Acute Liver Failure
Medically reviewed by Drugs.com. Last updated on Apr 2, 2024.
What is acute liver failure?
Acute liver failure occurs when your liver is damaged and suddenly stops working properly. This may cause damage to other tissues or organs, such as your brain or kidneys. Acute liver failure can become life-threatening.
 |
What are the signs and symptoms of acute liver failure?
- Yellowing of your skin or whites of your eyes
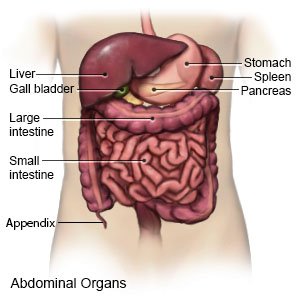
- Pain in the upper right side of your abdomen
- Itchy skin and a swollen abdomen, feet, and legs
- Changes in mood, confusion, or increased sleepiness
- Bleeding and bruising easily
- Dark bowel movements and decreased or dark urine
- Loss of appetite, nausea, and vomiting
- Fatigue (being mentally and physically tired) and weakness
What causes acute liver failure?
The exact cause of acute liver failure may not be known. Any of the following may increase your risk:
- Certain medicines, such as antiseizure medicines and some antibiotics
- An acetaminophen overdose or use of some herbal supplements
- Use of drugs such as cocaine
- A viral infection that causes hepatitis (inflammation of the liver)
- An autoimmune disease, such as rheumatoid arthritis
- Health conditions such as Wilson disease, heart failure, or Budd-Chiari syndrome
- HELLP syndrome during pregnancy
- Cancer that has spread to your liver from another body area
What do I need to know about health problems acute liver failure may cause?
- Encephalopathy occurs when harmful substances, such as ammonia, build up and cause brain damage.
- Bleeding problems may occur because your liver does not produce enough clotting factors. Clotting factors help your blood to clot.
- Heart and lung problems , such as hypotension (low blood pressure) and pulmonary edema may occur. Pulmonary edema is a buildup of fluid in the alveoli (air sacs) of your lungs. You may also get respiratory distress syndrome. This condition causes damage to the small blood vessels in your lungs.
- Infections , such as respiratory and urinary tract infections, may occur.
- Other health problems , such as kidney failure, hypoglycemia (decreased blood sugar level), and pancreatitis may occur. Pancreatitis is inflammation of the pancreas.
How is acute liver failure diagnosed?
Your healthcare provider will examine you. Your provider will ask if you have had any liver problems in the past. Tell your provider about your past and current medicines. Your provider will also check for other conditions that may be causing your symptoms. You may need any of the following:
- Blood tests show liver and kidney function. They may also show signs of infection. A blood test may also be done to check how quickly your blood clots. The level of acetaminophen in your blood will be checked if you had an overdose.
- A neurologic exam can show how well your brain works during your illness. Healthcare providers will check how your pupils (black dots in the center of each eye) react to light. Providers may check your memory and how easily you wake up.
- An ultrasound or CT may show signs of liver injury. You may be given contrast liquid to help your liver show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
- A liver biopsy is a procedure to remove a small piece of your liver. The sample is sent to a lab for tests.
How is acute liver failure treated?
Treatment depends on the cause of your acute liver failure, and other health problems caused by liver failure. The goal of treatment is to decrease damage to your liver and control your symptoms. You will need to stay in the hospital for treatment. If you have a pregnancy-related condition that caused liver failure, you may need to give birth early. You may need any of the following:
- Medicines may be given to decrease liver damage caused by an acetaminophen overdose. Antivirals help treat or prevent a viral infection. Antiviral medicine may also be given to control symptoms of a viral infection that cannot be cured. Steroids may be given to decrease inflammation. Medicines may be given to treat other health problems caused by acute liver failure. An example is medicine to decrease ammonia levels and treat encephalopathy.
- A liver transplant may be needed if your liver is badly damaged. All or part of your damaged liver is removed or replaced with a healthy liver from a donor.
What can I do to manage or prevent acute liver failure?
- Ask about medicines and supplements. Some medicines and supplements can harm your liver. Acetaminophen is an example. Talk to your healthcare provider about all your medicines. Do not take any over-the-counter medicine or herbal supplements unless your provider says it is okay.
- Do not drink alcohol. Alcohol will cause more damage to your liver.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause blood vessel and lung damage. Ask your provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
- Reach or maintain a healthy weight. Extra body weight increases the risk for fatty liver disease. Ask your provider what a healthy weight is for you. Your provider can help you create a safe weight loss plan, if needed.
- Slowly return to your activities. You may feel weak or get tired easily for several weeks. Slowly increase your activity every day. Take breaks and rest when you need it. You may need to avoid contact sports to prevent injury. You may bleed easily until your liver heals. Ask your provider which activities are safe for you to do.
Call your local emergency number (911 in the US) or have someone call if:
- You have a seizure.
- You lose consciousness or cannot be woken.
- You have sudden shortness of breath.
When should I seek immediate care?
- You feel lightheaded or are too weak to stand.
- You have shaking, chills, and a high fever.
- You have trouble thinking clearly, or you are confused.
- You urinate less than usual, have dark urine, or stop urinating.
- You vomit blood.
- You have blood in your bowel movements.
- You have severe abdominal pain.
- Your heart is beating faster than usual.
When should I call my doctor?
- You bruise or bleed easily.
- You have new or worse swelling in your legs, ankles, or feet.
- Your symptoms come back after treatment.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Acute Liver Failure
Treatment options
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
