Sulfazine Side Effects
Generic name: sulfasalazine
Medically reviewed by Drugs.com. Last updated on Jul 24, 2023.
Note: This document contains side effect information about sulfasalazine. Some dosage forms listed on this page may not apply to the brand name Sulfazine.
Applies to sulfasalazine: oral tablet, oral tablet enteric coated.
Serious side effects of Sulfazine
Along with its needed effects, sulfasalazine (the active ingredient contained in Sulfazine) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking sulfasalazine:
More common
- Aching of joints
- fever
- headache (continuing)
- increased sensitivity of the skin to sunlight
- skin rash or itching
- vomiting
Less common
- Back, leg, or stomach pains
- bleeding gums
- bluish color of the fingernails, lips, skin, palms, or nail beds
- chills
- dark urine
- difficulty breathing
- fever
- general body swelling
- headache
- loss of appetite
- nausea
- nosebleeds
- pale skin
- sore throat
- trouble breathing
- unusual bleeding or bruising
- unusual tiredness or weakness
- yellowing of the eyes or skin
Less common or rare
- Aching of muscles
- black, tarry stools
- blistering, peeling, or loosening of the skin
- bloating
- blood in the urine or stools
- bloody diarrhea
- bluish fingernails, lips, or skin
- chest pain or tightness
- constipation
- cough
- difficulty with swallowing
- dizziness
- fainting spells
- fast heartbeat
- general feeling of discomfort or illness
- general tiredness and weakness
- hives
- indigestion
- inflammation of the joints
- irregular heartbeat
- light-colored stools
- muscle aches
- muscle cramps or spasms
- muscle pain or stiffness
- painful or difficult urination
- pains in the stomach, side, or abdomen, possibly radiating to the back
- pinpoint red spots on the skin
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- rash
- red skin lesions, often with a purple center
- red, irritated eyes
- redness, blistering, peeling, or loosening of the skin
- sores, ulcers, or white spots in the mouth or on the lips
- swollen or painful glands
- upper right abdominal or stomach pain
Incidence not known
- Large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
Other side effects of Sulfazine
Some side effects of sulfasalazine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Decreased weight
- stomach upset
Less common
- Welts
Less common or rare
- Discoloration of the skin or urine
- hair loss or thinning of the hair
- swelling or inflammation of the mouth
For Healthcare Professionals
Applies to sulfasalazine: compounding powder, oral delayed release tablet, oral tablet.
General
The most common side effects reported were anorexia, headache, nausea, vomiting, gastric distress, elevated temperature, erythema, pruritus, rash, loss of appetite, and reversible oligospermia. Less common side effects included urticaria, fever, Heinz body anemia, hemolytic anemia, and cyanosis. Frequency of side effects increased with daily doses of 4 g or more, or total serum sulfapyridine levels above 50 mcg/mL.
The use of enteric-coated preparations may decrease gastrointestinal side effects.
Gastrointestinal
Very common (10% or more): Nausea (up to 33%), vomiting (up to 33%), gastric distress (about 33%), dyspepsia (13%)
Common (1% to 10%): Abdominal pain, diarrhea, stomatitis
Frequency not reported: Impaired folic acid absorption, impaired digoxin absorption, neutropenic enterocolitis, hemorrhagic colitis, bloody diarrhea, necrotizing pancreatitis
Postmarketing reports: Pseudomembranous colitis, pancreatitis, worsening ulcerative colitis, parotitis[Ref]
Nervous system
Transverse myelitis developed in 1 patient after receiving sulfasalazine (the active ingredient contained in Sulfazine) for 2 years. All symptoms resolved within 2 months after discontinuing sulfasalazine.[Ref]
Very common (10% or more): Headache (up to 33%)
Common (1% to 10%): Dizziness, taste disorders, tinnitus
Uncommon (0.1% to 1%): Convulsions, vertigo
Frequency not reported: Meningitis, neuropathy, transverse myelitis, transient lesions of the posterior spinal column, cauda equina syndrome, Guillain-Barre syndrome, hearing loss, drowsiness, neurotoxicity, dysphasia, acute encephalopathy, monoparesis, cerebrospinal fluid abnormalities, altered taste, peripheral neuritis
Postmarketing reports: Aseptic meningitis, ataxia, encephalopathy, peripheral neuropathy, smell disorders[Ref]
Metabolic
Hypoglycemia has been reported rarely in patients using sulfonamides.
