Carbon Monoxide Poisoning
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is carbon monoxide (CO) poisoning?
CO poisoning is a life-threatening condition caused by exposure to high levels of CO. CO is a poisonous gas that you cannot see, taste, or smell. Exposure happens when you breathe in CO. CO can build up in your body and replace oxygen in your blood. Your brain, organs, and tissues can be damaged from a lack of oxygen. CO poisoning can be mild or severe. Severe poisoning can cause permanent injury.
Where is CO found?
- Smoke from a fire
- Faulty devices or equipment, such as a furnace, water heater, gas stove, or wood-burning stove or fireplace
- Gas-powered tools, vehicles, or machines used in poorly ventilated areas, such as a barbecue grill or chain saw
- Nonvented devices such as propane heaters, stoves, grills, or lanterns used inside a house, trailer, or tent
- Exhaust from cars or other vehicles
What increases my risk for CO poisoning?
- Older age
- Heart disease, blood vessel disease, sickle cell anemia, and lung problems
- Pregnancy
- Smoking cigarettes
- Work that uses equipment or chemicals that produce CO
What are the signs and symptoms of CO poisoning?
Signs and symptoms may develop right after CO exposure, or several weeks later. You may have any of the following:
- Blurred vision, dizziness, or a headache
- Nausea, vomiting, or loss of appetite
- Faster breathing than normal, or trouble breathing
- Weakness, muscle pain, or dark urine
- Chest pain, or a fast, strong, or irregular heartbeat
- Confusion, fainting, or seizures
- Tremors or shaking, or trouble moving, bending arms or legs, or walking
- Difficulty speaking, chewing, or controlling facial muscles
How is CO poisoning diagnosed?
Your healthcare provider will examine you and ask about your symptoms. Tell him or her if anyone in your home has similar signs and symptoms. Pets may also show similar signs. Tell him or her if you use home heating devices that burn gas, oil, wood, or other fuel. You may need blood tests to check the level of CO in your blood. Blood tests may also show problems caused by CO poisoning. Your breath may be tested for the amount of CO it contains. Your heart rhythm and brain function may also be monitored.
How is CO poisoning treated?
- Extra oxygen may be given if your blood oxygen level is lower than it should be. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils.
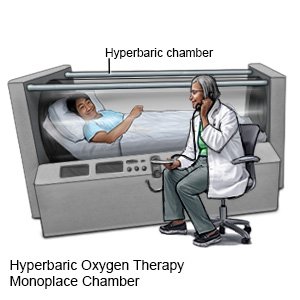
- Hyperbaric oxygen therapy is used to get more oxygen into your body. The oxygen is given under pressure to help it get into your tissues and blood.
What should I do if I think I or someone else was exposed to CO?
CO poisoning can seem like the flu. Anyone who may have been exposed to CO needs to be checked by a healthcare provider. The following are steps to take if you believe you or someone else is near a source of CO:
- Move into fresh air. If safely possible, shut off the source of the CO. Wait for a professional to help you if you cannot do this safely.
- Call 911. Explain when the exposure happened and how long you think it lasted.
- Start CPR if needed and you are trained on how to do this. CPR may be needed if the person is not breathing.
What can I do to prevent CO poisoning?
- Install a CO detector in every sleeping area in your home. Place it 5 feet above the floor and away from fireplaces or gas-burning equipment. Change the batteries twice each year.
- Check your chimney, furnace, or wood stoves. Check for problems every year before you use them. Have your fireplace flue cleaned on a regular basis.
- Be careful with gas appliances. Do not use barbecues or heaters that burn fuel inside your home or other closed spaces. Do not use your gas kitchen oven to heat your home. Make sure appliances are properly hooded or vented.
- Do not let motor vehicles run in closed areas. This includes letting your car run in a garage. If the car is outside, check that the exhaust pipe is not blocked.
- Do not smoke. Cigarette smoke contains small amounts of CO. This increases your risk of CO poisoning if you are exposed to a source of CO. Ask your healthcare provider for information if you need help quitting.
Call your local emergency number (911 in the US) if:
- You have chest pain or an irregular or fast heartbeat.
- You or someone close to you has a seizure or is unconscious.
- You have trouble breathing or are breathing faster than usual.
- You feel like you are going to faint.
- You feel weak, have trouble moving, or have severe muscle pain.
- Your urine becomes dark or red.
When should I call my doctor?
- You feel dizzy.
- You have a headache or start to vomit.
- Your eyesight becomes blurred.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Carbon Monoxide Poisoning
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
