Aspirin / oxycodone Side Effects
Medically reviewed by Drugs.com. Last updated on Oct 12, 2023.
Applies to aspirin / oxycodone: oral tablet.
Warning
- This drug is a strong pain drug that can put you at risk for addiction, abuse, and misuse. Misuse or abuse of this drug can lead to overdose and death. Talk with your doctor.
- You will be watched closely to make sure you do not misuse, abuse, or become addicted to this drug.
- This drug may cause very bad and sometimes deadly breathing problems. Call your doctor right away if you have slow, shallow, or trouble breathing.
- The chance of very bad and sometimes deadly breathing problems may be greater when you first start this drug or anytime your dose is raised.
- Even one dose of this drug may be deadly if it is taken by someone else or by accident, especially in children. If this drug is taken by someone else or by accident, get medical help right away.
- Keep all drugs in a safe place. Keep all drugs out of the reach of children and pets.
- Using this drug for a long time during pregnancy may lead to withdrawal in the newborn baby. This can be life-threatening. Talk with the doctor.
- This drug has an opioid drug in it. Severe side effects have happened when opioid drugs were used with benzodiazepines or other drugs that may make you drowsy or slow your actions. This includes slow or troubled breathing and death. Benzodiazepines include drugs like alprazolam, diazepam, and lorazepam. Benzodiazepines may be used to treat many health problems like anxiety, trouble sleeping, or seizures. If you have questions, talk with your doctor.
- Many drugs interact with this drug and can raise the chance of side effects like deadly breathing problems. Talk with your doctor and pharmacist to make sure it is safe to use this drug with all of your drugs.
- Do not take with alcohol or products that have alcohol. Unsafe and sometimes deadly effects may happen.
- Get medical help right away if you feel very sleepy, very dizzy, or if you pass out. Caregivers or others need to get medical help right away if the patient does not respond, does not answer or react like normal, or will not wake up.
Serious side effects of Aspirin / oxycodone
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
- Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
- Signs of high potassium levels like a heartbeat that does not feel normal; feeling confused; feeling weak, lightheaded, or dizzy; feeling like passing out; numbness or tingling; or shortness of breath.
- Weakness on 1 side of the body, trouble speaking or thinking, change in balance, drooping on one side of the face, or blurred eyesight.
- Very bad dizziness or passing out.
- Severe constipation or stomach pain. These may be signs of a severe bowel problem.
- Noisy breathing.
- Ringing in ears.
- Hearing loss.
- Dark urine or yellow skin or eyes.
- Not able to pass urine or change in how much urine is passed.
- Mood changes.
- Seizures.
- Chest pain or pressure or a fast heartbeat.
- Feeling confused.
- A severe and sometimes deadly problem called serotonin syndrome may happen if you take this drug with certain other drugs. Call your doctor right away if you have agitation; change in balance; confusion; hallucinations; fever; fast or abnormal heartbeat; flushing; muscle twitching or stiffness; seizures; shivering or shaking; sweating a lot; severe diarrhea, upset stomach, or throwing up; or severe headache.
Other side effects of Aspirin / oxycodone
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
- Constipation.
- Feeling dizzy, sleepy, tired, or weak.
- Upset stomach or throwing up.
- Headache.
- Stomach pain.
These are not all of the side effects that may occur. If you have questions about side effects, call your doctor. Call your doctor for medical advice about side effects.
You may report side effects to the FDA at 1-800-332-1088. You may also report side effects at https://www.fda.gov/medwatch.
For Healthcare Professionals
Applies to aspirin / oxycodone: oral tablet.
