Valproic Acid and Derivatives
Medically reviewed by Drugs.com. Last updated on Apr 28, 2023.
Pronunciation
(val PROE ik AS id & dah RIV ah tives)
Index Terms
- 2-Propylpentanoic Acid
- 2-Propylvaleric Acid
- Dipropylacetic Acid
- Divalproex Sodium
- DPA
- Valproate Semisodium
- Valproate Sodium
- Valproic Acid
- Valproic Acid Derivative
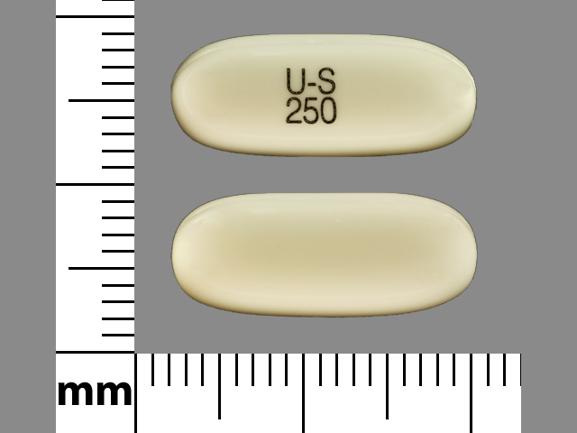
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral, Immediate Release, as valproic acid:
Depakene: 250 mg [DSC]
Generic: 250 mg
Capsule Delayed Release Sprinkle, Oral, as divalproex sodium:
Depakote Sprinkles: 125 mg [contains brilliant blue fcf (fd&c blue #1)]
Generic: 125 mg
Solution, Oral, Immediate Release, as valproate sodium:
Depakene: 250 mg/5 mL (480 mL [DSC])
Generic: 250 mg/5 mL (5 mL, 10 mL, 473 mL)
Solution, Intravenous, as valproate sodium:
Depacon: 100 mg/mL (5 mL [DSC]) [contains edetate disodium]
Solution, Intravenous, as valproate sodium [preservative free]:
Generic: 100 mg/mL (5 mL)
Tablet Delayed Release, Oral, as divalproex sodium:
Depakote: 125 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40]
Depakote: 250 mg [contains fd&c yellow #6 (sunset yellow)]
Depakote: 500 mg [contains fd&c blue #2 (indigotine)]
Generic: 125 mg, 250 mg, 500 mg
Tablet Extended Release 24 Hour, Oral, as divalproex sodium:
Depakote ER: 250 mg, 500 mg
Generic: 250 mg, 500 mg
Related/similar drugs
Qulipta, Aimovig, Emgality, Ubrelvy, Vraylar, gabapentin, acetaminophen
Brand Names: U.S.
- Depacon [DSC]
- Depakene [DSC]
- Depakote
- Depakote ER
- Depakote Sprinkles
Pharmacologic Category
- Anticonvulsant, Miscellaneous
- Antimanic Agent
- Histone Deacetylase Inhibitor
Pharmacology
Causes increased availability of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter, to brain neurons or may enhance the action of GABA or mimic its action at postsynaptic receptor sites. Also blocks voltage-dependent sodium channels, which results in suppression of high-frequency repetitive neuronal firing (Bourin 2009). Divalproex sodium is a compound of sodium valproate and valproic acid; divalproex dissociates to valproate in the GI tract.
Distribution
Distributes into CSF at concentrations similar to unbound concentration in plasma (ie, ∼10% of total plasma concentration)
Vd: Total valproate: 11 L/1.73 m2; Free valproate 92 L/1.73 m2
Metabolism
Extensively hepatic via glucuronide conjugation (30% to 50% of administered dose) and 40% via mitochondrial beta-oxidation; other oxidative metabolic pathways occur to a lesser extent.
Excretion
Urine (30% to 50% as glucuronide conjugate, <3% as unchanged drug); faster clearance in children who receive other antiepileptic drugs and those who are younger; age and polytherapy explain 80% of interpatient variability in total clearance; children >10 years of age have pharmacokinetic parameters similar to adults
Time to Peak
Oral:
Divalproex sodium:
Delayed release: tablet and sprinkle capsules: ~4 hours
Extended release: 4 to 17 hours
Immediate release enteric-coated tablet [Canadian product]: 4 hours
Valproic acid delayed release capsule: 2 hours
Rectal (off-label route): 1 to 3 hours (Graves 1987)
Half-Life Elimination
Increased in neonates, elderly, and patients with liver impairment
Newborns (exposed to VPA in utero): 30 to 60 hours
Neonates first week of life: 40 to 45 hours
Neonates <10 days: 10 to 67 hours
Infants and Children >2 months: 7 to 13 hours
Children and Adolescents 2 to 14 years: 9 hours (range: 3.5 to 20 hours) (Cloyd 1993)
Adults: 9 to 16 hours
Protein Binding
Concentration dependent: 80% to 90%; free fraction: ~10% at 40 mcg/mL and ~18.5% at 130 mcg/mL; protein binding decreased in neonates, the elderly and patients with hepatic or renal impairment
Special Populations: Renal Function Impairment
A 27% reduction in clearance of unbound valproate is seen in patients with CrCl <10 mL/minute. Hemodialysis reduces valproate concentrations by 20%. Therefore, no dosage adjustment appears to be necessary in patients with renal failure. Protein binding is reduced. Monitoring of free valproate concentrations may be of clinical value; total valproate concentrations may be misleading.
