Carbatrol Side Effects
Generic name: carbamazepine
Medically reviewed by Drugs.com. Last updated on Feb 27, 2024.
Note: This document contains side effect information about carbamazepine. Some dosage forms listed on this page may not apply to the brand name Carbatrol.
Applies to carbamazepine: oral capsule extended release, oral suspension, oral tablet, oral tablet chewable, oral tablet extended release.
Warning
Oral route (Tablet; Tablet, Chewable; Suspension; Tablet, Extended Release; Capsule, Extended Release)
Serious and sometimes fatal dermatologic reactions (including Stevens-Johnson syndrome and toxic epidermal necrolysis) have been reported, especially in patients with the inherited allelic variant HLA-B*1502. Screen genetically at-risk patients prior to receiving carbamazepine. Do not start carbamazepine in patients who test positive for the allele unless the benefit clearly outweighs the risk. Discontinue if you suspect that the patient has a serious dermatologic reaction. Aplastic anemia and agranulocytosis have also been reported. Obtain pretreatment hematological testing and periodically monitor CBC. Consider drug discontinuation if significant bone marrow depression develops.
Serious side effects of Carbatrol
Along with its needed effects, carbamazepine (the active ingredient contained in Carbatrol) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking carbamazepine:
More common
- Blurred vision or double vision
- continuous back-and-forth eye movements
Less common
- Actions that are out of control
- behavioral changes (especially in children)
- confusion, agitation, or hostility (especially in the elderly)
- diarrhea (severe)
- discouragement
- drooling
- fear
- feeling of unreality
- feeling sad or empty
- headache (continuing)
- increase in seizures
- irritability
- lack of appetite
- loss of balance control
- loss of interest or pleasure
- muscle trembling, jerking, or stiffness
- nausea (severe)
- other problems with muscle control or coordination
- sense of detachment from self or body
- shakiness and unsteady walk
- shuffling walk
- stiffness of the arm or leg
- sudden, wide mood swings
- talking, feeling, and acting with excitement
- thoughts or attempts of killing oneself
- tiredness
- trouble concentrating
- trouble sleeping
- twisting movements of the body
- uncontrolled movements, especially of the face, neck, and back
- unusual drowsiness
- vomiting (severe)
Rare
- Black, tarry stools
- blood in the urine or stools
- bone or joint pain
- chest pain or tightness
- cough
- darkening of the urine
- difficulty with speaking or slurred speech
- fainting
- frequent urination
- hoarseness
- irregular, pounding, or unusually slow heartbeat
- lower back or side pain
- mental depression with restlessness and nervousness or other mood or mental changes
- muscle or stomach cramps
- nosebleeds or other unusual bleeding or bruising
- numbness, tingling, pain, or weakness in the hands and feet
- pain, tenderness, swelling, or bluish color in the leg or foot
- painful or difficult urination
- pale stools
- pinpoint red spots on the skin
- rapid weight gain
- rigidity
- ringing, buzzing, or other unexplained sounds in the ears
- skin rash, hives, or itching
- sores, ulcers, or white spots on the lips or in the mouth
- swelling of the face, hands, feet, or lower legs
- swollen or painful glands
- sudden decrease in the amount of urine
- trembling
- trouble breathing
- uncontrolled body movements
- unusual tiredness or weakness
- visual hallucinations (seeing things that are not there)
- yellow eyes or skin
Incidence not known
- Blistering, peeling, or loosening of the skin
- chills
- decreased urine output
- dilated neck veins
- extreme tiredness or weakness
- general feeling of discomfort or illness
- irregular breathing
- irregular heartbeat
- joint or muscle pain
- red skin lesions, often with a purple center
- red, irritated eyes
- sore throat
- swelling of the face, fingers, feet, or lower legs
- thickening of bronchial secretions
- unusual bleeding or bruising
- weight gain
Other side effects of Carbatrol
Some side effects of carbamazepine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Dizziness (mild)
- drowsiness (mild)
- lightheadedness
- nausea (mild)
- vomiting (mild)
Incidence not known
- Accidental injury
- aching joints or muscles
- back pain
- belching
- constipation
- dryness of the mouth
- headache
- heartburn
- increased sensitivity of the skin to sunlight (skin rash, itching, redness or other discoloration of the skin, or severe sunburn)
- increased sweating
- indigestion
- irritation or soreness of the tongue or mouth
- lack or loss of strength
- loss of hair
- loss of memory
- problems with memory
- sexual problems in males
- sleepiness
- stomach pain, upset, or discomfort
For Healthcare Professionals
Applies to carbamazepine: compounding powder, intravenous solution, oral capsule extended release, oral suspension, oral tablet, oral tablet chewable, oral tablet extended release.