General
The most commonly reported adverse events have included lightheadedness, dizziness, drowsiness, sedation, nausea, and vomiting.[Ref]
Gastrointestinal
Oxycodone-Aspirin:
Frequency not reported: Nausea, vomiting, constipation
Postmarketing reports: Hemorrhagic gastric/duodenal ulcer, gastric/peptic ulcer, dyspepsia, abdominal pain, diarrhea, eructation, dry mouth, gastrointestinal bleeding, intestinal perforation, pancreatitis, intestinal obstruction, ileus, thirst, aspiration
Aspirin:
Frequency not reported: Anorexia[Ref]
Nervous system
Frequency not reported: Lightheadedness, dizziness, drowsiness, sedation
Postmarketing reports: Stupor, paresthesia, cerebral edema, coma, subdural or intracranial hemorrhage, seizures
Opioids:
Postmarketing reports: Serotonin syndrome[Ref]
Renal
Postmarketing reports: Renal insufficiency and failure[Ref]
Hematologic
Oxycodone-aspirin:
Postmarketing reports: Unspecified hemorrhage, purpura, reticulocytosis, prolongation of prothrombin time, disseminated intravascular coagulation, ecchymosis, thrombocytopenia
Aspirin:
Frequency not reported: Leukopenia, thrombocytopenia, purpura, decreased iron concentration, shortened erythrocyte survival time[Ref]
Hypersensitivity
Postmarketing reports: Anaphylaxis, allergic reaction, angioedema[Ref]
Cardiovascular
Frequency not reported: Hypotension
Postmarketing reports: Tachycardia, dysrhythmias, orthostatic hypotension, bradycardia, palpitations[Ref]
Metabolic
Postmarketing reports: Hypoglycemia, hyperglycemia, acidosis, alkalosis, dehydration, hyperkalemia[Ref]
Other
Postmarketing reports: Malaise, asthenia, hypothermia, accidental overdose, non-accidental overdose, hearing loss, tinnitus[Ref]
Hepatic
Oxycodone-aspirin:
Postmarketing reports: Transient elevations of hepatic enzymes, hepatitis, Reye syndrome
Aspirin:
Frequency not reported: Reversible hepatotoxicity[Ref]
Psychiatric
Frequency not reported: Euphoria, dysphoria
Postmarketing reports: Agitation, confusion, anxiety, mental impairment, drug dependence, drug abuse, depression, nervousness, hallucination[Ref]
Dermatologic
Frequency not reported: Pruritus
Postmarketing reports: Urticaria, rash, flushing, increased sweating[Ref]
Musculoskeletal
Postmarketing reports: Rhabdomyolysis
Ocular
Postmarketing reports: Miosis, visual disturbances, red eye
Genitourinary
Frequency not reported: Urinary retention, interstitial nephritis, proteinuria
Respiratory
Frequency not reported: Apnea, respiratory arrest, respiratory depression
Postmarketing reports: Bronchospasm, dyspnea, hyperpnea, pulmonary edema, tachypnea, hypoventilation, laryngeal edema
Endocrine
Opioids:
Postmarketing reports: Adrenal insufficiency, androgen deficiency
Adrenal insufficiency and androgen deficiency have been reported with opioid use, most often with chronic use.
More about aspirin / oxycodone
- Check interactions
- Compare alternatives
- Reviews (6)
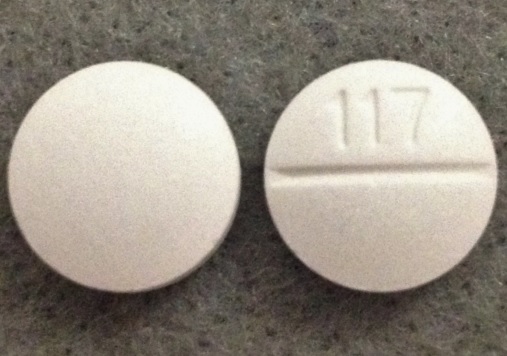
- Drug images
- Dosage information
- During pregnancy
- Drug class: narcotic analgesic combinations
Patient resources
Other brands
Professional resources
Related treatment guides
References
1. Leow KP, Smith MT, Watt JA, Williams BE, Cramond T. Comparative oxycodone pharmacokinetics in humans after intravenous, oral, and rectal administration. Ther Drug Monit. 1992;14:479-84.
2. Product Information. Percodan (aspirin-oxycodone). Endo Laboratories LLC. 2016;SUPPL-49.
3. Bergmann JF, Chassany O, Geneve J, Abiteboul M, Caulin C, Segrestaa JM. Endoscopic evaluation of the effect of ketoprofen, ibuprofen and aspirin on the gastroduodenal mucosa. Eur J Clin Pharmacol. 1992;42:685-8.
4. Leow KP, Smith MT, Williams B, Cramond T. Single-dose and steady-state pharmacokinetics and pharmacodynamics of oxycodone in patients with cancer. Clin Pharmacol Ther. 1992;52:487-95.
5. Glare P, Walsh D. Dose-ranging study of oxycodone for advanced cancer pain (meeting abstract). Proc Annu Meet Am Soc Clin Oncol. 1991;10:a1201.
6. Mehta S, Dasarathy S, Tandon RK, Mathur M, Malaviya AN. A prospective randomized study of the injurious effects of aspirin and naproxen on the gastroduodenal mucosa in patients with rheumatoid arthritis. Am J Gastroenterol. 1992;87:996-1000.
