Kymriah Dosage
Generic name: TISAGENLECLEUCEL 20000001
Dosage form: intravenous suspension
Drug class: Miscellaneous antineoplastics
Medically reviewed by Drugs.com. Last updated on Aug 1, 2023.
For autologous use only. For intravenous use only.
2.1 Dosage in Pediatric and Young Adult Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)
KYMRIAH is provided as a single-dose for infusion containing a suspension of chimeric antigen receptor (CAR)-positive viable T cells.
Based on the patient weight reported at the time of leukapheresis:
- Patients 50 kg or less: administer 0.2 to 5.0 x 106 CAR-positive viable T cells per kg body weight.
- Patients above 50 kg: administer 0.1 to 2.5 x 108 CAR-positive viable T cells.
2.2 Dosage in Adult Relapsed or Refractory (r/r) Diffuse Large B-cell Lymphoma (DLBCL) and Follicular Lymphoma (FL)
KYMRIAH is provided as a single-dose for infusion containing a suspension of chimeric antigen receptor (CAR)-positive viable T cells.
- For adult patients: administer 0.6 to 6.0 x 108 CAR-positive viable T cells.
2.3 Administration
Preparing Patient for KYMRIAH Administration with Lymphodepletion
- Confirm availability of KYMRIAH prior to starting the lymphodepleting regimen.
Pediatric and Young Adult Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)
- Lymphodepleting chemotherapy: Fludarabine (30 mg/m2 intravenously daily for 4 days) and cyclophosphamide (500 mg/m2 intravenously daily for 2 days starting with the first dose of fludarabine).
- Infuse KYMRIAH 2 to 14 days after completion of the lymphodepleting chemotherapy.
Adult Relapsed or Refractory (r/r) Diffuse Large B-cell Lymphoma (DLBCL) and r/r Follicular Lymphoma (FL)
• Lymphodepleting chemotherapy: Fludarabine (25 mg/m2 intravenously daily for 3 days) and cyclophosphamide (250 mg/m2 intravenously daily for 3 days starting with the first dose of fludarabine).
• Alternate lymphodepleting chemotherapy: bendamustine 90 mg/m2 intravenously daily for 2 days if a patient experienced a previous Grade 4 hemorrhagic cystitis with cyclophosphamide or demonstrates resistance to a previous cyclophosphamide containing regimen.
• Infuse KYMRIAH 2 to 11 days (r/r DLBCL) or 2 to 6 days (r/r FL) after completion of the lymphodepleting chemotherapy.
• Lymphodepleting chemotherapy may be omitted if a patient is experiencing significant cytopenia, e.g., white blood cell (WBC) count is less than 1 x 109/L within 1 week prior to KYMRIAH infusion.
Preparation of KYMRIAH for Infusion and Administration
Delay the infusion of KYMRIAH if a patient has unresolved serious adverse reactions (including pulmonary reactions, cardiac reactions, or hypotension) from preceding chemotherapies, active uncontrolled infection, active graft versus host disease (GVHD), or worsening of leukemia burden following lymphodepleting chemotherapy [see Warnings and Precautions (5.1)].
A KYMRIAH dose may be contained in one to three cryopreserved patient specific infusion bag(s). Verify the number of bags received for the dose of KYMRIAH with the Certificate of Conformance (CoC) and Certificate of Analysis (CoA). Coordinate the timing of thaw of KYMRIAH and infusion in the following manner. Confirm the infusion time in advance, and adjust the start time for thaw so that KYMRIAH is available for infusion when the recipient is ready. If more than one bag has been received for the treatment dose, thaw 1 bag at a time. Wait to thaw/infuse the next bag until it is determined that the previous bag is safely administered.
Preparation of KYMRIAH for Infusion
1. Ensure tocilizumab and emergency equipment are available prior to infusion and during the recovery period.
2. Premedicate patient with acetaminophen and diphenhydramine or another H1-antihistamine approximately 30 to 60 minutes prior to KYMRIAH infusion. Avoid prophylactic use of systemic corticosteroids, as it may interfere with the activity of KYMRIAH.