Gastrointestinal
Very common (10% or more): Nausea (29%), vomiting (18%), constipation (10%)
Very rare (less than 0.01%): Colitis, glossitis, stomatitis, pancreatitis
Frequency not reported: Dryness of the mouth, with suppositories occasional rectal irritation may occur, diarrhea, oral ulceration
Postmarketing reports: Gastric distress, abdominal pain, anorexia[Ref]
Endocrine
Carbamazepine (the active ingredient contained in Carbatrol) increases the rate of T4 and T3 metabolism and may lead to hypothyroidism in patients with hypothyroidism who are being treated with T4. Carbamazepine may also cause a 20% to 40% decrease in serum total and free T4 concentrations and a smaller decrease in serum total and free T3 concentrations in patients who have no thyroid disease.[Ref]
Very rare (less than 0.01%): Increase in prolactin (with or without symptoms such as gynecomastia or galactorrhea), impaired male fertility and/or abnormal spermatogenesis, abnormal thyroid function tests (e.g., decreased L-thyroxine [FT4, T4, T3] and increased TSH)
Frequency not reported: Lower serum testosterone, lower free androgen indexes, increased cerebrospinal fluid thyrotropin-releasing hormone levels[Ref]
Hematologic
Very common (10% or more): Leucopenia
Common (1% to 10%): Eosinophilia, thrombocytopenia, neutropenia
Rare (0.01% to 0.1%): Leukocytosis, lymphadenopathy, folic acid deficiency
Very rare (less than 0.01%): Agranulocytosis, aplastic anemia, pure red cell aplasia, megaloblastic anemia, acute intermittent porphyria, reticulocytosis, hemolytic anemia
Frequency not reported: Aplastic anemia, pancytopenia, bone marrow depression, leukopenia, thrombophlebitis, thromboembolism, adenopathy[Ref]
Thrombocytopenia is the most common hematologic effect of carbamazepine and may be either mild and transient or severe. Significant decreases in white blood cell counts may occur although the values may still be within the normal range. Often counts will return to baseline during continued therapy, and therefore, discontinuation of carbamazepine may not be necessary. Dose reductions may also result in normalization of white blood cell counts. Aplastic anemia has been reported (although many of the reported cases had confounding exposures to other medications). The manufacturer reports an incidence of 2 per 1,000,000 patients for aplastic anemia and 6 per 1,000,000 patients for agranulocytosis. Cases of reticulocytosis have been reported rarely in association with carbamazepine therapy as well. In addition, cases of hemolytic anemia and erythroid arrest have been reported.
Both humoral and nonimmune mechanisms have been implicated in the etiology of carbamazepine-induced bone marrow suppression.[Ref]
Cardiovascular
Rare (0.01% to 0.1%): Disturbances of cardiac conduction
Very rare (less than 0.01%): Bradycardia, arrhythmias, AV-block with syncope, collapse, congestive heart failure, hypertension or hypotension, aggravation of coronary artery disease, thrombophlebitis, thromboembolism
Frequency not reported: Edema[Ref]
Most of the cases of cardiovascular effects reported have occurred in patients receiving carbamazepine for trigeminal neuralgia. The reported effects included congestive heart failure, edema, hypotension, syncope and arrhythmias. In general, the doses were titrated quickly because of severe pain. Many of the doses were higher than those used to treat epilepsy. Many of the reported cardiovascular effects resolved after discontinuation of carbamazepine.[Ref]
Nervous system
Rigidity and oculogyric crises have been reported. Impairment of psychomotor function has been noted in association with use of the liquid suspension of carbamazepine (the active ingredient contained in Carbatrol) Additionally, impaired cognition, exacerbations of focal seizures and asterixis have been reported in association with carbamazepine treatment. One case of a lingual-facial-buccal extrapyramidal reaction has also been described.
One study has suggested that gradual withdrawal of carbamazepine over ten days results in significantly fewer generalized tonic-clonic seizures compared to rapid withdrawal over four days.
