Cinacalcet (Monograph)
Brand name: Sensipar
Drug class: Antiparathyroid Agents
- Calcium-sensing Receptor Agonists
- Calcimetic Agents
VA class: HS900
Chemical name: N-[1-(R)-(-)-(1-naphthyl)ethyl]-3-[3-(trifluoromethyl)phenyl]-1-aminopropane hydrochloride
Molecular formula: C22H22F3N HCl
CAS number: 364782-34-3
Introduction
Calcimimetic agent; binds to and increases sensitivity of calcium-sensing receptors on parathyroid glands to extracellular calcium, resulting in decreased serum parathyroid hormone (PTH) and calcium concentrations.1 2 12 13 16 17 31
Uses for Cinacalcet
Secondary Hyperparathyroidism Associated with Chronic Renal Disease
Treatment of secondary hyperparathyroidism associated with chronic renal disease in patients who are undergoing hemodialysis or peritoneal dialysis.1 18
Safety and efficacy in patients who are not undergoing dialysis have not been established.1
May be used alone or in conjunction with vitamin D analogs and/or phosphate binders.1
Effects on clinical outcomes remain to be fully determined.35 The primary finding of the EVOLVE trial (a lack of effect on mortality or major cardiovascular events32 ) is controversial because of study limitations.33 34 35
Hypercalcemia Associated with Parathyroid Carcinoma
Management of hypercalcemia associated with parathyroid carcinoma; designated an orphan drug by FDA for this use.1 18 20 23 26
Hypercalcemia Associated with Primary Hyperparathyroidism
Treatment of hypercalcemia associated with primary hyperparathyroidism in patients who would be candidates for parathyroidectomy based on serum calcium concentrations but who are unable to undergo the surgery; designated an orphan drug by FDA for this use.1 24 25 26
Cinacalcet Dosage and Administration
Administration
Oral Administration
Administer orally with food or shortly after a meal.1 (See Food under Pharmacokinetics.)
Swallow tablets whole; do not divide.1
Dosage
Available as cinacalcet hydrochloride; dosage expressed in terms of cinacalcet.1
Individualize dosage.1
Severe or prolonged nausea and vomiting can result in dehydration and worsening hypercalcemia; carefully monitor electrolytes in patients with these adverse effects.1
Adults
Secondary Hyperparathyroidism Associated with Chronic Renal Disease
Oral
Usual initial dosage: 30 mg once daily.1
Manufacturer recommends increasing dosage no more frequently than every 2–4 weeks through sequential adjustments to 60, 90, 120, and 180 mg once daily to achieve a target intact parathyroid hormone (iPTH) concentration of 150–300 pg/mL.1
Median dosage was 90 mg daily in 6-month clinical studies; patients with milder disease generally required lower dosages.1
Do not initiate cinacalcet if baseline serum calcium concentration is <8.4 mg/dL.1
Measure serum calcium and phosphorus concentrations within 1 week and iPTH concentrations 1–4 weeks after initiation or subsequent dosage adjustment; do not assess serum iPTH concentrations earlier than 12 hours following an oral dose.1
If serum calcium concentrations fall to <8.4 mg/dL but remain >7.5 mg/dL, or if manifestations of hypocalcemia occur, may use calcium-containing phosphate binders and/or vitamin D analogs to increase serum calcium concentrations.1
If serum calcium concentrations fall to <7.5 mg/dL, or hypocalcemia manifestations persist and vitamin D dosage cannot be increased, withhold cinacalcet.1 When serum calcium concentrations reach 8 mg/dL and/or manifestations of hypocalcemia have resolved, may reinitiate cinacalcet using the next lowest dosage.1
Once maintenance dosage is established, measure serum calcium and phosphorus concentrations monthly.1
Hypercalcemia Associated with Parathyroid Carcinoma
Oral
Usual initial dosage: 30 mg twice daily.1
Increase dosage every 2–4 weeks through sequential adjustments to 60 mg twice daily, 90 mg twice daily, and 90 mg 3 or 4 times daily as needed to normalize serum calcium concentrations.1
Measure serum calcium concentration within 1 week of cinacalcet initiation or dosage adjustment; measure every 2 months once an appropriate maintenance dosage has been established.1
Hypercalcemia Associated with Primary Hyperparathyroidism
Oral
Usual initial dosage: 30 mg twice daily.1
Increase dosage every 2–4 weeks through sequential adjustments to 60 mg twice daily, 90 mg twice daily, and 90 mg 3 or 4 times daily as needed to normalize serum calcium concentrations.1
Measure serum calcium concentration within 1 week of cinacalcet initiation or dosage adjustment; measure every 2 months once an appropriate maintenance dosage has been established.1
Special Populations
No special population dosage recommendations at this time.1 (See Hepatic Impairment under Cautions.)
