Pacerone Side Effects
Generic name: amiodarone
Medically reviewed by Drugs.com. Last updated on Nov 11, 2023.
Note: This document contains side effect information about amiodarone. Some dosage forms listed on this page may not apply to the brand name Pacerone.
Applies to amiodarone: oral tablet. Other dosage forms:
Warning
Oral route (Tablet)
Amiodarone oral tablet is intended for use only in patients with the indicated life-threatening arrhythmias because its use is accompanied by substantial toxicity. Amiodarone can cause pulmonary toxicity (hypersensitivity pneumonitis or interstitial/alveolar pneumonitis) that has resulted in clinically manifest disease at rates as high as 17% in some series of patients. Pulmonary toxicity has been fatal about 10% of the time. Obtain a baseline chest X-ray and pulmonary-function tests, including diffusion capacity, when therapy is initiated. Repeat history, physical exam, and chest X-ray every 3 to 6 months. Amiodarone can cause hepatoxicity, which can be fatal. Obtain baseline and periodic liver transaminases and discontinue or reduce dose if the increase exceeds three times normal, or doubles in a patient with an elevated baseline. Discontinue if the patient experiences signs or symptoms of clinical liver injury. Amiodarone can exacerbate arrhythmias. Initiate in a clinical setting where continuous electrocardiograms and cardiac resuscitation are available.
Serious side effects of Pacerone
Along with its needed effects, amiodarone (the active ingredient contained in Pacerone) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking amiodarone:
More common
- Cough
- dizziness, lightheadedness, or fainting
- fever (slight)
- numbness or tingling in the fingers or toes
- painful breathing
- sensitivity of the skin to sunlight
- trembling or shaking of the hands
- trouble with walking
- unusual and uncontrolled movements of the body
- weakness of the arms or legs
Less common
- Blue-gray coloring of the skin on the face, neck, and arms
- blurred vision or blue-green halos seen around objects
- coldness
- dry eyes
- dry, puffy skin
- fast or irregular heartbeat
- nervousness
- pain and swelling in the scrotum
- sensitivity of the eyes to light
- sensitivity to heat
- slow heartbeat
- sweating
- swelling of the feet or lower legs
- trouble with sleeping
- unusual tiredness
- weight gain or loss
Rare
- Skin rash
- yellow eyes or skin
Incidence not known
- Agitation
- back, leg, or stomach pains
- bleeding gums
- blistering, peeling, or loosening of the skin
- bloating
- blood in the urine
- bloody, black, or tarry stools
- blue lips, fingernails, or skin
- blurred or double vision
- chest pain
- chills
- clay-colored stools
- confusion
- confusion as to time, place, or person
- coughing or spitting up blood
- cracks in the skin
- dark urine
- decreased awareness or responsiveness
- decreased urine output
- depression
- diarrhea
- difficult or labored breathing
- difficult urination
- dry cough
- eye pain
- fast heartbeat
- general body swelling
- high fever
- holding false beliefs that cannot be change by facts
- hostility
- inability to have or keep an erection
- indigestion
- irregular, fast or slow, or shallow breathing
- irritability
- itching
- joint or muscle pain
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or genitals
- loss in sexual ability, desire, drive, or performance
- loss of consciousness
- loss of heat from the body
- lower back or side pain
- mood or mental change
- muscle cramps, spasms, twitching, pain, or stiffness
- no breathing
- noisy breathing
- nosebleeds
- pain in the abdomen, groin, or scrotum
- pain or burning with urination
- pains in the stomach, side, or abdomen, possibly radiating to the back
- pale skin
- pinpoint red spots on the skin
- rapid weight gain
- red skin lesions, often with a purple center
- red, irritated eyes
- red, swollen skin
- scaly skin
- seeing, hearing, or feeling things that are not there
- seizures
- severe headache
- severe sleepiness
- sneezing
- sore throat
- sores, ulcers, or white spots on the lips or in mouth
- stomach pain
- swelling of the face, ankles, or hands
- swelling of the scrotum
- swollen or painful glands
- tightness in the chest
- troubled breathing
- unpleasant breath odor
- unusual bleeding or bruising
- unusual drowsiness, dullness, tiredness, weakness or feeling of sluggishness
- unusual excitement, nervousness, or restlessness
- vomiting of blood
Other side effects of Pacerone
Some side effects of amiodarone may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Constipation
- headache
- loss of appetite
- nausea
- vomiting
Less common
- Bitter or metallic taste
- decrease in sexual interest
- decreased sexual ability in males
- feeling of warmth
- redness of the face, neck, arms and occasionally, upper chest
For Healthcare Professionals
Applies to amiodarone: compounding powder, intravenous solution, oral tablet.