Very common (10% or more): Anorexia (about 33%)
Rare (less than 0.1%): Hypoglycemia
Postmarketing reports: Folate deficiency, loss of appetite
Genitourinary
Diuresis has been reported rarely in patients using sulfonamides.
Infertility appeared to be reversible upon drug discontinuation.[Ref]
Very common (10% or more): Reversible oligospermia (about 33%)
Common (1% to 10%): Proteinuria
Rare (less than 0.1%): Impotence, diuresis
Frequency not reported: Decreased motility, abnormal sperm penetration (sometimes resulted in infertility), urinary tract infections, urine discoloration
Postmarketing reports: Hematuria, crystalluria[Ref]
Dermatologic
Very common (10% or more): Rash (up to 13%)
Common (1% to 10%): Pruritus, urticaria
Uncommon (0.1% to 1%): Alopecia
Frequency not reported: Toxic epidermal necrolysis (Lyell's syndrome), skin discoloration, erythema multiforme, parapsoriasis varioliformis acuta (Mucha-Haberman syndrome), generalized skin eruptions, petechiae
Postmarketing reports: Angioedema, purpura, epidermal necrolysis (Lyell's syndrome), Stevens-Johnson syndrome, drug rash with eosinophilia and systemic symptoms (DRESS), toxic pustuloderma, erythema, exanthema, exfoliative dermatitis, periorbital edema, lichen planus, photosensitivity[Ref]
Angioedema was reported during postmarketing experience with the use of products containing or metabolized to mesalamine.
The risk of Stevens-Johnson syndrome or toxic epidermal necrolysis increased largely with the use of sulfonamides; however, these phenomena were rare as a whole.[Ref]
Immunologic
Very common (10% or more): Immunoglobulin suppression (10%)
Frequency not reported: Drug-induced systemic lupus erythematosus (SLE)
Postmarketing reports: Kawasaki-like syndrome with hepatic function changes, induction of autoantibodies[Ref]
Immunoglobulin suppression was slowly reversible and rarely accompanied by clinical findings.
In most cases of sulfasalazine-induced SLE, patients received the drug for greater than 1 year. Patients most commonly developed arthralgias and pleuritic chest pain. Generally, these patients had a positive ANA, anti-DNA antibody titer, and were slow acetylators of sulfonamides. Symptoms typically resolved over several weeks to several months.
At least 1 case of Kawasaki-like syndrome with hepatic function changes was reported during postmarketing experience with the use of products containing or metabolized to mesalamine.[Ref]
Hepatic
Hepatitis associated with sulfasalazine (the active ingredient contained in Sulfazine) often developed 2 to 4 weeks after therapy was initiated, although hypersensitivity hepatitis has been reported after longer periods of therapy. Associated rash usually progressed to desquamation. Liver biopsy has shown necrosis and infiltration with moderate number of inflammatory cells. Noncaseating granulomas have also been seen. Hepatitis generally resolved over several weeks after therapy discontinuation, although some patients progressed to fulminant hepatic failure.
Hepatitis has been reported in patients with sulfasalazine hypersensitivity. Some of these cases were fatal.