Cautions for Cinacalcet
Contraindications
-
Serum calcium concentrations below lower limit of normal.1
Warnings/Precautions
Hypocalcemia
Fatal or life-threatening hypocalcemia reported, including in pediatric patients (see Pediatric Use under Cautions).1 Substantial lowering of serum calcium can cause paresthesias, myalgia, muscle spasm, tetany, seizures, QT-interval prolongation, and ventricular arrhythmias.1
Seizures (mainly generalized or tonic-clonic) reported in 1.4 or 0.7% of patients receiving cinacalcet or placebo, respectively.1 Reason for reported difference is unclear, but substantial reductions in serum calcium concentrations may lower seizure threshold.1
Cases of QT-interval prolongation and ventricular arrhythmia secondary to hypocalcemia reported.1
Isolated idiosyncratic cases of hypotension, worsening heart failure, and/or arrhythmia reported in patients with impaired cardiac function.1 Causal relationship to cinacalcet not excluded; effects possibly mediated by reductions in serum calcium.1
Nondialysis patients with chronic renal disease and secondary hyperparathyroidism are at increased risk for developing hypocalcemia;1 29 safety and efficacy in such patients not established.1
Carefully monitor patients for the occurrence of hypocalcemia; particularly close monitoring required in patients with history of seizure disorder.1
If serum calcium concentration falls to <8.4 mg/dL or if hypocalcemia manifestations occur in patients with secondary hyperparathyroidism associated with chronic renal disease, take appropriate steps (e.g., supplement calcium, initiate or increase dosage of calcium-containing phosphate binder or vitamin D analog, temporarily discontinue cinacalcet administration) to increase serum calcium concentrations.1 (See Secondary Hyperparathyroidism Associated with Chronic Renal Disease under Dosage and Administration.)
Upper GI Bleeding
Upper GI bleeding reported, but exact cause not established.1 Patients with risk factors for upper GI bleeding (e.g., gastritis, esophagitis, ulcers, severe vomiting) may be at increased risk.1
Monitor patients for worsening of nausea and vomiting and for signs and symptoms of GI bleeding or ulceration.1 Immediately evaluate and treat if GI bleeding is suspected.1
Adynamic Bone Disease
Adynamic bone disease may develop if iPTH concentrations are suppressed below 100 pg/mL.1
Decrease dosage or discontinue cinacalcet and/or vitamin D analogs if iPTH concentrations fall below 150 pg/mL.1
Specific Populations
Pregnancy
Category C.1 Pregnancy surveillance program (800-772-6436).1
Lactation
Distributed into milk in rats; not known whether distributed into human milk.1 Discontinue nursing or the drug.1 Encourage women who opt to continue cinacalcet treatment while nursing to enroll in manufacturer's lactation surveillance program (800-772-6436).1
Pediatric Use
Safety and efficacy not established in patients <18 years of age; not indicated for use in pediatric patients.1 19
FDA announced suspension of pediatric clinical trials of cinacalcet after death of a 14-year-old adolescent with severe hypocalcemia occurred during a trial.1 22
Geriatric Use
No substantial differences in pharmacokinetics, safety, and efficacy relative to younger adults; however, greater sensitivity of some older patients cannot be ruled out.1
Hepatic Impairment
Closely monitor serum phosphorus, iPTH, and serum calcium concentrations in patients with moderate or severe hepatic impairment.1 (See Absorption: Special Populations and also Elimination: Special Populations, under Pharmacokinetics.)