7. Naschitz JE, Yeshurun D, Odeh M, Bassan H, Rosner I, Stermer E, Levy N. Overt gastrointestinal bleeding in the course of chronic low-dose aspirin administration for secondary prevention of arterial occlusive disease. Am J Gastroenterol. 1990;85:408-11.
8. Sabesin SM, Boyce HW Jr, King CE, Mann JA, Ruoff G, Wall E. Comparative evaluation of gastrointestinal intolerance produced by plain and tri-buffered aspirin tablets. Am J Gastroenterol. 1988;83:1220-5.
9. Graham DY, Smith JL. Aspirin and the stomach. Ann Intern Med. 1986;104:390-8.
10. Levy M, Miller DR, Kaufman DW, Siskind V, Schwingl P, Rosenberg L, Strom B, Shapiro S. Major upper gastrointestinal tract bleeding. Relation to the use of aspirin and other nonnarcotic analgesics. Arch Intern Med. 1988;148:281-5.
11. Prichard PJ, Kitchingman GK, Walt RP, Daneshmend TK, Hawkey CJ. Human gastric mucosal bleeding induced by low dose aspirin, but not warfarin. BMJ. 1989;298:493-6.
12. Roderick PJ, Wilkes HC, Meade TW. The gastrointestinal toxicity of aspirin: an overview of randomised controlled trials. Br J Clin Pharmacol. 1993;35:219-26.
13. Glare PA, Walsh TD. Dose-ranging study of oxycodone for chronic pain in advanced cancer. J Clin Oncol. 1993;11:973-8.
14. Sunshine A, Olson NZ, Zighelboim I, Decastro A. Ketoprofen, acetaminophen plus oxycodone, and acetaminophen in the relief of postoperative pain. Clin Pharmacol Ther. 1993;54:546-55.
15. Wilcox CM, Shalek KA, Cotsonis G. Striking prevalence of over-the-counter nonsteroidal anti- inflammatory drug use in patients with upper gastrointestinal hemorrhage. Arch Intern Med. 1994;154:42-6.
16. Silagy CA, McNeil JJ, Donnan GA, Tonkin AM, Worsam B, Campion K. Adverse effects of low-dose aspirin in a healthy elderly population. Clin Pharmacol Ther. 1993;54:84-9.
17. Thirlby RC. More problems with aspirin: it may cause appendicitis. Gastroenterology. 1993;104:1571-3.
18. D'Haens G, Breysem Y, Rutgeerts P, van Besien B, Geboes K, Ponette E, Vantrappen G. Proctitis and rectal stenosis induced by nonsteroidal antiinflammatory suppositories. J Clin Gastroenterol. 1993;17:207-12.
19. Halla JT, Hardin JG. Salicylate ototoxicity in patients with rheumatoid arthritis: a controlled study. Ann Rheum Dis. 1988;47:134-7.
20. Boettcher FA, Salvi RJ. Salicylate ototoxicity: review and synthesis. Am J Otolaryngol. 1991;12:33-47.
21. Carlyon RP, Butt M. Effects of aspirin on human auditory filters. Hear Res. 1993;66:233-44.
22. Kimberly RP, Plotz PH. Aspirin-induced depression of renal function. N Engl J Med. 1977;296:418-24.
23. Riegger GA, Kahles HW, Elsner D, Kromer EP, Kochsiek K. Effects of acetylsalicylic acid on renal function in patients with chronic heart failure. Am J Med. 1991;90:571-5.
24. Carmichael J, Shankel SW. Effects of nonsteroidal anti-inflammatory drugs on prostaglandins and renal function. Am J Med. 1985;78:992-1000.
25. Wen SF, Parthasarathy R, Iliopoulos O, Oberley TD. Acute renal failure following binge drinking and nonsteroidal antiinflammatory drugs. Am J Kidney Dis. 1992;20:281-5.
26. Maher JF. Analgesic nephropathy. Observations, interpretations, and perspective on the low incidence in America. Am J Med. 1984;76:345-8.
27. Muther RS, Potter DM, Bennett WM. Aspirin-induced depression of glomerular filtration rate in normal humans: role of sodium balance. Ann Intern Med. 1981;94:317-21.