Side effects listed as postmarketing reports were reported during postmarketing experience with the use of products containing or metabolized to mesalamine.[Ref]
Common (1% to 10%): Abnormal liver function tests
Uncommon (0.1% to 1%): Elevated liver enzymes
Frequency not reported: Hepatic necrosis
Postmarketing reports: Hepatotoxicity (some cases were fatal), including elevated liver function tests (SGOT/AST, SGPT/ALT, GGT, LDH, alkaline phosphatase, bilirubin), jaundice, cholestatic jaundice, cirrhosis, cholestatic hepatitis, cholestasis, possible hepatocellular damage (including liver necrosis and liver failure); Kawasaki-like syndrome with hepatic function changes; fulminant hepatitis; hepatitis; hepatic failure[Ref]
Hematologic
Common (1% to 10%): Hemolytic anemia, Heinz body anemia, leukopenia
Uncommon (0.1% to 1%): Thrombocytopenia
Frequency not reported: Red cell aplasia, congenital neutropenia, myelodysplastic syndrome
Postmarketing reports: Pseudomononucleosis, lymphadenopathy, macrocytosis, neutropenia, pancytopenia, agranulocytosis, aplastic anemia, hypoprothrombinemia, methemoglobinemia, megaloblastic (macrocytic) anemia[Ref]
Agranulocytosis has generally occurred during the first 1 to 3 months of therapy. Patients often presented with fever and sore throat. A few also presented with a rash. Bone marrow hypoplasia or aplasia was usually confined to the myeloid series, but may be accompanied by erythroid hypoplasia and marrow plasmacytosis. In one review of 62 cases of sulfasalazine-induced agranulocytosis, 6.5% of patients died. Recovery of granulocytes was generally seen within 1 to 2 weeks after drug discontinuation, and leukocyte counts and differential returned to normal in 1 to 3 weeks. Some cases of agranulocytosis were treated with colony stimulating factor, which appeared to increase the time to recovery.[Ref]
Respiratory
Common (1% to 10%): Cough
Uncommon (0.1% to 1%): Dyspnea
Frequency not reported: Pulmonary infiltrates (frequently accompanied by eosinophilia), pneumonitis (with or without eosinophilia), pleuritis, bronchiolitis obliterans, lung toxicity (may mimic Wegener's granulomatosis)
Postmarketing reports: Oropharyngeal pain, fibrosing alveolitis, eosinophilic infiltration, interstitial lung disease[Ref]
Patients often presented after several weeks or months of therapy with fever, malaise, shortness of breath, and nonproductive cough. Eosinophilic infiltrates have been seen. Respiratory changes generally resolved over a few weeks, however, fatal reactions involving fibrosing alveolitis have been reported.[Ref]
Cardiovascular
Common (1% to 10%): Cyanosis
Uncommon (0.1% to 1%): Vasculitis
Frequency not reported: Tachycardia
Postmarketing reports: Myocarditis, allergic myocarditis, pallor, polyarteritis nodosa, pericarditis[Ref]
Psychiatric
Common (1% to 10%): Insomnia
Uncommon (0.1% to 1%): Depression
Frequency not reported: Confusion, vivid dreams
Postmarketing reports: Hallucinations[Ref]
Musculoskeletal
Common (1% to 10%): Arthralgia
Frequency not reported: Myopathy, rhabdomyolysis, Sjogren's syndrome
Postmarketing reports: Systemic lupus erythematosus
Other
Common (1% to 10%): Fever
Uncommon (0.1% to 1%): Facial edema
Frequency not reported: Malaise, false positive c-ANCAs, elevated temperature, petechiae and drug fever, LE phenomenon
Postmarketing reports: Yellow discoloration of skin and body fluids[Ref]
Ocular
Common (1% to 10%): Conjunctival and scleral injection
Frequency not reported: Diplopia, blurred vision, corneal damage[Ref]
Hypersensitivity
Frequency not reported: Hypersensitivity reactions, drug-induced rash, lupus erythematosus-like syndrome, anaphylactoid reactions
Postmarketing reports: Anaphylaxis, serum sickness[Ref]
The following side effects have been reported as hypersensitivity reactions: erythema multiforme (Stevens-Johnson syndrome), exfoliative dermatitis, epidermal necrolysis (Lyell's syndrome) with corneal damage, drug rash with eosinophilia and systemic symptoms (DRESS), anaphylaxis, serum sickness syndrome, pneumonitis (with or without eosinophilia), vasculitis, fibrosing alveolitis, pleuritis, pericarditis (with or without tamponade), allergic myocarditis, polyarteritis nodosa, lupus erythematosus-like syndrome, hepatitis and hepatic necrosis (with or without immune complexes), fulminant hepatitis (sometimes leading to liver transplantation), parapsoriasis varioliformis acuta (Mucha-Haberman syndrome), rhabdomyolysis, photosensitization, arthralgia, periorbital edema, conjunctival and scleral injection, alopecia, and interstitial lung disease.