Common Adverse Effects
Dialysis patients with secondary hyperparathyroidism: Nausea,1 2 12 13 16 32 vomiting,1 2 12 16 17 32 diarrhea,1 32 myalgia,1 dyspnea,1 cough,1 hypotension,1 headache,1 hypocalcemia,1 32 muscle spasms,1 abdominal pain (including upper abdominal pain),1 dizziness,1 hyperkalemia,1 upper respiratory tract infection,1 dyspepsia,1 hypertension,1 asthenia,1 anorexia/decreased appetite,1 12 noncardiac chest pain,1 access infection,1 constipation.1
Patients with hypercalcemia associated with parathyroid carcinoma or primary hyperparathyroidism: Adverse effects generally similar to those observed in dialysis patients.1
Metabolized mainly by CYP1A2, 2D6, and 3A4; potent inhibitor of CYP2D6 in vitro.1 Does not inhibit CYP1A2, 2C9, 2C19, or 3A4 in vitro.1 Does not induce CYP isoenzymes in vitro.1
Drugs Affecting Hepatic Microsomal Enzymes
Potent CYP3A4 inhibitors: Potential increased plasma cinacalcet concentrations.1 Closely monitor iPTH and serum calcium concentrations upon initiation or discontinuance of potent CYP3A4 inhibitor; cinacalcet dosage adjustment may be required.1
Potent CYP3A4 inducers: Potential decreased plasma cinacalcet concentrations.30 Cinacalcet dosage adjustment may be required if a potent CYP3A4 inducer is initiated or discontinued.30
Potent CYP1A2 inhibitors: Potential increased plasma cinacalcet concentrations.30 Cinacalcet dosage adjustment may be required if a potent CYP1A2 inhibitor is initiated or discontinued.30
Drugs Metabolized by Hepatic Microsomal Enzymes
CYP2D6 substrates: Potential increased plasma concentrations of drugs metabolized principally by CYP2D6.1 Dosage adjustment may be required if cinacalcet is administered concomitantly with a drug that is metabolized principally by CYP2D6, particularly one with a narrow therapeutic index.1
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antidepressants, tricyclic |
Possible increased plasma tricyclic antidepressant concentrations1 Amitriptyline: Increased AUC (by about 17–23%) and peak plasma concentration (by about 11–21%) of amitriptyline and nortriptyline (active metabolite) in CYP2D6 extensive metabolizers1 Desipramine: Desipramine AUC and peak plasma concentrations increased by 264 and 75%, respectively, in CYP2D6 extensive metabolizers1 |
Adjust dosage of tricyclic antidepressant if needed1 |
|
Calcium salts |
Calcium carbonate: Clinically important pharmacokinetic interaction unlikely1 30 |
|
|
Carvedilol |
Possible increased plasma carvedilol concentrations1 |
Adjust carvedilol dosage if needed1 |
|
Cigarette smoking |
Cinacalcet clearance increased by 36–38%30 |
Adjust cinacalcet dosage as needed if patient starts or stops smoking30 |
|
Dextromethorphan |
Dextromethorphan AUC increased 11-fold in CYP2D6 extensive metabolizers30 |
|
|
Flecainide |
Possible increased plasma flecainide concentrations1 |
Adjust flecainide dosage if needed1 |
|
Itraconazole |
Possible increased plasma cinacalcet concentrations1 |
Closely monitor iPTH and serum calcium concentrations upon initiation or discontinuance of itraconazole; adjust cinacalcet dosage if needed1 |
|
Ketoconazole |
Cinacalcet AUC and peak plasma concentration increased by 127 and 116%, respectively1 |
Closely monitor iPTH and serum calcium concentrations upon initiation or discontinuance of ketoconazole; adjust cinacalcet dosage if needed1 |
|
Metoprolol |
Possible increased plasma metoprolol concentrations1 |
Adjust metoprolol dosage if needed1 |
|
Midazolam |
Clinically important pharmacokinetic interaction unlikely1 30 |
|
|
Pantoprazole |
Clinically important pharmacokinetic interaction unlikely1 30 |
|
|
Rifampin |
Possible decreased plasma cinacalcet concentrations30 |
