Bowel Management Program after Spinal Cord Injury
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
A bowel management program helps you have regular bowel movements. It can also help you control your bowel movements and prevent constipation or impaction. Impaction is when bowel movements get stuck in your rectum or colon. A bowel management program includes food and fluid intake, activity, medications, and scheduled bowel care. Talk to your healthcare provider about the best bowel management program for you.
DISCHARGE INSTRUCTIONS:
Seek care immediately if:
The following may be symptoms of autonomic dysreflexia:
- You have sudden changes in your vision.
- Your heart is beating faster than usual and you suddenly feel anxious.
- Your skin above the spinal cord injury is red and sweaty.
- You have a severe headache.
Contact your healthcare provider if:
- You have a fever.
- Your abdomen is swollen and hard.
- You have blood in your bowel movement or coming from your rectum.
- You do not have a bowel movement for 2 days or more.
- You are vomiting or have diarrhea for 2 or more days.
- The skin near your rectum or on your buttocks is sore or open.
- You have questions or concerns about your condition or care.
What you need to know about foods, liquids, and bowel management:
Food and liquids are an important part of your bowel management program. Certain foods can help you have regular bowel movements. Liquids can help prevent constipation and soften your bowel movements. Your healthcare provider will tell you if you need to be on a special diet. The following are tips about food and liquids that will help manage your bowel movements:
- Drink liquids such as water, juice, and milk. Do not drink liquids with caffeine. Caffeine can cause constipation or diarrhea. Your healthcare provider will tell you how much liquid to drink each day.
- Eat a variety of healthy foods. Choose foods that are also high in fiber. Healthy foods that are also high in fiber include fruits, vegetables, whole-grain breads and cereals, and beans. Fiber may help decrease constipation by adding bulk to your bowel movements. Your healthcare provider or dietitian can help you create a healthy, high-fiber meal plan.
-

What you need to know about activity and bowel management:
Activity can help keep your bowels moving. Your healthcare provider can help you find activities that are safe for you. The following are examples of how you can stay active:
- Change your position often. Have someone help you change the side you lie on in bed. Move from lying to sitting or standing with help, if possible.
- Do range of motion (ROM) exercises several times a day or as directed. ROM exercises help prevent stiff muscles and joints.
What you need to know about medicines and bowel management:
Medicines, such as stool softeners, laxatives, enemas, and suppositories, can help you have regular bowel movements. These medicines increase bowel activity and make your bowel movements softer. Take your medicines as directed. Call your healthcare provider if you think your medicine is not helping or if you have side effects.
What you need to know about scheduled bowel care:
Scheduled bowel care means planning a time to have a bowel movement every day. Scheduled bowel care may help train your body to have regular bowel movements. You may schedule bowel movements 1 to 2 times each day or more. You may instead schedule bowel care for every other day. You and your healthcare provider can decide which schedule is right for you.
Tips that can help you have a bowel movement:
Your healthcare provider may tell you to do any of the following to help you have a bowel movement:
- Eat or drink 15 to 30 minutes before you try to have a bowel movement. This may help start movement in your bowels.
- Sit up to have your bowel movement, if possible. This will make it easier for the bowel movement to move down through your colon. Use arm rests or safety straps if needed.
- Massage your abdomen. Place the palm of your hand on the lower right part of your abdomen. Press in and move up to your ribs and straight across to the left side of your abdomen. Continue to press and move your hand down the left side of your abdomen. Repeat 10 times, waiting about 30 seconds in between.
- Use digital stimulation. Wash your hands and put on gloves. Lubricate one of your fingers. Insert your finger 2 to 3 inches inside your rectum. Point your finger toward your belly button and move it in a circle for about 20 seconds. Stop when you feel gas or bowel movement. Repeat this every 5 to 10 minutes until you have a bowel movement. You can also use your finger to scoop out any bowel movement that is stuck in your rectum.
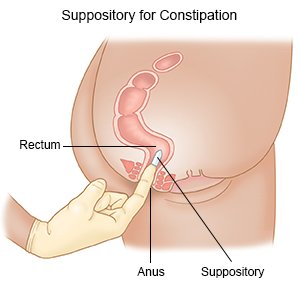
- Insert a suppository or enema as directed. Wash your hands before and after you insert a suppository or enema. You may need someone to help you insert a suppository or enema.
Keep a bowel care record:
A bowel care record helps you and your healthcare providers know if your bowel program is working. Write down the following information after each scheduled bowel care:
- Date and time of the bowel movement
- How long it took to have the bowel movement
- Description of your bowel movement, such as soft or hard
- Position during the bowel movement
- Anything that helped you have a bowel movement, such as abdominal massage or a suppository
Follow up with your healthcare provider as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Bowel Management Program after Spinal Cord Injury
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