One study has suggested that the epoxide metabolite of carbamazepine may be responsible for the occasional occurrence of seizure exacerbations in patients receiving carbamazepine.[Ref]
Very common (10% or more): Dizziness (44%), somnolence (32%), ataxia (15%)
Common (1% to 10%): Headache, tremor
Uncommon (0.1% to 1%): Abnormal involuntary movements (tremor, asterixis, dystonia, tics)
Rare (less than 0.1%): Choreoathetotic disorders, orofacial dyskinesia, oculomotor disturbances, speech disorders (e.g., dysarthria or slurred speech), peripheral neuritis, paresthesia, paretic symptoms, neuroleptic malignant syndrome
Frequency not reported: Drowsiness, fatigue, taste disturbances[Ref]
Hypersensitivity
Rash and pruritus often resolve after discontinuation of carbamazepine (the active ingredient contained in Carbatrol) therapy. Both cases of lupus-like syndrome resolved after discontinuation of carbamazepine. Stevens-Johnson syndrome, erythema multiforme, and a mononucleosis-like syndrome have also been reported.[Ref]
Rare (0.01% to 0.1%): A delayed multi-organ hypersensitivity disorder (of serum sickness type) with fever, skin rashes, vasculitis, lymphadenopathy, disorders mimicking lymphoma, arthralgia, leucopenia, eosinophilia, hepato-splenomegaly and abnormal liver function tests, occurring in various combinations, other organs may also be affected (e.g., lungs, kidneys, pancreas, myocardium, colon)
Very rare (less than 0.01%): Aseptic meningitis (with myoclonus and peripheral eosinophilia), anaphylactic reaction, angioedema
Frequency not reported: Multiorgan hypersensitivity reactions occurring days, weeks, or months after initiating treatment[Ref]
Hepatic
Very common (10% or more): Elevated gamma-GT (due to hepatic enzyme induction) usually not clinically relevant
Common (1% to 10%): Elevated alkaline phosphatase
Uncommon (0.1% to 1%): Elevated transaminases
Rare (0.01% to 0.1%): Cholestatic and hepatocellular jaundice, hepatitis of cholestatic, parenchymal (hepatocellular), or mixed type
Very rare (less than 0.01%): Granulomatous hepatitis, hepatic failure
Frequency not reported: Liver function test abnormalities, variegate porphyria, porphyria cutanea tarda[Ref]
Alterations in liver function tests may progress to hepatotoxicity including cholangitis, granuloma formation, fever and hepatocellular necrosis. Discontinuation of carbamazepine often results in improvement in laboratory abnormalities and liver injury.[Ref]
Renal
Very rare (less than 0.01%): Interstitial nephritis, renal failure, renal dysfunction (including albuminuria, hematuria, oliguria, and elevated BUN/azotemia)[Ref]
Respiratory
Very rare (less than 0.01%): Pulmonary hypersensitivity (characterized by fever, dyspnea, pneumonitis or pneumonia), pulmonary embolism[Ref]
Dermatologic
Very common (10% or more): Allergic skin reactions, urticaria
Common (1% to 10%): Pruritus, rash, paresthesia
Uncommon (0.1% to 1%): Exfoliative dermatitis, erythroderma
Rare (0.01% to 0.1%): Systemic lupus erythematosus-like syndrome
Very rare (less than 0.01%): Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), photosensitivity, erythema multiforme, erythema nodosum, alterations in skin pigmentation, purpura, acne, sweating, alopecia, hirsutism, unusual bruising, pruritic and erythematous rashes, diaphoresis, onychomycosis, dermatitis
Frequency not reported: Psoriasiform eruption[Ref]
Dangerous, sometimes fatal skin reactions (Stevens Johnson syndrome and toxic epidermal necrolysis), that can be caused by carbamazepine therapy are significantly more common in patients with the human leukocyte antigen (HLA) allele, HLA-B 1502. This allele occurs almost exclusively in patients with ancestry across broad areas of Asia, including South Asian Indians. Patients with ancestry from areas in which HLA-B 1502 is present should be screened for the HLA-B 1502 allele before starting treatment with carbamazepine. If these individuals test positive, carbamazepine should not be started unless the expected benefit clearly outweighs the increased risk of serious skin reactions. Patients who have been taking carbamazepine for more than a few months without developing skin reactions are at low risk of these events ever developing from carbamazepine. This is true for patients of any ethnicity or genotype, including patients who test positive for HLA-B 1502.[Ref]