Adjust cinacalcet dosage as needed if rifampin is initiated or discontinued30 |
|
Sevelamer |
Clinically important pharmacokinetic interaction unlikely1 30 |
|
|
Warfarin |
Clinically important pharmacokinetic or pharmacodynamic interaction unlikely1 30 |
Cinacalcet Pharmacokinetics
Absorption
Bioavailability
Following oral administration, peak plasma concentration usually is attained within 2–6 hours.1
Onset
Nadir in iPTH concentration occurs 2–6 hours after a dose.1
Food
Food increases extent of absorption.1
A high-fat meal increases peak plasma concentration by about 82% and AUC by about 68%.1
A low-fat meal increases peak plasma concentration by about 65% and AUC by about 50%.1
Special Populations
In patients with moderate or severe hepatic impairment, AUC was 2.4 or 4.2 times higher, respectively, than in healthy individuals.1
Distribution
Extent
Extensively distributed.1
Cinacalcet crosses the placenta in animals and is distributed into milk in rats; not known whether distributed into human milk.1
Plasma Protein Binding
About 93–97%.1
Elimination
Metabolism
Metabolized to inactive hydrocinnamic acid and to hydroxy-hydrocinnamic acid, which are further metabolized by glycine conjugation and by β-oxidation, and to glucuronidated dihydrodiols with minimal activity.1
Cinacalcet is metabolized by multiple enzymes, mainly CYP3A4, CYP2D6, and CYP1A2.1
Elimination Route
Excreted in urine (80%), mainly as metabolites, and in feces (15%).1
Half-life
Biphasic; terminal half-life is 30–40 hours.1
Special Populations
In patients with moderate or severe hepatic impairment, plasma half-life was prolonged by about 33 or 70%, respectively, compared with healthy individuals.1
Renal impairment (including hemodialysis or peritoneal dialysis) and age (≥65 years versus <65 years) do not alter cinacalcet pharmacokinetics.1
Stability
Storage
Oral
Tablets
25°C (may be exposed to 15–30°C).1
Actions
-
Binds to and allosterically modulates calcium-sensing receptors (principal regulators of PTH secretion) on parathyroid glands to increase their sensitivity to activation by extracellular calcium, thereby inhibiting PTH secretion.1 2 12 13 16 17 31
-
Lowers serum PTH concentrations within a few hours after oral administration.1 2 12 13 16 17
-
In dialysis patients with secondary hyperparathyroidism, serum calcium and phosphorus concentrations usually decline as PTH concentrations decrease.1 2 12 13 16 17
Advice to Patients
-
Advise patients to report nausea, vomiting, and symptoms of hypocalcemia (e.g., paresthesias, myalgia, muscle spasms, seizures).1 Ask patients if they have a history of seizures or are taking anticonvulsants.1
-
Advise patients to report any symptoms of upper GI bleeding to their clinician.1
-
Inform patients of the importance of routine blood tests to monitor safety and efficacy of cinacalcet therapy.1
-
Importance of taking cinacalcet with food or shortly after a meal.1
-
Importance of swallowing the tablets whole (and not divided).1
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 Encourage women who receive cinacalcet during pregnancy or while breast-feeding to enroll in manufacturer's pregnancy or lactation surveillance program.1
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.1
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
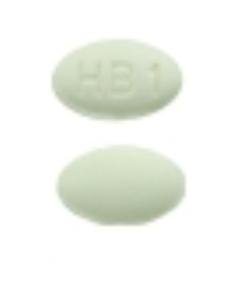
Oral |
Tablets, film-coated |
30 mg (of cinacalcet) |
Sensipar |
Amgen |
|
60 mg (of cinacalcet) |
Sensipar |
Amgen |
||
|
90 mg (of cinacalcet) |
Sensipar |
Amgen |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions August 28, 2017. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Amgen Inc. Sensipar (cinacalcet hydrochloride) tablets prescribing information. Thousand Oaks, CA; 2017 Mar.