General
The most common adverse reactions were corneal microdeposits, hypotension, and photosensitivity.[Ref]
Cardiovascular
Very common (10% or more): Hypotension (up to 20.2%)
Common (1% to 10%): Bradycardia, blood pressure decreased, congestive heart failure, heart arrest, ventricular tachycardia, cardiac arrhythmia, sinoatrial node dysfunction, flushing
Uncommon (0.1% to 1%): Conduction disturbances
Very rare (less than 0.01%): Marked bradycardia, sinus arrest, vasculitis, hot flushes
Frequency not reported: Torsade de pointes, collapse, atrial fibrillation, nodal arrhythmia, QT interval prolonged, sinus bradycardia, ventricular fibrillation, shock, asystole, pulseless electrical activity, cardiogenic shock, atrioventricular block, severe hypotension
Postmarketing reports: Sinoatrial block, intraventricular conduction disorders, bundle branch block, infra-His block, ventricular extrasystole, antegrade conduction via an accessory pathway[Ref]
Hepatic
Common (1% to 10%): Acute liver disorders with high serum transaminases and/or jaundice including hepatic failure, liver function tests abnormal, nonspecific hepatic disorder
Very rare (less than 0.01%): Pseudo alcoholic hepatitis, cirrhosis, serum transaminases increased
Frequency not reported: ALT increased, AST increased
Postmarketing reports: Cholestatic hepatitis, cholestasis, jaundice, alkaline phosphatase increased, blood lactate dehydrogenase increased, hepatitis[Ref]
Respiratory
Common (1% to 10%): Pulmonary toxicity, pulmonary inflammation or fibrosis, adult respiratory distress syndrome
Very rare (less than 0.01%): Bronchospasm, interstitial pneumonitis, severe respiratory complications, apnea
Frequency not reported: Pulmonary hemorrhage, lung edema, respiratory disorder, alveolar pneumonitis
Postmarketing reports: Possibly fatal respiratory disorder, bronchiolitis obliterans organizing pneumonia, dyspnea, cough, hemoptysis, wheezing, hypoxia, pulmonary infiltrates, pulmonary mass, pleuritis, pulmonary phospholipidosis, pleural effusion, eosinophilic pneumonia, acute respiratory distress syndrome[Ref]
Ocular
Very common (10% or more): Corneal microdeposits (up to 90% or more)
Common (1% to 10%): Visual disturbance
Very rare (less than 0.01%): Optic neuropathy/neuritis
Frequency not reported: Permanent blindness, papilledema, corneal degeneration, eye discomfort, scotoma, lens opacities, macular degeneration, keratopathy, gritty eyes, itching, burning
Postmarketing reports: Visual field defect, blurred vision[Ref]
Dermatologic
Very common (10% or more): Photosensitivity (up to 10%)
Common (1% to 10%): Slate-gray or bluish pigmentations of light-exposed skin
Very rare (less than 0.01%): Erythema, rash, exfoliative dermatitis, alopecia, sweating
Frequency not reported: Granuloma, angioedema, urticaria, Stevens-Johnson syndrome, spontaneous ecchymosis, pustular psoriasis enhanced
Postmarketing reports: Toxic epidermal necrolysis, erythema multiforme, skin cancer, pruritus, bullous dermatitis, drug rash with eosinophilia and systemic symptoms (DRESS), eczema[Ref]
Nervous system
Common (1% to 10%): Extrapyramidal symptoms, extrapyramidal tremor, tremor/abnormal involuntary movement, lack of coordination, gait abnormal/ataxia, dizziness, paresthesia, headache, abnormal taste and smell