Special Populations: Hepatic Function Impairment
Clearance is decreased with liver impairment. Hepatic disease is also associated with decreased albumin concentrations and 2- to 2.6-fold increase in the unbound fraction. Free concentrations of valproate may be elevated while total concentrations appear normal.
Use: Labeled Indications
Bipolar disorder: Treatment of manic episodes (delayed release) or acute manic or mixed episodes with or without psychotic features (extended release) associated with bipolar disorder, as monotherapy or in combination with atypical antipsychotics (BAP [Goodwin 2016])
Focal (partial) onset and generalized onset seizures: Monotherapy and adjunctive therapy in the treatment of patients with focal onset seizures with impairment of consciousness or awareness (complex partial) and generalized onset nonmotor seizures (absence), and as adjunctive therapy for multiple seizure types. May be used off-label as monotherapy for other seizure types.
Migraine prophylaxis (excluding IV formulation): Prophylaxis of migraine headaches
Limitation of use: Do not administer to pregnant women, women who plan to become pregnant, or women of childbearing potential for the treatment of epilepsy or bipolar disorder unless essential for the management of her condition.
Off Label Uses
Bipolar major depression (alternative agent)
Data from a limited number of patients studied suggest that valproate may be beneficial as monotherapy for the treatment of depressive episodes in patients with bipolar disorder [Davis 2005], [Ghaemi 2007], [Muzina 2011].
Based on the Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) guidelines for the management of patients with bipolar disorder, valproate is recommended as monotherapy or as an adjunct to antidepressants in patients who have not responded to first-line options [CANMAT/ISBD [Yatham 2018]].
Maintenance treatment of bipolar disorder
Data from a limited number of clinical trials suggest that valproate may delay future mood episodes following a manic episode in bipolar disorder [Cipriani 2013].
Based on the Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) guidelines for the management of patients with bipolar disorder and the World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders, medications that are effective in acute mania are recommended for continuation during maintenance treatment, and valproate is recommended for maintenance treatment of bipolar disorder based on limited positive evidence [CANMAT/ISBD [Yatham 2018]], [WFSBP [Grunze 2013]]. Based on the WFSBP guidelines for the acute and long-term treatment of mixed states in bipolar disorder, valproate is recommended for maintenance treatment to prevent a mixed episode following a depressed or manic episode based on limited positive evidence [WFSBP [Grunze 2018]].
Status epilepticus
Data from multiple studies, including randomized controlled trials, support the use of valproate sodium for the treatment of urgent or refractory status epilepticus [Agarwal 2007], [Alvarez 2011], [Gilad 2008], [Limdi 2005], [Misra 2006], [Olsen 2007], [Peters 2005], [Sinha 2000], [Tripathi 2010]. In a systematic review of clinical trials in status epilepticus, valproate sodium was determined to be a safe therapeutic option in patients with established status epilepticus who previously failed conventional first-line treatment with benzodiazepines [Trinka 2014].
Based on the Neurocritical Care Society guidelines for the evaluation and management of status epilepticus and the American Epilepsy Society Guidelines for the treatment of convulsive status epilepticus in children and adults, the use of intravenous valproate sodium is an effective and recommended treatment option for urgent control of status epilepticus in adults; however, benzodiazepines continue to be the agents of choice for initial therapy.
