Endocarditis
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is endocarditis?
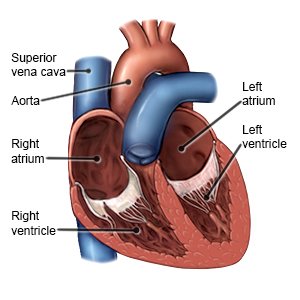
Endocarditis is an infection of the inner lining of your heart. It may also affect the valves of your heart. Endocarditis, and the health problems it may cause, can be serious and can become life-threatening.
 |
What causes endocarditis?
Some autoimmune disease, such as rheumatoid arthritis and cancer, can increase your risk for endocarditis. Your risk for endocarditis may also be increased if you have congenital heart disease. Endocarditis is most often caused by a bacterial infection. It may also be caused by viral, fungal, or parasitic infections. Bacteria or other germs may enter your bloodstream and get to your heart in the following ways:
- A heart surgery such as a valve replacement
- Dental procedures
- A urinary or IV catheter
- Skin, mouth, or intestinal sores
- Injecting illegal drugs
- An implanted device such as a pacemaker or defibrillator
What are the signs and symptoms of endocarditis?
- Fever
- Cough or shortness of breath
- Small red spots in your eye
- Red or painful spots on your hands
- Dark lines on your fingernails
- Headaches, body aches, or joint pain
- A fast or pounding heartbeat, or heart flutters
- Swelling in your legs, feet, or ankles
- Chest pain
How is endocarditis diagnosed?
Your healthcare provider will examine you and ask about your symptoms. Tell him or her if you have any medical conditions or take any medicines. You may need any of the following:
- Blood and urine tests may show if you have an infection or if another health condition is causing your symptoms.
- An EKG records your heart rhythm and how fast your heart beats. It is used to check for problems with your heart.
- An echocardiogram is an ultrasound used to find infection in your heart. Sound waves are used to show the structure and function of your heart. You may need a transthoracic or transesophageal echocardiogram. Ask your healthcare provider about these types of echocardiogram.
How is endocarditis treated?
You will need to be monitored and treated in a hospital. You may need any of the following:
- Medicines will be given to treat the infection. You may need medicine to strengthen your heart, decrease stress on your heart, or to remove extra fluid.
- Surgery may be needed to repair or replace a damaged heart valve. Surgery may also be needed to remove an implanted device that has caused the infection. This may include removal of a pacemaker or defibrillator.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What can I do to care for myself?
- Rest as directed. Some activities may make your symptoms worse. Ask your healthcare provider what activities are safe for you to do. Also ask when you can return to your normal activities.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can make it hard to heal from endocarditis. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
How can I help prevent endocarditis?
- Keep your teeth and gums healthy. Brush and floss your teeth 2 to 3 times every day. It is best to brush and floss after meals. Gently brush your teeth and gums with a clean toothbrush that has soft bristles. Go to the dentist every 6 months for checkups. Always tell your dentist that you have had endocarditis.
- Ask your healthcare provider if you should take antibiotics before certain procedures. Some procedures may allow bacteria to get into your blood and travel to your heart.
- Carry a wallet card that says you are at risk for endocarditis. This card will alert healthcare providers. It will also help them decide if you need antibiotics before a procedure or in an emergency. You can get this card through the American Heart Association.
- American Heart Association
7272 Greenville Avenue
Dallas , TX 75231-4596
Phone: 1- 800 - 242-8721
Web Address: http://www.heart.org
- American Heart Association
How can I help prevent the spread of germs?
 |
- Wash your hands often. Wash your hands several times each day. Wash after you use the bathroom, change a child's diaper, and before you prepare or eat food. Use soap and water every time. Rub your soapy hands together, lacing your fingers. Wash the front and back of your hands, and in between your fingers. Use the fingers of one hand to scrub under the fingernails of the other hand. Wash for at least 20 seconds. Rinse with warm, running water for several seconds. Then dry your hands with a clean towel or paper towel. Use hand sanitizer that contains alcohol if soap and water are not available. Do not touch your eyes, nose, or mouth without washing your hands first.

- Cover a sneeze or cough. Use a tissue that covers your mouth and nose. Throw the tissue away in a trash can right away. Use the bend of your arm if a tissue is not available. Then wash your hands well with soap and water or use a hand sanitizer. Do not stand close to anyone who is sneezing or coughing.
- Do not share items. Examples include eating utensils, drinks, and food.
- Ask about vaccines you may need. Vaccines help prevent some infections that cause disease. Get a yearly flu vaccine as soon as recommended, usually starting in September or October. Your healthcare provider can tell you other vaccines you should get, and when to get them.
Call your local emergency number (911 in the US) if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have sudden trouble breathing or shortness of breath while lying down.
- Your heart pounds or flutters, or your heart rate is faster than usual.
- You cough up blood.
When should I seek immediate care?
- You have a severe headache, stiff neck, and your eyes are sensitive to light.
- You have new or increased swelling in your feet or ankles.
- You feel faint.
When should I call my doctor?
- You have a fever.
- You lose your appetite or are unable to eat.
- You have increased fatigue and weakness.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Endocarditis
Treatment options
- Medications for Endocarditis
- Medications for Infectious Endocarditis
- Medications for Valvular Heart Disease
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
