Hypercoagulation
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is hypercoagulation?
Hypercoagulation is a condition that causes your blood to clot more easily than normal. Hypercoagulation can be an acquired or inherited condition. Acquired hypercoagulation is caused by a disease or other condition. Examples include obesity, pregnancy, use of birth control pills, or cancer. Inherited coagulation is caused by genes that have been passed to you from a parent. These genes cause problems with how your blood clots. You may have no signs or symptoms of hypercoagulation until you get a blood clot.
What increases my risk for hypercoagulation?
- Limited mobility caused by bed rest, a leg cast, or sitting for long periods
- Smoking
- Dehydration
- Age older than 60
- HIV and HIV treatments
- Surgery or trauma
- An implanted devices such as a central venous catheter or dialysis shunt
- Hormone replacement therapy
- Cancer
- Diabetes, atrial fibrillation, heart disease, or heart failure
What problems can hypercoagulation cause?
Hypercoagulation may cause blood clots to form anywhere in your body. Some of these conditions may become life-threatening. You may be at risk for any of the following:
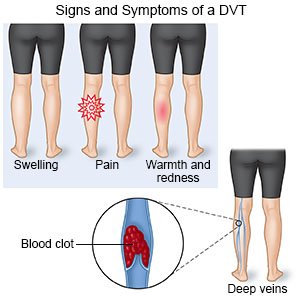
- A deep venous thrombosis (DVT) happens when a clot forms in a deep vein, such as veins in your legs or pelvis. This blocks blood flow to parts of your leg and foot. A DVT may travel to other parts of your body and block blood flow.
- A stroke happens when a blood clot blocks blood flow to your brain.
- A heart attack happens when a blood clot blocks blood flow to your heart.
- A pulmonary embolism (PE) happens when a blood clot blocks blood flow to your lungs.
- Problems with pregnancy , such as clots in the placenta, may happen. The placenta provides oxygen and nutrition to your unborn baby. The placenta also removes waste products from the baby. Clots in the placenta can reduce blood flow to the baby. This may cause a miscarriage or problems with the baby's development.
- Peripheral artery disease (PAD) happens when blood flow to the legs and pelvis decreases. It is caused by tiny clots in the blood vessels in your pelvis or legs.
- Kidney failure can happen when 1 or more blood clots block blood flow to your kidneys. This prevents the kidneys from removing waste and fluid from your body.
How is hypercoagulation diagnosed?
Your healthcare provider will examine you. Tell him or her if you have ever had a blood clot or miscarriage and if you take any medicines. Also tell him or her if anyone in your family has had blood clots. You may need blood tests to check your blood cell levels, blood protein levels, and how well your blood clots. Blood proteins help control how your blood clots. Blood tests may also show if you have other conditions, such as Factor V Leiden, that cause hypercoagulation.
How is hypercoagulation treated?
The goal of treatment is to prevent a blood clot from forming. Treatment depends on the cause of your hypercoagulation. Conditions such as diabetes or heart disease may need to be treated. Medicines that cause blood clots may be stopped or changed. You may need any of the following medicines:
- Blood thinners , such as heparin or warfarin, help stop clots from forming.
- Antiplatelets , such as aspirin or clopidogrel, prevent your platelets from sticking together and forming blood clots.
- Clot busters are medicines given in an emergency to break apart blood clots. These medicines are usually given to treat a DVT, stroke, PE, or heart attack.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I decrease my risk for a blood clot?
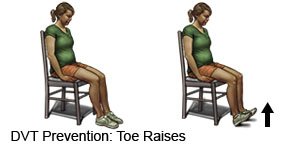
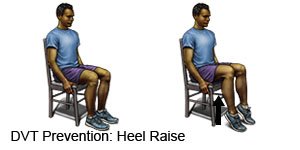
- Change your body position often during travel and at work. If you travel by airplane, get up and walk around once every hour. Move and stretch in your seat several times each hour. Do leg exercises at work and during travel to increase blood flow through your legs.
- Point your toes toward your shin. Then point them toward the ground. Do this 10 times every hour.
- Pull each knee to your chest and hold it for 15 seconds. Then straighten your leg. Do this 10 times every hour.
- Point your toes toward your shin. Then point them toward the ground. Do this 10 times every hour.
- Change your position every 2 hours in bed. If you need help to move, ask other family members to help you change your position.
- Eat a variety of healthy foods. Healthy foods can help you manage your weight and other health problems. Examples include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Ask if you need to be on a special diet.

- Drink plenty of liquids. Liquids can help prevent dehydration. Ask how much liquid to drink each day and which liquids are best for you. You should drink extra liquids before plane rides and long car rides.
- Get plenty of exercise. Talk to your healthcare provider about the best exercise plan for you. Exercise can help you lose weight, keep your heart healthy, and help manage other conditions.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can heart and lung damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Wear pressure stockings as directed. These are tight elastic stockings that squeeze the lower part of your legs to improve circulation. This helps keep blood clots from forming. Ask your healthcare provider where to buy these products.

- Talk to your healthcare provider before you get pregnant. You may need to take medicine to prevent blood clots during your pregnancy.
Call your local emergency number (911 in the US) or have someone else call if:
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
When should I seek immediate care?
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
When should I call my doctor?
- You have a fever or chills.
- You have hard, bulging veins on your arms or legs.
- You have skin changes, such as wounds or reddish blue spots.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Hypercoagulation
Treatment options
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