Contraindications
Hypersensitivity to valproic acid, divalproex, derivatives, or any component of the formulation; hepatic disease or significant impairment; urea cycle disorders; prevention of migraine in pregnant women and women of childbearing potential who are not using effective contraception; known mitochondrial disorders caused by mutations in mitochondrial DNA polymerase gamma (POLG; eg, Alpers-Huttenlocher syndrome [AHS]) or children <2 years of age suspected of having a POLG-related disorder
Canadian labeling: Additional contraindications (not in US labeling): Treatment of epilepsy in pregnant women, unless no suitable alternative; treatment of epilepsy in women of childbearing potential, unless requirements of Pregnancy Prevention Program fulfilled (see Canadian labeling for more information); known porphyria
Epival: Additional contraindication: Treatment of bipolar disorder in pregnant women, unless no suitable alternative; treatment of bipolar disorder in women of childbearing potential, unless requirements of Pregnancy Prevention Program fulfilled (see Canadian labeling for more information)
Dosing: Adult
Note: The dosing recommendations in this monograph are expressed as the total daily dose (ie, per 24 hours) unless stated otherwise. The total daily oral dose is given in 1 to 4 divided doses per day depending on the type of preparation. Available preparations include: Oral immediate release (usually dosed 3 to 4 times daily [Koch-Weser 1980]), delayed release (DR) (usually dosed 2 to 3 times daily) and extended release (ER) (commonly dosed once daily; may also be dosed twice daily) formulations and an IV injection (Bialer 2007). The ER oral formulation is not available in Canada. Available formulations of valproate (active moiety) include valproic acid, valproate sodium, and divalproex sodium (also known as valproate semisodium) salts. All doses in this monograph are expressed as the equivalent amounts of valproic acid.
Bipolar disorder:
Acute manic or mixed episodes (in combination with or as an alternative to an antipsychotic) (BAP [Goodwin 2016]):
Fixed dose: Oral: Initial: 500 to 750 mg/day (BAP [Goodwin 2016]; Tohen 2008); increase by 250 to 500 mg every 1 to 3 days to reach desired clinical effect and therapeutic serum concentration (BAP [Goodwin 2016]; Stovall 2018); therapeutic serum levels generally occur with daily doses of 1.5 to 2.5 g (Stovall 2018). Maximum recommended dosage: 60 mg/kg/day (manufacturer's labeling).
Weight-based loading dose for rapid symptom control: Oral: Initial: 20 to 30 mg/kg/day. After 2 to 3 days, adjust dose upward or downward to reach desired clinical effect and therapeutic serum concentration (BAP [Goodwin 2016]; Bowden 2006; Bowden 2010; Hirschfeld 1999); therapeutic serum levels generally occur with daily doses of 1.5 to 2.5 g. To avoid intolerable adverse effects, some experts limit the initial rapid loading dose to 20 mg/kg/day (up to 2 g/day if body weight exceeds 100 kg) and then adjust based on response and serum concentration (Stovall 2018). Maximum recommended dosage: 60 mg/kg/day (manufacturer's labeling).
Bipolar major depression (alternative agent) (mono- or adjunctive therapy) (off-label use): Based on limited data: Oral: Initial: 500 to 750 mg/day; increase by 250 to 500 mg every 1 to 3 days to reach desired clinical effect and therapeutic serum concentration; therapeutic serum levels generally occur with daily doses of 1.5 to 2.5 g (CANMAT/ISBD [Yatham 2018]; Davis 2005; Ghaemi 2007; Muzina 2011; Shelton 2019).
Maintenance treatment of bipolar disorder (off-label): Oral: Continue dose and combination regimen that was used to achieve control of the acute episode (Gyulai 2003; McElroy 2008).
Focal (partial) onset seizures and generalized onset seizures (FDA-approved for monotherapy or adjunctive therapy of complex partial and absence seizures, and as adjunctive therapy for multiple seizure types; may be used off-label as monotherapy for other seizure types):
Oral: Initial monotherapy or adjunctive therapy: 10 to 15 mg/kg/day for complex partial seizures or 15 mg/kg/day for absence seizures; increase by 5 to 10 mg/kg/day at weekly intervals until optimal clinical response and/or therapeutic levels are achieved; maximum recommended dose: 60 mg/kg/day (manufacturer's labeling). Some experts suggest checking serum level ~1 to 2 weeks after initial dose to help guide dose adjustment (Schachter 2018).
Conversion to monotherapy from valproate adjunctive therapy: Initial oral dosage as above. Dosage reduction of the concomitant antiseizure drug may begin when valproate therapy is initiated or 1 to 2 weeks following valproate initiation; taper the concomitant antiseizure drug over 8 weeks (ie, by ~25% every 2 weeks).
IV (for non-status epilepticus): Total daily IV dose should be equivalent to the total daily oral valproate dose (expressed as valproic acid) and divided every 6 hours. Administer each dose as a 60-minute infusion (rate ≤20 mg/minute). Note: In non-status epilepticus, IV formulation should be used only for those who temporarily cannot use oral formulations; switch to oral formulation as soon as appropriate.
Migraine prophylaxis: Oral: Initial: 500 mg once daily (ER) or in 2 divided doses (DR or ER); increase dose gradually based on response and tolerability in increments of 250 mg/day at intervals >3 days up to 1 g/day. Based on clinical experience, some patients require doses up to 1.5 g/day for sufficient response; however, adverse effects are increased (Bajwa 2018; Klapper 1997; Linde 2013; Pringsheim 2010).