3. Confirm patient identity: Prior to KYMRIAH preparation, match the patient's identity with the patient identifiers on each KYMRIAH infusion bag(s). KYMRIAH is for autologous use only. Employ universal precautions to avoid potential transmission of infectious diseases when handling the product.
Note: The patient identifier number may be preceded by the letters DIN or Aph ID.
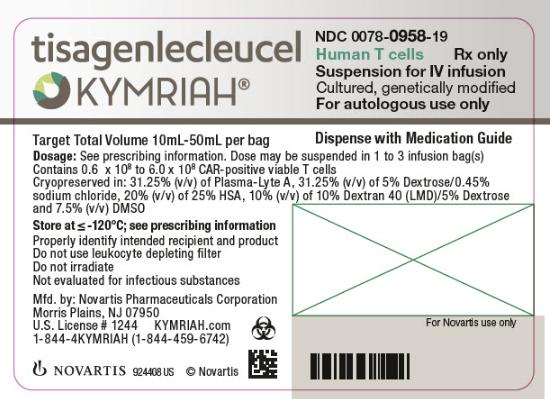
Figure 1. KYMRIAH Infusion Bag

4. Inspect the infusion bag(s) for any breaks or cracks prior to thawing. If a bag is compromised, do not infuse the contents. Call Novartis at 1-844-4KYMRIAH.
5. Place the infusion bag inside a second, sterile bag in case of a leak and to protect ports from contamination.
6. Thaw each infusion bag one at a time at 37°C using either a water bath or dry thaw method until there is no visible ice in the infusion bag. Remove bag from thawing device immediately; do not store product bag at 37°C. Once the infusion bag has been thawed and is at room temperature (20°C to 25°C), it should be infused within 30 minutes. Do not wash, spin down, and/or resuspend KYMRIAH in new media prior to infusion.
7. Inspect the contents of the thawed infusion bag for any visible cell clumps. If visible cell clumps remain, gently mix the contents of the bag. Small clumps of cellular material should disperse with gentle manual mixing. Do not infuse KYMRIAH if clumps are not dispersed, the infusion bag is damaged or leaking, or otherwise appears to be compromised. Call Novartis at 1-844-4KYMRIAH.
Administration
8. Confirm the patient’s identity with the patient identifiers on the infusion bag.
9. Administer KYMRIAH as an intravenous infusion at 10 mL to 20 mL per minute, adjusted as appropriate for smaller children and smaller volumes. The volume in the infusion bag ranges from 10 mL to 50 mL. Do NOT use a leukocyte-depleting filter. If more than one bag is being infused for the treatment dose, wait to thaw/infuse the next bag until it is determined that the previous bag is safely administered.
- Prime the tubing prior to infusion with sodium chloride 9 mg/mL (0.9%) solution for injection.
- Infuse all contents of the infusion bag.
- Rinse the infusion bag with 10 mL to 30 mL sodium chloride 9 mg/mL (0.9%) solution for injection while maintaining a closed tubing system to assure as many cells as possible are infused into the patient.
- Cells from all the bag(s) must be infused to complete a single dose.
KYMRIAH contains human cells genetically modified with a lentivirus. Follow local biosafety guidelines applicable for handling and disposal of such products.
Monitoring
- Administer KYMRIAH at a REMS-certified healthcare facility.
- Monitor patients 2-3 times during the first week following KYMRIAH infusion at the certified healthcare facility for signs and symptoms of CRS and neurologic toxicities [see Warnings and Precautions (5.1, 5.2)].
- Instruct patients to remain within proximity of the certified healthcare facility for at least 4 weeks following infusion.
- Instruct patients to refrain from driving or hazardous activities for at least 8 weeks following infusion.