Anaphylaxis was reported during postmarketing experience with the use of products containing or metabolized to mesalamine.[Ref]
Renal
Frequency not reported: Toxic nephrosis with oliguria and anuria, nephritis, hemolytic uremic syndrome, bilateral renal calculi composed of acetylsulfapyridine, proteinase 3-ANCA positive necrotizing glomerulonephritis
Postmarketing reports: Nephrolithiasis, nephrotic syndrome, interstitial nephritis[Ref]
At least 1 patient developed bilateral renal calculi composed of acetylsulfapyridine, a metabolite of sulfasalazine.[Ref]
Endocrine
Rare (less than 0.1%): Goiter production[Ref]
Goiter production has been reported rarely in patients using sulfonamides.[Ref]
More about Sulfazine (sulfasalazine)
- Check interactions
- Compare alternatives
- Reviews (12)
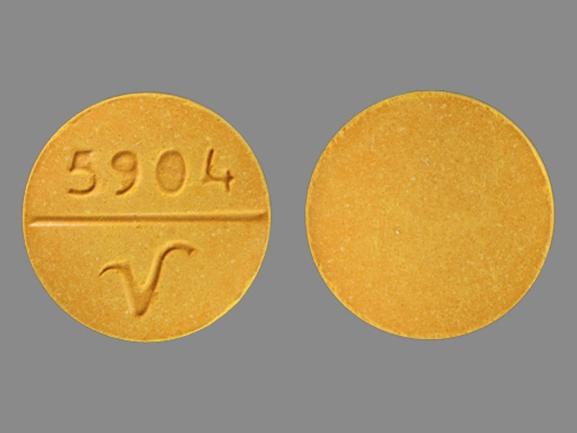
- Drug images
- Dosage information
- During pregnancy
- Drug class: 5-aminosalicylates
- Breastfeeding
Patient resources
Other brands
Azulfidine, Azulfidine EN-tabs
Professional resources
Other brands
Azulfidine, Azulfidine EN-tabs
Related treatment guides
References
1. Peppercorn MA. Sulfasalazine. Pharmacology, clinical use, toxicity, and related new drug development. Ann Intern Med. 1984;101:377-86.
2. Pokorney BH, Nichols TW, Jr. Pseudomembranous colitis. A complication of sulfasalazine therapy in a patient with Crohn's colitis. Am J Gastroenterol. 1981;76:374-6.
3. Ring FA, Hershfield NB, Machin GA, Scott RB. Sulfasalazine-induced colitis complicating idiopathic ulcerative colitis. Can Med Assoc J. 1984;131:43-5.
4. Taffet SL, Das KM. Sulfasalazine. Adverse effects and desensitization. Dig Dis Sci. 1983;28:833-42.
5. Werlin SL, Grand RJ. Bloody diarrhea--a new complication of sulfasalazine. J Pediatr. 1978;92:450-1.
6. Schwartz AG, Targan SR, Saxon A, Weinstein WM. Sulfasalazine-induced exacerbation of ulcerative colitis. N Engl J Med. 1982;306:409-12.
7. Faintuch J, Mott CB, Machado MC. Pancreatitis and pancreatic necrosis during sulfasalazine therapy. Int Surg. 1985;70:271-2.
8. Marcus RW. Sulfasalazine induced taste disturbances. J Rheumatol. 1991;18:634-5.
9. Nielsen OH. Sulfasalazine intolerance. A retrospective survey of the reasons for discontinuing treatment with sulfasalazine in patients with chronic inflammatory bowel disease. Scand J Gastroenterol. 1982;17:389-93.
10. Rubin R. Sulfasalazine-induced fulminant hepatic failure and necrotizing pancreatitis. Am J Gastroenterol. 1994;89:789-91.