Ocular
Common (1% to 10%): Diplopia, accommodation disorders (blurred vision)
Very rare (less than 0.01%): Lens opacities, conjunctivitis
Postmarketing reports: Diplopia, oculomotor disturbances, nystagmus, photosensitivity, visual hallucinations, scattered punctate cortical lens opacities, overall impairment of the chromatic and achromatic systems, increased intraocular pressure[Ref]
Oncologic
Frequency not reported: Disorders mimicking lymphoma[Ref]
Immunologic
Frequency not reported: Antibody deficiency, hypogammaglobulinemia
Postmarketing reports: Aseptic meningitis (with myoclonus and peripheral eosinophilia)[Ref]
Psychiatric
Euphoria has also been reported and has led to abuse of carbamazepine (the active ingredient contained in Carbatrol) in some patients[Ref]
Common (1% to 10%): Abnormal thinking
Rare (0.01% to 0.1%): Hallucinations (visual or acoustic), depression, loss of appetite, restlessness, aggressive behavior, agitation, confusion, talkativeness
Very rare (less than 0.01%): Activation of psychosis, rebound mania following discontinuation of therapy
Frequency not reported: Euphoria, abuse[Ref]
Genitourinary
Very rare (less than 0.01%): Sexual disturbances/impotence, abnormal spermatogenesis (with decreased sperm count and/or motility)
Frequency not reported: Urinary frequency, acute urinary retention, oliguria with elevated blood pressure, azotemia, albuminuria, glycosuria, elevated BUN, microscopic deposits in the urine[Ref]
Metabolic
Common (1% to 10%): Hyponatremia, fluid retention, edema, weight gain, reduced plasma osmolarity due to an antidiuretic hormone (ADH)-like effect (leading in rare cases to water intoxication accompanied by lethargy)
Very rare (less than 0.01%): Elevated cholesterol (including HDL cholesterol), elevated triglycerides[Ref]
Musculoskeletal
Rare (0.01% to 0.1%): Muscle weakness
Very rare (less than 0.01%): Arthralgia
Frequency not reported: Osteoporosis, disturbances of bone metabolism (decrease in plasma calcium and 25-OH-cholecalciferol) leading to osteomalacia, decreased levels of plasma calcium[Ref]
Other
Common (1% to 10%): Vertigo
Very rare (less than 0.01%): Tinnitus, hyperacusis, hypoacusis, changes in pitch perception
Frequency not reported: Fever and chills[Ref]
More about Carbatrol (carbamazepine)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (14)
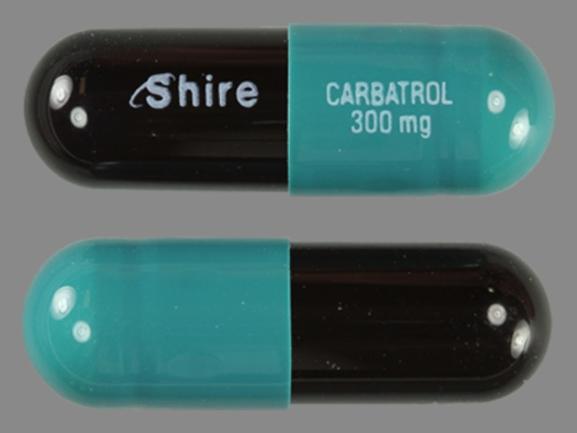
- Drug images
- Dosage information
- During pregnancy
- Generic availability
- Drug class: dibenzazepine anticonvulsants
- Breastfeeding
- En español
Patient resources
Other brands
Tegretol, Tegretol XR, Equetro, Epitol, Carnexiv
Professional resources
Other brands
Tegretol, Equetro, Epitol, Carnexiv
Related treatment guides
References
1. Pellock JM. Carbamazepine side effects in children and adults. Epilepsia. 1987;28:s64-70.
2. Soman M, Swenson C. A possible case of carbamazepine-induced pancreatitis. Drug Intell Clin Pharm. 1985;19:925-7.
3. Product Information. Tegretol (carbamazepine). Novartis Pharmaceuticals. 2002;PROD.
4. Tsao CY, Wright FS. Acute chemical pancreatitis associated with carbamazepine intoxication. Epilepsia. 1993;34:174-6.
5. Hebert AA, Ralston JP. Cutaneous reactions to anticonvulsant medications. J Clin Psychiatry. 2001;62:22-6.
6. Cerner Multum, Inc. UK Summary of Product Characteristics.
7. Cerner Multum, Inc. Australian Product Information.
8. Kalff R, Houtkooper MA, Meyer JW, et al. Carbamazepine and serum sodium levels. Epilepsia. 1984;24:390-7.
9. Uhde TW, Post RM. Effects of carbamazepine on serum electrolytes: clinical and theoretical implications. J Clin Psychopharmacol. 1983;3:103-6.