Uncommon (0.1% to 1%): Peripheral sensorimotor neuropathy
Very rare (less than 0.01%): Cerebellar ataxia, benign intracranial hypertension, vertigo
Frequency not reported: Peripheral neuropathy, demyelinating polyneuropathy, nerve conduction abnormal, neurolipidosis, neuromyopathy, parosmia
Postmarketing reports: Confusional state, disorientation, delirium, intracranial pressure increased, hypoesthesia, Parkinsonian symptoms[Ref]
Psychiatric
Common (1% to 10%): Nightmare, sleep disorders, libido decreased, insomnia, sleep disturbance
Frequency not reported: Vivid dreams, chronic anxiety
Postmarketing reports: Hallucination[Ref]
Gastrointestinal
Common (1% to 10%): Nausea, constipation, abdominal pain, salivation abnormal
Frequency not reported: Vomiting, dysgeusia, diarrhea
Postmarketing reports: Pancreatitis, acute pancreatitis, dry mouth[Ref]
Other
Common (1% to 10%): Fever, malaise, fatigue[Ref]
Endocrine
Very common (10% or more): Hypothyroidism (up to 10%)
Common (1% to 10%): Hyperthyroidism
Very rare (less than 0.01%): Syndrome of inappropriate antidiuretic hormone secretion
Frequency not reported: Thyroid function tests abnormal
Postmarketing reports: Thyroid nodules/cancer[Ref]
Metabolic
Common (1% to 10%): Anorexia, edema
Frequency not reported: Weight gain, symptomatic hypercalcemia, appetite decreased[Ref]
Hematologic
Common (1% to 10%): Coagulation abnormalities
Very rare (less than 0.01%): Hemolytic anemia, aplastic anemia, thrombocytopenia
Frequency not reported: Bone marrow granuloma, bone marrow depression
Postmarketing reports: Pancytopenia, neutropenia, agranulocytosis, granulocytosis[Ref]
Musculoskeletal
Common (1% to 10%): Muscle weakness
Frequency not reported: Back pain
Postmarketing reports: Myopathy, rhabdomyolysis, muscle spasm, lupus-like syndrome[Ref]
Local
Common (1% to 10%): Injection site reactions[Ref]
Genitourinary
Very rare (less than 0.01%): Epididymo-orchitis, impotence
Postmarketing reports: Epididymitis[Ref]
Immunologic
Very rare (less than 0.01%): Anaphylactic shock
Frequency not reported: Hypersensitivity reaction, positive antinuclear antibodies, immunoglobulin level increased
Postmarketing reports: Anaphylactic/anaphylactoid reaction[Ref]
Renal
Very rare (less than 0.01%): Blood creatinine increased
Frequency not reported: Kidney function abnormal, chronic renal failure worsened
Postmarketing reports: Renal impairment, renal insufficiency, acute renal failure[Ref]
More about Pacerone (amiodarone)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (4)
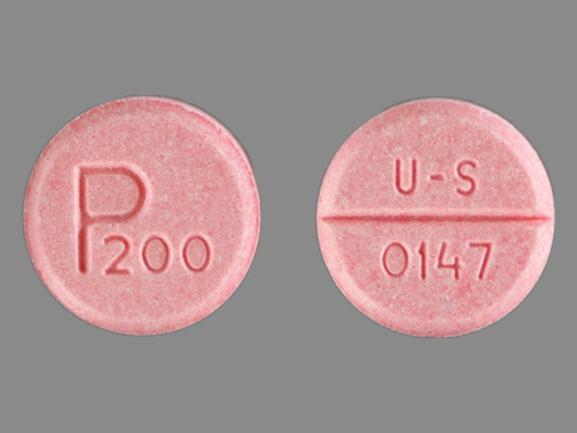
- Drug images
- Latest FDA alerts (4)
- Dosage information
- During pregnancy
- Drug class: group III antiarrhythmics
- Breastfeeding
- En español
Patient resources
Other brands
Cordarone, Nexterone, Cordarone IV
Professional resources
Other brands
Related treatment guides
References
1. Product Information. Cordarone (amiodarone). Wyeth-Ayerst Laboratories. 2002;PROD.
2. Product Information. Cordarone (amiodarone). Apothecon Inc. 2022.
3. Cerner Multum, Inc. UK Summary of Product Characteristics.
4. Cerner Multum, Inc. Australian Product Information.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.