11. Product Information. Azulfidine (sulfasalazine). Pharmacia and Upjohn. 2001;PROD.
12. Ward MM, Kuzis S. Medication toxicity among patients with ankylosing spondylitis. Arthritis Rheum. 2002;47:234-41.
13. Cantarini L, Tinazzi I, Biasi D, Fioravanti A, Galeazzi M. Sulfasalazine-induced immune thrombocytopenia. Postgrad Med J. 2007;83:e1.
14. Rashidi T, Mahd AA. Treatment of persistent alopecia areata with sulfasalazine. Int J Dermatol. 2008;47:850-2.
15. Mut SE, Kutlu G, Ucler S, Erdal A, Inan LE. Reversible encephalopathy due to sulfasalazine. Clin Neuropharmacol. 2008;31:368-71.
16. Drugs for rheumatoid arthritis. Treat Guidel Med Lett. 2009;7:37-46.
17. Schoonjans R, Mast A, Van Den Abeele G, Dewilde D, Achten E, Van Maele V, Pauwels W. Sulfasalazine-associated encephalopathy in a patient with Crohn's disease. Am J Gastroenterol. 1993;88:1416-20.
18. Olenginski TP, Harrington TM, Carlson JP. Transverse myelitis secondary to sulfasalazine. J Rheumatol. 1991;18:304.
19. Skeith KJ, Russell AS. Adverse reaction to sulfasalazine. J Rheumatol. 1988;15:529-30.
20. Alloway JA, Mitchell SR. Sulfasalazine neurotoxicity: a report of aseptic meningitis and a review of the literature. J Rheumatol. 1993;20:409-11.
21. Hill ME, Gordon C, Situnayake RD, Heath DA. Sulfasalazine induced seizures and dysphasia. J Rheumatol. 1994;21:748-9.
22. Norden DK, Lichtenstein GR, Williams WV. Sulfasalazine-induced myopathy. Am J Gastroenterol. 1994;89:801-2.
23. Pearl RK, Nelson RL, Prasad ML, Orsay CP, Abcarian H. Serious complications of sulfasalazine. Dis Colon Rectum. 1986;29:201-2.
24. Kaplan S, Mcdonald E, Marino C. Lichen planus in patients with rheumatoid arthritis treated with sulfasalazine. J Rheumatol. 1995;22:191-2.
25. Jullien D, Wolkenstein P, Roupie E, Roujeau JC, Revuz J. Toxic epidermal necrolysis after sulfasalazine treatment of mild psoriatic arthritis: warning on the use of sulfasalazine for a new indication. Arthritis Rheum. 1995;38:573.
26. Carr-Locke DL. Sulfasalazine-induced lupus syndrome in a patient with Crohn's disease. Am J Gastroenterol. 1982;77:614-6.
27. Clementz GL, Dolin BJ. Sulfasalazine-induced lupus erythematosus. Am J Med. 1988;84:535-8.
28. Siam AR, Hammoudeh M. Sulfasalazine induced systemic lupus erythematosus in a patient with rheumatoid arthritis. J Rheumatol. 1993;20:207.
29. Caulier M, Dromer C, Andrieu V, Leguennec P, Fournie B. Sulfasalazine induced lupus in rheumatoid arthritis. J Rheumatol. 1994;21:750-1.
30. Leroux JL, Ghezail M, Chertok P, Blotman F. Hypersensitivity reactions to sulfasalazine: skin rash, fever, hepatitis and activated lymphocytes. Clin Exp Rheumatol. 1992;10:427.
31. Kanner RS, Tedesco FJ, Kalser MH. Azulfidine- (sulfasalazine-) induced hepatic injury. Am J Dig Dis. 1978;23:956-8.
32. Losek JD, Werlin SL. Sulfasalazine hepatotoxicity. Am J Dis Child. 1981;135:1070-2.
33. Fich A, Schwartz J, Braverman D, Zifroni A, Rachmilewitz D. Sulfasalazine hepatotoxicity. Am J Gastroenterol. 1984;79:401-2.