2. Block GA, Martin KJ, de Francisco AL et al. Cinacalcet for secondary hyperparathyroidism in patients receiving hemodialysis. N Engl J Med. 2004; 350:1516-25. http://www.ncbi.nlm.nih.gov/pubmed/15071126?dopt=AbstractPlus
3. Bleyer AJ, Burke SK, Dillon M et al. A comparison of the calcium-free phosphate binder sevelamer hydrochloride with calcium acetate in the treatment of hyperphosphatemia in hemodialysis patients. Am J Kidney Dis. 1999; 33:694-701. http://www.ncbi.nlm.nih.gov/pubmed/10196011?dopt=AbstractPlus
4. Chertow GM, Dillon M, Burke SK et al. A randomized trial of sevelamer hydrochloride (Renagel) with and without supplemental calcium: Strategies for the control of hyperphosphatemia and hyperparathyroidism in hemodialysis patients. Clin Nephrol. 1999; 51:18-26. http://www.ncbi.nlm.nih.gov/pubmed/9988142?dopt=AbstractPlus
5. Chertow GM, Burke SK, Lazarus JM et al. Poly[allylamine hydrochloride] (RenaGel): a noncalcemic phosphate binder for the treatment of hyperphosphatemia in chronic renal failure. Am J Kidney Dis. 1997; 29:66-71. http://www.ncbi.nlm.nih.gov/pubmed/9002531?dopt=AbstractPlus
6. Sakhaee K, Gonzalez GB. Update on renal osteodystrophy: pathogenesis and clinical management. Am J Med Sci. 1999; 317:251-60. http://www.ncbi.nlm.nih.gov/pubmed/10210362?dopt=AbstractPlus
7. Tan AU Jr, Levine BS, Mazess RB et al. Effective suppression of parathyroid hormone by 1 alpha-hydroxy-vitamin D2a in hemodialysis patients with moderate to severe secondary hyperparathyroidism. Kidney Int. 1997; 51:317-23. http://www.ncbi.nlm.nih.gov/pubmed/8995749?dopt=AbstractPlus
8. Bone Care International. Hectorol (doxercalciferol) capsules prescribing information. Madison, WI; 1999 Jun 9.
9. Burke S, Dillon MA, Goldberg DI. Control of P1 with Renagel, a calcium and aluminum free phosphate binder, combined with vitamin D stabilizes iPTH in ESRD independent of Ca++. Nephrology. 1997; (Suppl 1):S183.
10. Genzyme, Boston, MA: Personal communication on sevelamer.
12. Ohashi N, Uematsu T, Nagashima M et al. The calcimimetic agent KRN 1493 lowers plasma parathyroid hormone and ionized calcium concentrations in patients with chronic renal failure on haemodialysis both on the day of haemodialysis and on the day without haemodialysis. Br J Clin Pharmacol. 2004; 57:726-34. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1884513&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/15151518?dopt=AbstractPlus
13. Lindberg JS, Moe SM, Goodman WG et al. The calcimimetic AMG 073 reduces parathyroid hormone and calcium x phosphorus in secondary hyperparathyroidism. Kidney Int. 2003; 63:248-54. http://www.ncbi.nlm.nih.gov/pubmed/12472790?dopt=AbstractPlus
14. Genzyme. Renagel (sevelamer hydrochloride) capsules and tablets prescribing information. Cambridge, MA; 2000 Jul.
15. Slatopolsky EA, Burke SK, Dillon MA and the RenaGel Study Group. RenaGel, a nonadsorbed calcium- and aluminum-free phosphate binder, lowers serum phosphorus and parathyroid hormone. Kidney Int. 1999; 55:299-307. http://www.ncbi.nlm.nih.gov/pubmed/9893140?dopt=AbstractPlus
16. Goodman WG, Hladik GA, Turner SA et al. The calcimimetic agent AMG 073 lowers plasma parathyroid hormone levels in hemodialysis patients with secondary hyperparathyroidism. J Am Soc Nephrol. 2002; 13:1017-24. http://www.ncbi.nlm.nih.gov/pubmed/11912261?dopt=AbstractPlus
17. Quarles LD, Sherrard DJ, Adler S et al. The calcimimetic AMG 073 a a potential treatment for secondary hyperparathyroidism of end-stage renal disease. J Am Soc Nephrol. 2003; 14:575-83. http://www.ncbi.nlm.nih.gov/pubmed/12595492?dopt=AbstractPlus
18. Anon. Cinacalcet (Sensipar). Med Lett Drugs Ther. 2004; 46:80. http://www.ncbi.nlm.nih.gov/pubmed/15452465?dopt=AbstractPlus
19. Amgen Inc. Thousand Oaks, CA: Personal communication.
20. Food and Drug Administration. Cumulative list of orphan products designated and approved. Rockville, MD;. Accessed [2004 11 17]. http://www.fda.gov/ForIndustry/DevelopingProductsforRareDiseasesConditions/HowtoapplyforOrphanProductDesignation/default.htm
21. Moe SM, Sprague SM, Cunningham J et al. Long-term treatment of secondary hyperparathyroidism with the calcimimetic cinacalcet HCl. Paper presented at 36th annual American Society of Nephrology meeting and scientific exposition. San Diego, CA: 2003 Nov 15.