2.4 Management of Severe Adverse Reactions
Cytokine Release Syndrome
Identify cytokine release syndrome (CRS) based on clinical presentation [see Warnings and Precautions (5.1)]. Evaluate for and treat other causes of fever, hypoxia, and hypotension. If CRS is suspected, manage according to the recommendations in Table 1 (Lee et al 2014). Alternative CRS management strategies may be implemented based on appropriate institutional or academic guidelines.
| aLee et al. 2014. bSantomasso et al. 2021. cRefer to tocilizumab Prescribing Information for details. dAlternative therapy includes anti-cytokine and anti-T cell therapies as per institutional policy and published guidelines such as (but not limited to) anakinra, siltuximab, ruxolitinib, cyclophosphamide, IVIG and ATG. |
|||
| CRS Grade a | Symptomatic treatment | Tocilizumab | Corticosteroids |
| Grade 1 Mild symptoms requiring symptomatic treatment only (e.g., low grade fever, fatigue, anorexia, etc.) |
Exclude other causes (e.g., infection) and treat specific symptoms (e.g., with antipyretics, antiemetics, analgesics, etc.) | In patients with persistent (> 3 days) or refractory fever, consider managing as Grade 2 CRSb. | Not applicable |
| Grade 2 Symptoms require and respond to moderate intervention Oxygen requirement < 40% or Hypotension responsive to fluids or low dose of one vasopressor or Grade 2 organ toxicity |
Antipyretics, oxygen, intravenous fluids and/or low dose vasopressors as needed. | Administer tocilizumabc intravenously over 1 hour: - 8 mg/kg (max. 800 mg) if body weight ≥ 30 kg - 12 mg/kg if body weight < 30 kg If no improvement after first dose, repeat every 8 hours (limit to a maximum of 3 dosages in 24 hours period; maximum total of 4 doses). |
If no improvement within 24 hours of tocilizumab, administer a daily dose of 2 mg/kg/day methylprednisolone intravenously (or equivalent) until vasopressor and oxygen no longer needed, then taper. If not improving, manage as appropriate grade below. |
| Grade 3 Symptoms require and respond to aggressive intervention Oxygen requirement ≥ 40% or Hypotension requiring high dose or multiple vasopressors or Grade 3 organ toxicity or Grade 4 transaminitis |
High-flow oxygen Intravenous fluids, and high-dose or multiple vasopressors Treat other organ toxicities as per local guidelines. |
Per Grade 2 If not improving, consider alternative therapyd. |
Per Grade 2 If not improving, manage as Grade 4. |
| Grade 4 Life-threatening symptoms Requirement for ventilator support or Grade 4 organ toxicity (excluding transaminitis) |
Mechanical ventilation Intravenous fluids and high-dose vasopressor(s) Treat other organ toxicities as per local guidelines. | Per Grade 2 If not improving, consider alternative therapyd. |
Administer methylprednisolone 1,000 mg intravenously one to two times per day for 3 days. If not improving, consider methylprednisolone 1,000 mg intravenously two to three times a day or alternate therapyd. Continue corticosteroids until improvement to Grade 1, and then taper as clinically appropriate. |
Neurologic Toxicities
Patients should be monitored for neurologic toxicities, including ICANS, following KYMRIAH infusion, particularly during and after resolution of CRS. Identify neurologic toxicities based on clinical presentation. Evaluate for and treat other causes of neurological symptoms. Consider non-sedating seizure prophylaxis (e.g., levetiracetam) for patients at higher risk of seizure, such as those with seizure history, CNS disease, concerning EEG findings, or neoplastic brain lesions. If neurologic toxicity is suspected, manage according to the recommendations in Table 2. Alternative neurologic toxicities management strategies may be implemented based on appropriate institutional, academic, or consensus guidelines.