34. Ribe J, Benkov KJ, Thung SN, Shen SC, LeLeiko NS. Fatal massive hepatic necrosis: a probable hypersensitivity reaction to sulfasalazine. Am J Gastroenterol. 1986;81:205-8.
35. Poland GA, Love KR. Marked atypical lymphocytosis, hepatitis, and skin rash in sulfasalazine drug allergy. Am J Med. 1986;81:707-8.
36. Sotolongo RP, Neefe LI, Rudzki C, Ishak KG. Hypersensitivity reaction to sulfasalazine with severe hepatotoxicity. Gastroenterology. 1978;75:95-9.
37. Haines JD, Jr. Hepatotoxicity after treatment with sulfasalazine. Postgrad Med. 1986;79:193-4,.
38. Marinos G, Riley J, Painter DM, McCaughan GW. Sulfasalazine-induced fulminant hepatic failure. J Clin Gastroenterol. 1992;14:132-5.
39. Namias A, Bhalotra R, Donowitz M. Reversible sulfasalazine-induced granulomatous hepatitis. J Clin Gastroenterol. 1981;3:193-8.
40. Gremse DA, Bancroft J, Moyer MS. Sulfasalazine hypersensitivity with hepatotoxicity, thrombocytopenia, and erythroid hypoplasia. J Pediatr Gastroenterol Nutr. 1989;9:261-3.
41. Cerner Multum, Inc. UK Summary of Product Characteristics.
42. Kuipers EJ, Vellenga E, de Wolf JT, Hazenberg BP. Sulfasalazine induced agranulocytosis treated with GM-CSF. J Rheumatol. 1992;19:621-2.
43. Youssef PP, Bertouch JV. Sulphasalazine induced aplastic anaemia. Aust N Z J Med. 1992;22:391-2.
44. Keisu M, Ekman E. Sulfasalazine associated agranulocytosis in sweden 1972-1989: clinical features, and estimation of its incidence. Eur J Clin Pharmacol. 1992;43:215-8.
45. Jacobson IM, Kelsey PB, Blyden GT, Demirjian ZN, Isselbacher KJ. Sulfasalazine-induced agranulocytosis. Am J Gastroenterol. 1985;80:118-21.
46. Wheelan KR, Cooper B, Stone MJ. Multiple haematologic abnormalities associated with sulfasalazine. Ann Intern Med. 1982;97:726-7.
47. Pena JM, Gonzalez-Garcia JJ, Garcia-Alegria J, Barbado FJ, Vazquez JJ. Thrombocytopenia and sulfasalazine. Ann Intern Med. 1985;102:277-8.
48. Davies GE, Palek J. Selective erythroid and magakaryocytic aplasia after sulfasalazine administration. Arch Intern Med. 1980;140:1122.
49. Rospond RM, Glowacki RC, Mailliard JA. Sargramostim for sulfasalazine-induced agranulocytosis. Clin Pharm. 1993;12:179.
50. Dery CL, Schwinghammer TL. Agranulocytosis associated with sulfasalazine. Drug Intell Clin Pharm. 1988;22:139-42.
51. Guillemin F, Aussedat R, Guerci A, Lederlin P, Trechot P, Pourel J. Fatal agranulocytosis in sulfasalazine treated rheumatoid arthritis. J Rheumatol. 1989;16:1166-7.
52. Mitrane MP, Singh A, Seibold JR. Cholestasis and fatal agranulocytosis complicating sulfasalazine therapy: case report and review of the literature. J Rheumatol. 1986;13:969-72.
53. Canvin JM, el-Gabalawy HS, Chalmers IM. Fatal agranulocytosis with sulfasalazine therapy in rheumatoid arthritis. J Rheumatol. 1993;20:909-10.
54. Mechanick JI. Coombs' positive hemolytic anemia following sulfasalazine therapy in ulcerative colitis: case reports, review, and discussion of pathogenesis. Mt Sinai J Med. 1985;52:667-70.
55. Gales BJ, Gales MA. Granulocyte-colony stimulating factor for sulfasalazine-induced agranulocytosis. Ann Pharmacother. 1993;27:1052-4.
