Bronchiolitis
Medically reviewed by Drugs.com. Last updated on May 6, 2024.
Bronchiolitis causes the small airways to become swollen and filled with fluid and mucus. This makes it hard for your child to breathe. Bronchiolitis usually goes away on its own. Most children can be treated at home. Treatment is based on your child's symptoms. Medication is generally not needed.
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) for any of the following:
- Your child stops breathing.
- Your child has pauses in his or her breathing.
- Your child is grunting and has increased wheezing or noisy breathing.
Return to the emergency department if:
- Your child is 6 months or younger and takes more than 60 breaths in 1 minute.
- Your child is 6 to 11 months old and takes more than 50 breaths in 1 minute.
- Your child is 1 year or older and takes more than 40 breaths in 1 minute.
- Your child's nostrils become wider when he or she breathes in.
- Your child's skin, lips, fingernails, or toes are pale or blue.
- Your child's heart is beating faster than usual.
- Your child has any of the following signs of dehydration:
- Crying without tears
- Dry mouth or cracked lips
- More irritable or sleepy than usual
- Sunken soft spot on the top of the head, if he or she is younger than 1 year
- Having less wet diapers than usual, or urinating less than usual or not at all
- Your child's temperature reaches 105°F (40.6°C).
Call your child's doctor if:
- Your child is younger than 2 years and has a fever for more than 24 hours.
- Your child is 2 years or older and has a fever for more than 72 hours.
- Your child's nasal drainage is thick, yellow, green, or gray.
- Your child's symptoms do not get better, or they get worse.
- Your child is not eating, has nausea, or is vomiting.
- Your child is very tired or weak, or he or she is sleeping more than usual.
- You have questions or concerns about your child's condition or care.
Medicines:
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to give your child and how often to give it. Follow directions. Read the labels of all other medicines your child uses to see if they also contain acetaminophen, or ask your child's doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Do not give aspirin to children younger than 18 years. Your child could develop Reye syndrome if he or she has the flu or a fever and takes aspirin. Reye syndrome can cause life-threatening brain and liver damage. Check your child's medicine labels for aspirin or salicylates.
- Give your child's medicine as directed. Contact your child's healthcare provider if you think the medicine is not working as expected. Tell the provider if your child is allergic to any medicine. Keep a current list of the medicines, vitamins, and herbs your child takes. Include the amounts, and when, how, and why they are taken. Bring the list or the medicines in their containers to follow-up visits. Carry your child's medicine list with you in case of an emergency.
Manage your child's symptoms:
- Have your child rest. Rest can help your child's body fight the infection.
- Give your child plenty of liquids. Liquids will help thin and loosen mucus so your child can cough it up. Liquids will also keep your child hydrated. Do not give your child liquids with caffeine. Caffeine can increase your child's risk for dehydration. Liquids that help prevent dehydration include water, fruit juice, or broth. Ask your child's healthcare provider how much liquid to give your child each day. If you are breastfeeding, continue to breastfeed your baby. Breast milk helps your baby fight infection.
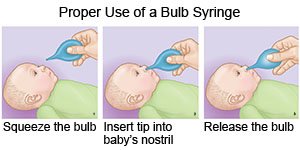
- Remove mucus from your child's nose. Do this before you feed your child so it is easier for him or her to drink and eat. You can also do this before your child sleeps. Place saline (saltwater) spray or drops into your child's nose to help remove mucus. Saline spray and drops are available over-the-counter. Follow directions on the spray or drops bottle. Have your child blow his or her nose after you use these products. Use a bulb syringe to help remove mucus from an infant or young child's nose. Ask your child's healthcare provider how to use a bulb syringe.
- Use a cool mist humidifier in your child's room. Cool mist can help thin mucus and make it easier for your child to breathe. Be sure to clean the humidifier as directed.
- Keep your child away from smoke. Do not smoke near your child. Nicotine and other chemicals in cigarettes and cigars can make your child's symptoms worse. Ask your child's healthcare provider for information if you currently smoke and need help to quit.
Prevent bronchiolitis:
- Wash your hands and your child's hands often. Wash hands several times each day. Wash after you use the bathroom, change a child's diaper, and before you prepare or eat food. Teach your child how to wash his or her hands. Use soap and water every time. Rub your soapy hands together, lacing your fingers. Wash the front and back of each hand, and in between all fingers. Use the fingers of one hand to scrub under the fingernails of the other hand. Wash for at least 20 seconds. Rinse with warm, running water for several seconds. Then dry your hands with a clean towel or paper towel. You and your older child can use hand sanitizer that contains alcohol if soap and water are not available. No one should touch his or her eyes, nose, or mouth without washing hands first.

- Clean toys and other objects with a disinfectant solution. Clean tables, counters, doorknobs, and cribs. Also clean toys that are shared with other children. Use a disinfecting wipe, a single-use sponge, or a cloth you can wash and reuse. Use disinfecting cleaners if you do not have wipes. You can create a disinfecting cleaner by mixing 1 part bleach with 10 parts water. Wash sheets and towels in hot, soapy water, and dry on high.
- Do not smoke near your child. Do not let others smoke near your child. Secondhand smoke can increase your child's risk for bronchiolitis and other infections.
- Keep your child away from people who are sick. Keep your child away from crowds or people with colds and other respiratory infections. Do not let other sick children sleep in the same bed as your child.
- Ask if the medicine that protects against RSV is right for your child. It may be given if your child has a high risk of becoming severely ill from RSV. When needed, your child will receive 1 dose every month for 5 months. The first dose is usually given in early November.
Follow up with your child's doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Bronchiolitis
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