| aASTCT criteria for grading NT (Lee et al. 2019); NCI CTCAE criteria for grading NT used in clinical trials. bICE Assessment Tool: (1) Orientation: orientation to year, month, city, and hospital: 4 points. (2) Naming: ability to name three objects (e.g., point to clock, pen, and button): 3 points. (3) Following commands: ability to follow simple commands (e.g., show me 2 fingers or close your eyes and stick out your tongue): 1 point. (4) Writing: ability to write a standard sentence (e.g., Our national bird is the bald eagle): 1 point. (5) Attention: ability to count backward from 100 by 10: 1 point. cSantomasso et. al. 2021. dAlternate therapy may include anakinra, siltuximab, ruxolitinib, cyclophosphamide, antithymocyte globulin, or intrathecal hydrocortisone (50 mg) plus methotrexate (12 mg). *A patient with an ICE score of 0 may be classified as Grade 3 ICANS if awake with global aphasia, but a patient with an ICE score of 0 may be classified as Grade 4 ICANS if unarousable. |
||
| ICANS Gradea | No concurrent CRS | Concurrent CRS |
| Grade 1 ICE scoreb: 7-9 with no depressed level of consciousness |
Offer supportive care with intravenous hydration and aspiration precautions. | Administer tocilizumab at any grade CRS, as per dosage recommendation in Table 1. Caution with repeated tocilizumab doses in patients with ICANS. Consider adding corticosteroids to tocilizumab past the first dose c. |
| Grade 2 ICE scoreb: 3-6 and/or Mild somnolence awaking to voice |
Supportive care as above. Consider dexamethasone 10 mg intravenously every 6-12 hours or methylprednisolone equivalent (1 mg/kg intravenously every 12 hours) until the event is Grade 1 or less. If improving, taper corticosteroids. |
Administer tocilizumab at any grade CRS, as per dosage recommendation in Table 1. If refractory to tocilizumab past the first dose, administer dexamethasone 10 mg intravenously every 6-12 hours or methylprednisolone equivalent (1 mg/kg intravenously every 12 hours) until the event is Grade 1 or less, then taper corticosteroids. |
| Grade 3 ICE scoreb: 0-2* and/or Depressed level of consciousness awakening only to tactile stimulus and/or Any clinical seizure focal or generalized that resolves rapidly or nonconvulsive seizures on EEG that resolve with intervention and/or Focal or local edema on neuroimaging |
Administer dexamethasone 10 mg intravenously every 6-12 hours or methylprednisolone equivalent (1 mg/kg intravenously every 12 hours) | Administer tocilizumab at any grade CRS, as per dosage recommendation in Table 1. Administer dexamethasone 10 mg intravenously every 6-12 hours or methylprednisolone equivalent (1 mg/kg intravenously every 12 hours). Continue corticosteroids until the event is Grade 1 or less, then taper corticosteroids. If not improving, manage as Grade 4. |
| Grade 4 ICE scoreb: 0* (patient is unarousable and unable to perform ICE) and/or Stupor or coma and/or Life-threatening prolonged seizure (> 5 minutes) or repetitive clinical or electrical seizures without return to baseline in between and/or Diffuse cerebral edema on neuroimaging, decerebrate or decorticate posturing or papilledema, cranial nerve VI palsy, or Cushing’s triad |
Consider mechanical ventilation for airway protection. Administer high-dose methylprednisolone intravenously 1,000 mg one to two times per day for 3 days. If not improving, consider 1,000 mg of methylprednisolone two to three times per day or alternate therapyd. Continue corticosteroids until improvement to Grade 1, and then taper as clinically appropriate. Treat seizures, status epilepticus, and cerebral edema as per institutional guidelines. |
Administer tocilizumab at any grade CRS, as per dosage recommendation in Table 1. Administer methylprednisolone 1,000 mg intravenously one to two times per day for 3 days. If not improving, consider methylprednisolone 1,000 mg intravenously two to three times per day or alternate therapyd. Continue corticosteroids until improvement to Grade 1, and then taper as clinically appropriate. Treat seizures, status epilepticus, and cerebral edema as per institutional guidelines. |
Frequently asked questions
- What is the cost of Kymriah?
- How is Kymriah administered?
- What type of drug is Kymriah (tisagenlecleucel)?
More about Kymriah (tisagenlecleucel)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Latest FDA alerts (2)
- Side effects
- During pregnancy
- FDA approval history
- Drug class: miscellaneous antineoplastics
- En español
Patient resources
Professional resources
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.