Microscopic Colitis
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
What is microscopic colitis?
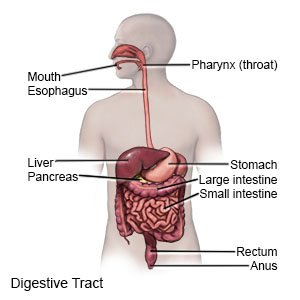
Microscopic colitis is long-term inflammation of your colon (large intestine). Inflammation can damage the lining of your colon and cause long-term diarrhea. Microscopic colitis may be caused by an infection, higher levels of acid in your colon, or the cause may not be known.
 |
What increases my risk for microscopic colitis?
- Older age
- Being female
- Increased bile acids
- Family history of microscopic colitis or another colon disease
- Bacterial infection
- Medicines for pain, depression, ulcers, or seizures
- Weakened immune system
What are the signs and symptoms of microscopic colitis?
- Diarrhea
- Abdominal pain
- Fatigue
- Nausea or vomiting
- Weight loss
- Loss of bowel movement control
- Dehydration (thirst, dry mouth, or decreased urine)
How is microscopic colitis diagnosed?
- Blood tests may show if you have an infection.
- A bowel movement sample may show what germ is causing your illness.
- A colonoscopy may show what is causing your colitis. A tube with a light and camera on the end will be put into your anus, and moved forward into your intestine.
How is microscopic colitis treated?
Medicines may be given to treat a bacterial infection, decrease inflammation in your colon, or treat diarrhea. You may also need medicine to decrease acid levels in your colon that could cause irritation.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I manage my symptoms?
- Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. You may need to eat several small meals throughout the day. Avoid spicy foods, caffeine, chocolate, and foods high in fat.
- Drink liquids as directed to help prevent dehydration. Good liquids to drink include water, juice, and broth. Ask how much liquid to drink each day. You may need to drink an oral rehydration solution (ORS). An ORS contains a balance of water, salt, and sugar to replace body fluids lost during diarrhea.
- Start to exercise when you feel better. Regular exercise helps your bowels work normally. Ask about the best exercise plan for you.
- Ask about probiotics. You may need supplements that help balance the bacteria in your colon. This may help decrease you symptoms.
How can I help prevent microscopic colitis?
- Wash your hands. Wash your hands in warm, soapy water for 20 seconds before and after you handle food. Wash your hands after you use the bathroom, change a diaper, or touch an animal.
- Clean food and areas that come in contact with food. Rinse fruits and vegetables in running water. Clean cutting boards, knives, countertops, and other areas where you prepare food before and after you cook. Wash sponges and dishtowels weekly in hot water.
- Cook food all the way through. Cook eggs until the yolks are firm. Use a meat thermometer to make sure meat is heated to a temperature that will kill bacteria. Do not eat raw or undercooked chicken, turkey, seafood, or meat.
- Store food properly. Refrigerate or freeze fruits and vegetables, cooked foods, and leftovers.
- Drink safe water. Drink only treated water. Do not drink water from ponds or lakes, or from swimming pools that do not contain chlorine. Drink bottled water when traveling.
Call 911 for any of the following:
- You have trouble breathing.
When should I seek immediate care?
- You have any of the following signs of severe dehydration:
- Dizziness or weakness
- Dry mouth, cracked lips, or severe thirst
- Fast heartbeat or breathing
- Passing little to no urine
- You have black or bright red stools.
- You have blood in your vomit.
- Your abdomen feels larger than normal, hard, and painful.
When should I contact my healthcare provider?
- You have a fever with abdominal pain that does not go away.
- You have a fever, chills, cough, or feel weak and achy.
- Your diarrhea gets worse.
- Your symptoms do not improve or get worse.
- You are losing weight without trying.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