28. Sutor AH. Thrombocyturia after aspirin. N Engl J Med. 1973;288:794-5.
29. Moroz LA. Increased blood fibrinolytic activity after aspirin ingestion. N Engl J Med. 1977;296:525-9.
30. Barrow MV, Quick DT, Cunningham RW. Salicylate hypoprothrombinemia in rheumatoid arthritis with liver disease. Report of two cases. Arch Intern Med. 1967;120:620-4.
31. Wijnja L, Snijder JA, Nieweg HO. Acetylsalicylic acid as a cause of pancytopenia from bone-marrow damage. Lancet. 1966;2:768-70.
32. Williams JO, Mengel CE, Sullivan LW, Haq AS. Megaloblastic anemia associated with chronic ingestion of an analgesic. N Engl J Med. 1969;280:312-3.
33. Eldar M, Aderka D, Shoenfeld Y, Livni E, Pinkhas J. Aspirin-induced aplastic anaemia. S Afr Med J. 1979;55:318.
34. Fausa O. Salicylate-induced hypoprothrombinemia: a report of four cases. Acta Med Scand. 1970;188:403-8.
35. Lee TH. Mechanism of bronchospasm in aspirin-sensitive asthma. Am Rev Respir Dis. 1993;148:1442-3.
36. Israel E, Fischer AR, Rosenberg MA, Lilly CM, Callery JC, Shapiro J, Cohn J, Rubin P, Drazen JM. The pivotal role of 5-lipoxygenase products in the reaction of aspirin-sensitive asthmatics to aspirin. Am Rev Respir Dis. 1993;148:1447-51.
37. Kowalski ML, Sliwinska-Kowalska M, Igarashi Y, White MV, Wojciechowska B, Brayton P, Kaulbach H, Rozniecki J, Kaliner MA. Nasal secretions in response to acetylsalicylic acid. J Allergy Clin Immunol. 1993;91:580-98.
38. Katz Y, Goldberg N, Kivity S. Localized periorbital edema induced by aspirin. Allergy. 1993;48:366-9.
39. Al-Abbasi AH. Salicylate-induced variant angina. Am Heart J. 1983;106:1450.
40. Mukerji V, Alpert MA, Flaker GC, Beach CL, Weber RD. Cardiac conduction abnormalities and atrial arrhythmias associated with salicylate toxicity. Pharmacotherapy. 1986;6:41-3.
41. Berg KJ. Acute acetylsalicylic acid poisoning: treatment with forced alkaline diuresis and diuretics. Eur J Clin Pharmacol. 1977;12:111-6.
42. David DS, Steere AC Jr, Pi-Sunyer XF, Sakai S, Clark SB. Aspirin-induced hypoglycaemia in a patient on haemodialysis. Lancet. 1971;2:1092-3.
43. Gardos G. Dyskinesia after discountinuation of compound analgesic containing oxycodone . Lancet. 1977;1:759-60.
44. Fishbain DA, Goldberg M, Rosomoff RS, Rosomoff H. Atypical withdrawal syndrome (organic delusional syndrome) secondary to oxycodone detoxification . J Clin Psychopharmacol. 1988;8:441-2.
45. Peters LJ, Wiener GJ, Gilliam J, Van Noord G, Geisinger KR, Roach ES. Reye's syndrome in adults. A case report and review of the literature. Arch Intern Med. 1986;146:2401-3.
46. Epidemiology Office, Divisiion of Viral and Rickettsial Diseasses, Center for Infectious Diseases, Centers for Disease Control. Leads from the MMWR. Reye syndrome surveillance--United States, 1987 and 1988. JAMA. 1989;261:3520,.
47. Seaman WE, Ishak KG, Plotz PH. Aspirin-induced hepatotoxicity in patients with systemic lupus erythematosus. Ann Intern Med. 1974;80:1-8.
48. Wolfe JD, Metzger AL, Goldstein RC. Aspirin hepatitis. Ann Intern Med. 1974;80:74-6.
49. Sbarbaro JA, Bennett RM. Aspirin hepatotoxicity and disseminated intravascular coagulation. Ann Intern Med. 1977;86:183-5.
50. Pearson RE, Salter FJ. Drug interaction? Orphenadrine with propoxyphene. N Engl J Med. 1970;282:1215.
51. Bharija SC, Belhaj MS. Acetylsalicylic acid may induce a lichenoid eruption. Dermatologica. 1988;177:19.
52. Analysis of Reports to the Spontaneous Reporting System of the Gruppo Italiano Studi Epidemiiologici in Dermatologia. Cutaneous reactions to analgesic-antipyretics and nonsteroidal anti- inflammatory drugs. Dermatology. 1993;186:164-9.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.