Lumbar Nerve Root Injection
Medically reviewed by Drugs.com. Last updated on Apr 2, 2024.
WHAT YOU NEED TO KNOW:
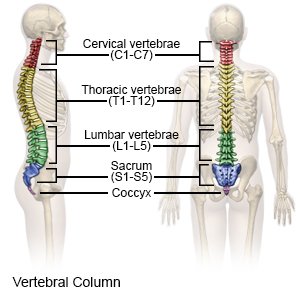
A lumbar nerve root injection is a procedure to inject medicines at the nerve roots of your lumbar (lower back) spine. This procedure is done to decrease inflammation and pain.
 |
HOW TO PREPARE:
The week before your procedure:
- Your healthcare provider will tell you how to prepare. Arrange to have someone drive you home after your procedure.
- Tell your provider about all the medicines you currently take. He or she will tell you if you need to stop any medicine before the procedure, and when to stop. He or she will tell you which medicines to take or not take on the day of the procedure. He or she will also talk to you about starting your usual pain medicine again after the procedure.
- Tell your provider about all your allergies. Tell him or her if you had an allergic reaction to anesthesia, antibiotics, or contrast liquid.
- You may need to have blood and urine tests. Tests such as x-rays, a CT scan, or an MRI may also be done.
The night before your procedure:
You may be told not to eat or drink anything after midnight.
The day of your procedure:
- Take only the medicines your healthcare provider told you to take.
- Healthcare providers may insert an intravenous tube (IV) into your vein. A vein in the arm is usually chosen. You may be given liquids or medicine through the IV.
- An anesthesiologist will give you medicine to make you sleepy before your procedure. Tell your healthcare provider if you or anyone in your family has had a problem using anesthesia in the past.
- You or a close family member will be asked to sign a legal document called a consent form. It gives healthcare providers permission to do the procedure or surgery. It also explains the problems that may happen, and your choices. Make sure all your questions are answered before you sign this form.
WHAT WILL HAPPEN:
What will happen:
- You will lie on your stomach, with your body slightly turned to the side. A pillow may be placed under your abdomen, or you may be asked to bend one or both knees.
- A thin needle will be inserted near your lumbar spine to the affected nerve root. Your healthcare provider will use an x-ray with contrast liquid or a CT scan to help guide the needle. He or she will place the needle tip near the nerve root. Your provider will inject medicines, such as steroids and anesthesia. After the procedure, the injection sites will be covered with bandages to keep the area clean and dry to prevent infection.
After your procedure:
You will be taken to a recovery room to rest. Healthcare providers will watch you closely for any problems. Do not get out of bed until your healthcare provider says it is okay. When healthcare providers see that you are okay, you may be able to go home.
- Bandages will cover the procedure area. The bandages keep the area clean and dry to prevent infection. A healthcare provider may remove the bandages soon after your procedure to check the injection sites.
- Medicines may be given to treat pain, swelling, or fever, or to prevent an infection.
CONTACT YOUR HEALTHCARE PROVIDER IF:
- You have a fever.
- You have a skin infection or an infected wound near your lower back.
- You have questions or concerns about your procedure.
Risks
You may get an infection or have bleeding. Other parts near your spine, such as nerves, blood vessels, ligaments, muscles, and bones, may be damaged. The medicines may spread in areas near the lumbar nerve root and cause numbness in these areas. You may still have leg or lower back pain.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
