Gastrectomy
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
What do I need to know about a gastrectomy?
A gastrectomy is surgery to remove part or all of your stomach.
 |
How do I prepare for surgery?
- Your surgeon will tell you how to prepare for surgery. You may be told not to eat or drink anything after midnight on the day of surgery. Arrange to have someone drive you home after surgery.
- Tell your surgeon about any allergies you have. Tell him or her if you have had an allergic reaction to anesthesia or antibiotics.
- Tell your surgeon about all medicines you currently take. He or she will tell you if you need to stop taking any medicine before surgery, and when to stop. He or she will tell you which medicines to take or not take on the day of surgery.
- You may need blood or urine tests before your surgery. You may also need x-rays, a CT scan, endoscopy, or ultrasound. Tissue samples may be taken and checked for cancer.
What will happen during surgery?
- You will be given general anesthesia to keep you asleep and free from pain during surgery. Antibiotics may be given to prevent an infection caused by bacteria.
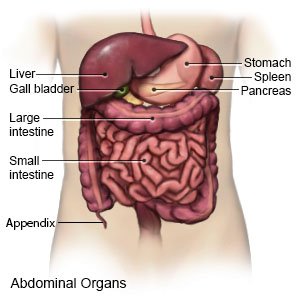
- For an open gastrectomy, an incision will be made on your abdomen. Your surgeon will remove part or all of your stomach. He or she will connect the remaining stomach or your esophagus to your small intestine.
- For a laparoscopic gastrectomy, your surgeon will make 3 to 5 small incisions on your abdomen. The laparoscope and other tools will be put through the incisions. Your surgeon may also make a larger incision on your abdomen to place a hand and tools inside your abdomen. Your abdomen will be filled with a gas so your surgeon can see your stomach more easily. He or she will remove part or all of your stomach. Your esophagus or remaining stomach will be connected to your small intestine.
- Drains may be placed in your incision to remove extra fluid from your abdomen. The incision will be closed with stitches or staples and covered with bandages.
What should I expect after surgery?
You may be taken to a recovery room to stay until you are fully awake. Healthcare providers will watch you closely for problems. Do not get out of bed until your healthcare provider says it is okay.
- You may need to walk around the same day of surgery, or the day after. Movement will help prevent blood clots. You may also be given exercises to do in bed.
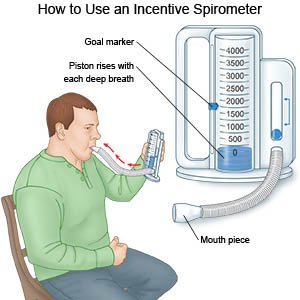
- Deep breathing and coughing will decrease your risk for a lung infection. Take a deep breath and hold it for as long as you can. Let the air out and then cough strongly. Deep breaths help open your airway. You may be given an incentive spirometer to help you take deep breaths. Put the plastic piece in your mouth and take a slow, deep breath. Then let the air out and cough. Repeat these steps 10 times every hour.
- Medicines may be given to relieve pain or to prevent nausea or a bacterial infection.
- A nasogastric (NG) tube may be put into your nose and down into your stomach during surgery. The NG tube helps prevent vomiting and may help get your intestines working. The NG tube is usually removed 1 day after surgery.
- You will be started on soft foods, such as applesauce, cottage cheese, and gelatin. Your healthcare providers will monitor how well you do with these foods. Providers will tell you when you can eat larger amounts of food or different types of food.
What are the risks of a gastrectomy?
- You may have leaking of stomach or bowel contents from your incisions and get a life-threatening infection. After surgery, you may not get enough nutrients. You may be able to only eat small amounts of food. You may have pain or feel full even after you eat only small amounts of food. Without some parts of your stomach, you may not get all the nutrients you need from your food. You may have dumping syndrome (diarrhea soon after you eat). You may get a blood clot in your arm or leg. This may become life-threatening.
- Even after surgery, tumors may return in your remaining stomach or in nearby organs and tissues. You may get a blood clot in your leg or arm. This may become life-threatening.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