10. Strandjord RE, AAnderud S, Myking OL, Johannessen SI. Influence of carbamazepine on serum thyroxine and triiodothyronine in patients with epilepsy. Acta Neurol Scand. 1981;63:111-21.
11. Isojarvi JI, Airaksinen KE, Repo M, Pakarinen AJ, Salmela P, Myllyla VV. Carbamazepine, serum thyroid hormones and myocardial function in epileptic patients. J Neurol Neurosurg Psychiatry. 1993;56:710-2.
12. Tormey WP. Mechanisms of carbamazepine-induced antidiuresis. J Neurol Neurosurg Psychiatry. 1993;56:567.
13. Kamiyama T, Iseki K, Kawazoe N, Takishita S, Fukiyama K. Carbamazepine-induced hyponatremia in a patient with partial central diabetes insipidus. Nephron. 1993;64:142-5.
14. Gandelman MS. Review of carbamazepine-induced hyponatremia. Prog Neuropsychopharmacol Biol Psychiatry. 1994;18:211-33.
15. Delzompo M, Bocchetta A, Loviselli A, Martino E, Post RM, Ketter TA. Thyroid function during carbamazepine. Biol Psychiatry. 1994;36:135-6.
16. Brewerton TD, Jackson CW. Prophylaxis of carbamazepine-induced hyponatremia by demeclocycline in 6 patients. J Clin Psychiatry. 1994;55:249-51.
17. Otto C, Richter WO. Syndrome of inappropriate antidiuretic hormone secretion induced by different drugs. Ann Pharmacother. 1994;28:1199-200.
18. Marangell LB, George MS, Bissette G, Pazzaglia P, Huggins T, Post RM. Carbamazepine increases cerebrospinal fluid thyrotropin-releasing hormone levels in affectively ill patients. Arch Gen Psychiatry. 1994;51:625-8.
19. Isojarvi JIT, Pakarinen AJ, Rautio A, Pelkonen O, Myllyla VV. Liver enzyme induction and serum lipid levels after replacement of carbamazepine with oxcarbazepine. Epilepsia. 1994;35:1217-20.
20. Verrotti A, Basciani F, Morresi S, Morgese G, Chiarelli F. Thyroid hormones in epileptic children receiving carbamazepine and valproic acid. Pediatr Neurol. 2001;25:43-6.
21. Kuz GM, Manssourian A. Carbamazepine-induced hyponatremia: assessment of risk factors. Ann Pharmacother. 2005;39:1943-6.
22. Lofgren E, Tapanainen JS, Koivunen R, Pakarinen A, Isojarvi JI. Effects of carbamazepine and oxcarbazepine on the reproductive endocrine function in women with epilepsy. Epilepsia. 2006;47:1441-6.
23. Sobotka JL, Alexander B, Cook BL. A review of carbamazepine's hematologic reactions and monitoring recommendations. DICP. 1990;24:1214-9.
24. Tohen M, Castillo J, Cole JO, et al. Thrombocytopenia associated with carbamazepine: a case series. J Clin Psychiatry. 1991;52:496-8.
25. Stroink AR, Skillrud DM, Kiely JM, Sundt TM Jr. Carbamazepine-induced hemolytic anemia. Acta Haematol. 1984;72:346-8.
26. Shoenfeld Y, Ben Baruch N, Livni E, et al. Carbamazepine (tegretol)-induced thrombocytopenia. Acta Haematol. 1982;68:74.
27. Medberry CA, Pappas AA, Ackerman BH. Carbamazepine and erythroid arrest. Drug Intell Clin Pharm. 1987;21:439-41.
28. Ponte CD. Carbamazepine-induced thrombocytopenia, rash, and hepatic dysfunction. Drug Intell Clin Pharm. 1983;17:642-4.
29. Baciewicz G, Yerevanian BI. Thrombocytopenia associated with carbamazepine: case report and review. J Clin Psychiatry. 1984;45:315-6.