22. Food and Drug Administration. Sensipar (cinacalcet hydrochloride): Drug safety communication - FDA suspends pediatric clinical trials after report of death. . Silver Spring, MD; 2013 Feb 26. From FDA website. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm341255.htm
23. Silverberg SJ, Rubin MR, Faiman C et al. Cinacalcet hydrochloride reduces the serum calcium concentration in inoperable parathyroid carcinoma. J Clin Endocrinol Metab. 2007; 92:3803-8. http://www.ncbi.nlm.nih.gov/pubmed/17666472?dopt=AbstractPlus
24. Marcocci C, Chanson P, Shoback D et al. Cinacalcet reduces serum calcium concentrations in patients with intractable primary hyperparathyroidism. J Clin Endocrinol Metab. 2009; 94:2766-72. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=3214593&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/19470620?dopt=AbstractPlus
25. Khan A, Bilezikian J, Bone H et al. Cinacalcet normalizes serum calcium in a double-blind randomized, placebo-controlled study in patients with primary hyperparathyroidism with contraindications to surgery. Eur J Endocrinol. 2015; 172:527-35. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=5729741&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/25637076?dopt=AbstractPlus
26. Food and Drug Administration. FDA Application: Search Orphan Drug Designations and Approvals. Rockville, MD. From FDA website. Accessed 2017 March 28. https://www.accessdata.fda.gov/scripts/opdlisting/oopd/listResult.cfm
27. Cunningham J, Locatelli F, Rodriguez M. Secondary hyperparathyroidism: pathogenesis, disease progression, and therapeutic options. Clin J Am Soc Nephrol. 2011; 6:913-21. http://www.ncbi.nlm.nih.gov/pubmed/21454719?dopt=AbstractPlus
28. Amgen Inc. Parsabiv (etelcalcetide hydrochloride) injection prescribing information. Thousand Oaks, CA; 2017 Feb.
29. Chonchol M, Locatelli F, Abboud HE et al. A randomized, double-blind, placebo-controlled study to assess the efficacy and safety of cinacalcet HCl in participants with CKD not receiving dialysis. Am J Kidney Dis. 2009; 53:197-207. http://www.ncbi.nlm.nih.gov/pubmed/19110359?dopt=AbstractPlus
30. Amgen Europe. Mimpara (cinacalcet) tablets. Annex I: Summary of product characteristics. Breda, Netherlands. (undated).
31. Marcocci C, Cetani F. Update on the use of cinacalcet in the management of primary hyperparathyroidism. J Endocrinol Invest. 2012; 35:90-5. http://www.ncbi.nlm.nih.gov/pubmed/22104762?dopt=AbstractPlus
32. EVOLVE Trial Investigators, Chertow GM, Block GA et al. Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med. 2012; 367:2482-94. http://www.ncbi.nlm.nih.gov/pubmed/23121374?dopt=AbstractPlus
33. Parfrey PS, Block GA, Correa-Rotter R et al. Lessons Learned from EVOLVE for Planning of Future Randomized Trials in Patients on Dialysis. Clin J Am Soc Nephrol. 2016; 11:539-46. http://www.ncbi.nlm.nih.gov/pubmed/26614406?dopt=AbstractPlus
34. Goldsmith D, Covic A, Vervloet M et al. Should patients with CKD stage 5D and biochemical evidence of secondary hyperparathyroidism be prescribed calcimimetic therapy? An ERA-EDTA position statement. Nephrol Dial Transplant. 2015; 30:698-700. http://www.ncbi.nlm.nih.gov/pubmed/25928337?dopt=AbstractPlus
35. Bover J, Ureña P, Ruiz-García C et al. Clinical and Practical Use of Calcimimetics in Dialysis Patients With Secondary Hyperparathyroidism. Clin J Am Soc Nephrol. 2016; 11:161-74. http://www.ncbi.nlm.nih.gov/pubmed/26224878?dopt=AbstractPlus
36. Amgen Inc. Sensipar (cinacalcet hydrochloride) tablets prescribing information. Thousand Oaks, CA; 2004 Mar 8.
More about cinacalcet
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (10)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: calcimimetics
- Breastfeeding
- En español