56. Jick H, Myers MW, Dean AD. The risk of sulfasalazine- and mesalazine-associated blood disorders. Pharmacotherapy. 1995;15:176-81.
57. Teplitsky V, Virag I, Halabe A. Drug points - Immune complex haemolytic anaemia associated with sulfasalazine. Br Med J. 2000;320:1113.
58. Baillie J. Sulfasalazine and pulmonary infiltrates. Am J Gastroenterol. 1984;79:77.
59. Yaffe BH, Korelitz BI. Sulfasalazine pneumonitis. Am J Gastroenterol. 1983;78:493-4.
60. Averbuch M, Halpern Z, Hallak A, Topilsky M, Levo Y. Sulfasalazine pneumonitis. Am J Gastroenterol. 1985;80:343-5.
61. Gabazza EC, Taguchi O, Yamakami T, Machishi M, Ibata H, Suzuki S, Matsumoto K, Kitagawa T, Yamamoto J. Pulmonary infiltrates and skin pigmentation associated with sulfasalazine. Am J Gastroenterol. 1992;87:1654-7.
62. Hamadeh MA, Atkinson J, Smith LJ. Sulfasalazine-induced pulmonary disease. Chest. 1992;101:1033-7.
63. Williams T, Eidus L, Thomas P. Fibrosing alveolitis, bronchiolitis obliterans, and sulfasalazine therapy. Chest. 1982;81:766-8.
64. Valcke Y, Pauwels R, Van der Straeten M. Bronchoalveolar lavage in acute hypersensitivity pneumonitis caused by sulfasalazine. Chest. 1987;92:572-3.
65. Moseley RH, Barwick KW, Dobuler K, DeLuca VA, Jr. Sulfasalazine-induced pulmonary disease. Dig Dis Sci. 1985;30:901-4.
66. Wang KK, Bowyer BA, Fleming CR, Schroeder KW. Pulmonary infiltrates and eosinophilia associated with sulfasalazine. Mayo Clin Proc. 1984;59:343-6.
67. Sullivan SN. Sulfasalazine lung. Desensitization to sulfasalazine and treatment with acrylic coated 5-ASA and azodisalicylate. J Clin Gastroenterol. 1987;9:461-3.
68. Miura N, Aoyama R, Kitagawa W, Yamada H, Nishikawa K, Imai H. Proteinase 3-antineutrophil cytoplasmic antibody-(PR3-ANCA) positive necrotizing glomerulonephritis after restarting sulphasalazine treatment. Clin Nephrol. 2009;71:74-9.
69. Roujeau JC, Kelly JP, Naldi L, et al. Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. N Engl J Med. 1995;333:1600-7.
70. Kawada A, Kobayashi T, Noguchi H, Hiruma M, Ishibashi A, Marshall J. Fixed drug eruption induced by sulfasalazine. Contact Dermatitis. 1996;34:155-6.
71. Kounis GN, Kouni SA, Chiladakis JA, Kounis NG. Comment: Mesalamine-Associated Hypersensitivity Myocarditis in Ulcerative Colitis and the Kounis Syndrome (February). Ann Pharmacother. 2009;43:393-4.
72. De Greef E, Mennie K, Muise A. Drug reaction with eosinophilia and systemic symptoms. CMAJ. 2010;182:481.
73. Dwarakanath AD, Michael J, Allan RN. Sulphasalazine-induced renal failure. Gut. 1992;33:1006-7.
74. Erturk E, Casemento JB, Guertin KR, Kende AS. Bilateral acetylsulfapyridine nephrolithiasis associated with chronic sulfasalazine therapy. J Urol. 1994;151:1605-6.
75. Chatzinoff M, Guarino JM, Corson SL, Batzer FR, Friedman LS. Sulfasalazine-induced abnormal sperm penetration assay reversed on changing to 5-aminosalicylic acid enemas. Dig Dis Sci. 1988;33:108-10.
76. Ireland A, Jewell DP. Sulfasalazine-induced impotence: a beneficial resolution with olsalazine?. J Clin Gastroenterol. 1989;11:711.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.