30. Hawson GA, Bain BJ, Whyte I. Agranulocytosis after administration of carbamazepine. Med J Aust. 1980;Jan:82-3.
31. Rush JA, Beran RG. Leucopenia as an adverse reaction to carbamazepine therapy. Med J Aust. 1984;140:426-8.
32. Schweiger FJ, Kelton JG, Messner H, et al. Anticonvulsant-induced marrow suppression and immune thrombocytopenia. Acta Haematol. 1988;80:54-8.
33. Terao T. Reticulocyte increase and carbamazepine. Am J Psychiatry. 1993;150:1271-2.
34. Terao T. Transient thrombocytopenia while continuing carbamazepine. Am J Psychiatry. 1993;150:1750-1.
35. Levander HG. Granulomatous hepatitis in a patient receiving carbamazepine. Acta Med Scand. 1980;208:333-5.
36. Boesen F, Andersen EB, Jensen EK, Ladefoged SD. Cardiac conduction disturbances during carbamazepine therapy. Acta Neurol Scand. 1983;68:49-52.
37. Kenneback G, Bergfeldt L, Vallin H, et al. Electrophysiologic effects and clinical hazards of carbamazepine treatment for neurologic disorders in patients with abnormalities of thecardiac conduction system. Am Heart J. 1991;121:1421-9.
38. Weig SG, Pollack P. Carbamazepine-induced heart block in a child with tuberous sclerosis and cardiac rhabdomyoma - implications for evaluation and follow-up. Ann Neurol. 1993;34:617-9.
39. Steckler TL. Lithium- and carbamazepine-associated sinus node dysfunction: nine-year experience in a psychiatric hospital. J Clin Psychopharmacol. 1994;14:336-9.
40. Verma SP, Yunis N, Lekos A, Crausman RS. Carbamazepine-induced systemic lupus erythematosus presenting as cardiac tamponade. Chest. 2000;117:597-8.
41. Hennessy MJ, Tighe MG, Binnie CD, Nashef L. Sudden withdrawal of carbamazepine increases cardiac sympathetic activity in sleep. Neurology. 2001;57:1650-4.
42. Joyce RP, Gunderson CH. Carbamazepine-induced orofacial dyskinesia. Neurology. 1980;30:1333-4.
43. Ambrosetto G, Riva R, Baruzzi A. Hyperammonemia in asterixis induced by carbamazepine: two case reports. Acta Neurol Scand. 1984;69:186-9.
44. Stuppaeck CH, Whitworth AB, Fleischhacker WW. Abuse potential of carbamazepine. J Nerv Ment Dis. 1993;181:519-20.
45. Wildin JD, Pleuvry BJ, Mawer GE. Impairment of psychomotor function at modest plasma concentrations of carbamazepine after administration of the liquid suspension to naive subjects. Br J Clin Pharmacol. 1993;35:14-9.
46. Neufeld MY. Exacerbation of focal seizures due to carbamazepine treatment in an adult patient. Clin Neuropharmacol. 1993;16:359-61.
47. Malow BA, Blaxton TA, Stertz B, Theodore WH. Carbamazepine withdrawal - effects of taper rate on seizure frequency. Neurology. 1993;43:2280-4.
48. Pulliainen V, Jokelainen M. Effects of phenytoin and carbamazepine on cognitive functions in newly diagnosed epileptic patients. Acta Neurol Scand. 1994;89:81-6.
49. So EL, Ruggles KH, Cascino GD, Ahmann PA, Weatherford KW. Seizure exacerbation and status epilepticus related to carbamazepine-10,11-epoxide. Ann Neurol. 1994;35:743-6.
50. Smith KR, Goulding PM, Wilderman D, Goldfader PR, Holtermanhommes P, Wei FF. Neurobehavioral effects of phenytoin and carbamazepine in patients recovering from brain trauma: a comparative study. Arch Neurol. 1994;51:653-60.
51. Roberts DL, Marks R. Skin reactions to carbamazepine. Arch Dermatol. 1981;117:273-5.
52. Bateman DE. Carbamazepine induced systemic lupus erythematosus: case report. Br Med J. 1985;291:632-3.
53. De Giorgio CM, Rabinowicz AL, Olivas RD. Carbamazepine-induced antinuclear antibodies and systemic lupus erythematosus-like syndrome. Epilepsia. 1991;32:128-9.
