heart could be damaged. You may have problems with your heartbeat or have a heart attack. Your kidneys may stop working and you may need dialysis. You may get a blood clot in your arm or leg. The clot may travel to your heart or brain and cause life-threatening problems, such as a heart attack or stroke.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
