Minimally Invasive Maze Procedure
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
A minimally invasive maze procedure is used to treat atrial fibrillation.
 |
WHILE YOU ARE HERE:
Before your procedure:
- Informed consent is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
- An IV is a small tube placed in your vein that is used to give you medicine or liquids.
- Tests:
- Cardiac catheterization is a procedure done to find the cause of and treat a heart condition. A thin, bendable tube inserted into an arm, neck, or groin vein is moved into your heart. Your healthcare provider may use an x-ray to guide the tube to the right place. Contrast liquid may be put into your vein so the pictures show up better on a monitor.
- An EKG test records your heart rhythm and how fast your heart beats.
During your procedure:
- General anesthesia will be used to keep you asleep and free from pain during this procedure. A catheter (tube) will be threaded into your heart through a blood vessel in your chest, neck, arm, or leg. Another tube with a small ultrasound sensor on the end may also be moved down into your esophagus. This will allow your surgeon to see your heart clearly.
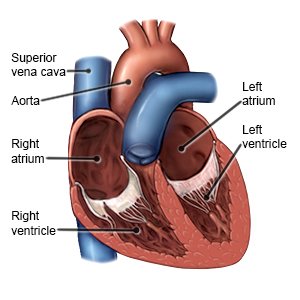
- Your surgeon will make a small incision in your chest to insert the endoscope through. Two smaller incisions will also be made between the ribs to insert the other instruments. Small incisions will be made in the right and left atria (upper chambers) of your heart and then sewn closed. This will form scar tissue and a maze where the impulses can travel in only 1 direction.
- The openings and incisions in your chest will be closed. A bandage will be placed over your incision to control bleeding.
After your procedure:
You will be taken to a room to rest until you are fully awake. Healthcare providers will monitor you closely for any problems. Do not get out of bed until your healthcare provider says it is okay. When your healthcare provider sees that you are okay, you will be able to go home or be taken to your hospital room. The catheter inserted for the procedure will be removed. A tight pressure bandage will cover the incision. A healthcare provider may remove the bandages soon after the procedure to check your wound.
- You will need to lie flat and still in bed for a few hours. Healthcare providers will help you roll from side to side. If an artery in your groin was used for the procedure, you must keep your leg straight. Do not bend it until your healthcare provider tells you it is okay. Your provider will also tell you when it is okay to get out of bed.
- A temporary pacemaker is a device that helps your heart beat at a normal speed and in a regular rhythm. It is connected to the wires that were put into your heart muscle during your procedure. The wires may then be connected to a small pacemaker outside of your body. You may need this pacemaker treatment for a short time.
- Medicines:
- Heart medicine is given to strengthen or regulate your heartbeat.
- Anticoagulants are used to help thin your blood to prevent blood clots. You may bleed or bruise more easily while you are taking this medicine.
- Diuretics help get rid of extra fluid that collects in a part of your body, such as your legs. Diuretics can also remove fluid from around your heart or lungs and lower your blood pressure. You may urinate more often when you take this medicine.
- Antibiotics help treat or prevent an infection caused by bacteria.
- Antinausea medicine helps calm your stomach and prevents vomiting.
- Pain medicine may be given. Tell healthcare providers right away if you start feeling discomfort, pressure, burning, or tightness in your chest. Tell providers right away if you start sweating, have trouble breathing, or feel discomfort in your arm, back, neck, or jaw. Any of these may be a sign that your heart is not getting enough oxygen, and may need medicine to help.
RISKS:
Problems may happen during this procedure that may lead to an open chest surgery. During this procedure, your heartbeat may stop. This may decrease blood flow more and lead to a heart attack. A blood vessel or your atria may get injured, causing a large amount of blood loss. You could also have trouble breathing, an infection, or bleed more than expected after this procedure. You may develop a life-threatening blood clot.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