54. Meisel S, North CQ. Carbamazepine-associated erythema multiforme with extreme eosinophilia. Clin Pharm. 1984;3:15-9.
55. Merino N, Duran JA, Jimenez MC, Ravella R. Multisystem hypersensitivity reaction to carbamazepine. Ann Pharmacother. 1994;28:402-3.
56. Takahashi N, Aizawa H, Takata S, Matsumoto K, Koto H, Inoue H, Hara N. Acute interstitial pneumonitis induced by carbamazepine. Eur Respir J. 1993;6:1409-11.
57. Parha S, Garoufi A, Yiallouros P, Theodoridis C, Karpathios T. Carbamazepine hypersensitivity and rickettsiosis mimicking kawasaki disease. Eur J Pediatr. 1993;152:1040-1.
58. Richens A, Davidson DLW, Cartlidge NEF, Easter DJ. A multicentre comparative trial of sodium valproate and carbamazepine in adult onset epilepsy. J Neurol Neurosurg Psychiatry. 1994;57:682-7.
59. Roujeau JC, Kelly JP, Naldi L, et al. Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. N Engl J Med. 1995;333:1600-7.
60. Suzuki Y, Fukuda M, Tohyama M, Ishikawa M, Yasukawa M, Ishii E. Carbamazepine-induced drug-induced hypersensitivity syndrome in a 14-year-old Japanese boy. Epilepsia. 2008;49:2118-21.
61. Fsadni C, Fsadni P, Piscopo T, Mallia Azzopardi C. Carbamazepine-induced drug reaction with eosinophilia and systemic symptoms syndrome in a 35-year-old man with epilepsy. Clin Neuropharmacol. 2008;31:295-8.
62. Levy M, Goodman MW, Van Dyne BJ, Sumner HW. Granulomatous hepatitis secondary to carbamazepine. Ann Intern Med. 1981;95:64-5.
63. Larrey D, Hadengue A, Pessayre D, et al. Carbamazepine-induced acute cholangitis. Dig Dis Sci. 1987;32:554-7.
64. Horowitz S, Patwardhan R, Marcus E. Hepatotoxic reactions associated with carbamazepine therapy. Epilepsia. 1988;29:149-54.
65. Hopen G, Nesthus I, Laerum OD. Fatal carbamazepine-associated hepatitis. Acta Med Scand. 1981;210:333-5.
66. Sheridan WP, King RW, Gerstman M. Fever as an adverse reaction to carbamazepine. Aust N Z J Med. 1982;12:520-2.
67. Swinburn BA, Croxson MS, Miller MV, Crawford KB. Carbamazepine induced granulomatous hepatitis. N Z Med J. 1986;Mar:167.
68. Soffer EE, Taylor RJ, Bertram PD, et al. Carbamazepine-induced liver injury. South Med J. 1983;76:681-3.
69. Laspina I, Secchi P, Grampa G, Uccellini D, Porazzi D. Acute cholangitis induced by carbamazepine. Epilepsia. 1994;35:1029-31.
70. Hogg RJ, Sawyer M, Hecox K, Eigenbrodt E. Carbamazepine-induced acute tubulointerstitial nephritis. J Pediatr. 1981;98:830-2.
71. Hegbrant J, Kurkus J, Oqvist B. Carbamazepine-related acute renal failure. Neurology. 1993;43:446-7.
72. Jubert P, Almirall J, Casanovas A, Garcia M. Carbamazepine-induced acute renal failure. Nephron. 1994;66:121.
73. King GG, Barnes DJ, Hayes MJ. Carbamazepine-induced pneumonitis. Med J Aust. 1994;160:126-7.
74. Brenner S, Wolf R, Landau M, Politi Y. Psoriasiform eruption induced by anticonvulsants. Isr J Med Sci. 1994;30:283-6.
75. Mecarelli O, Rinalduzzi S, Accornero N. Changes in color vision after a single dose of vigabatrin or carbamazepine in healthy volunteers. Clin Neuropharmacol. 2001;24:23-6.
76. DiLernia V, Viglio A, Cattania M, Paulli M. Carbamazepine-induced, CD30(+), primary, cutaneous, anaplastic large-cell lymphoma. Arch Dermatol. 2001;137:675-6.
77. Hayman G, Bansal A. Antibody deficiency associated with carbamazepine. BMJ. 2002;325:1213.
78. Sanacora G, Kendell SF, Fenton L, Coric V, Krystal JH. Riluzole augmentation for treatment-resistant depression. Am J Psychiatry. 2004;161:2132.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.