Status epilepticus (off-label use): Note: Given in combination with an IV benzodiazepine: IV: Loading dose: 20 to 40 mg/kg administered at a rate up to 10 mg/kg/minute (maximum dose: 3 g) (AES [Glauser 2016]; Limdi 2007; NCS [Brophy 2012]). In non-convulsive status epilepticus, some experts recommend a maximal infusion rate of 5 mg/kg/minute (Gaspard 2018).
Discontinuation of therapy: In patients receiving valproic acid chronically, unless safety concerns require a more rapid withdrawal, valproic acid should be withdrawn gradually over 2 to 6 months to minimize the potential of increased seizure frequency (in patients with epilepsy) or other withdrawal symptoms (Medical Research Council Antiepileptic Drug Withdrawal Study Group 1991; Schachter 2019). In patients discontinuing therapy for treatment of bipolar disorder, close monitoring for several weeks to months for reemergence of mania/hypomania is recommended (Post 2019).
Dosing conversions: Note: The ER formulation is not available in Canada:
Conversion from immediate release to DR or ER: When converting to DR, use the same total daily dose as the immediate release and divide into 2 to 3 daily doses. When converting from immediate release to ER, increase the total daily dose of ER by 8% to 20% and dose once daily (most common) or twice daily (Bialer 2007).
Conversion from DR to ER: For patients on a stable dose of DR, increase the total daily dose of ER by 8% to 20% to maintain similar serum concentrations, and dose once daily (most common) or twice daily (Bialer 2007).
Conversion to IV valproate preparations: To continue therapy IV in patients temporarily unable to receive oral therapy, total daily IV dose should be equivalent to the total daily oral dose (expressed as valproic acid) and divided every 6 hours. Trough levels may fall below the equivalent oral regimen when administered less frequently than every 6 hours; in these cases, closely monitor trough plasma concentrations.
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Dosing: Geriatric
Note: The dosing recommendations in this monograph are expressed as the total daily dose (ie, per 24 hours) unless stated otherwise. The total daily oral dose is given in 1 to 4 divided doses per day depending on the type of preparation. Available preparations include: Oral immediate release (usually dosed 3 to 4 times daily [Koch-Weser 1980]), delayed release (DR) (usually dosed 2 to 3 times daily) and extended release (ER) (commonly dosed once daily; may also be dosed twice daily) formulations and an IV injection. The ER oral formulation is not available in Canada. Available valproate formulations include valproic acid, valproate sodium, and divalproex sodium (also known as valproate semisodium) salts. All doses in this monograph are expressed as the equivalent amounts of valproic acid.
Oral, IV: Lower initial doses are recommended due to decreased elimination and increased incidences of somnolence in the elderly. No specific dosage recommendations are provided by the manufacturer; however, some experts suggest initial doses of 125 to 250 mg/day and gradually increasing the dose by 125 to 250 mg/day every 2 to 5 days up to a usual daily dose of 500 to 1,000 mg/day (Sajatovic 2002). Monitor closely for adverse events (eg, sedation, dehydration, decreased nutritional intake). Safety and efficacy for use in patients >65 years of age have not been studied for migraine prophylaxis.
Dosing conversions: Note: The ER formulation is not available in Canada:
Conversion from immediate release to DR or ER: Refer to adult dosing.
Conversion from DR to ER: Refer to adult dosing.
Conversion to IV valproate preparations: Refer to adult dosing.
Dosing: Pediatric
Note: Use of Depakote ER in pediatric patients <10 years of age is not recommended; do not confuse Depakote ER with Depakote. Erroneous substitution of Depakote (delayed-release tablets) for Depakote ER has resulted in toxicities; only Depakote ER is intended for once daily administration.
Migraine, prophylaxis:
Divalproex sodium (eg, Depakote tablets):
Children ≥5 years and Adolescents ≤16 years: Limited data available: Oral: Initial 10 to 15 mg/kg/day in 2 divided doses; maximum initial dose: 250 mg/dose. Titrate as needed over 4 to 6 weeks to 40 to 45 mg/kg/day in 2 divided doses; maximum daily dose: 1,000 mg/day (AAN [Lewis 2004]; Ashrafi 2005; Caruso 2000; Gunner 2008). Dosing based on multiple pediatric trials. In one open-label trial of divalproex sodium (DVS) (n=42; age range: 7 to 16 years); dose was initiated at 15 mg/kg/day in 2 divided doses and increased as needed over 6 weeks to 45 mg/kg/day in 2 divided doses. After 4 months, 78.5% of subjects had a 50% decrease in headaches frequency, 14.2% had a 75% decrease in headache frequency, and 9.5% became headache free (Caruso 2000). In a randomized comparative trial of pediatric patients aged 4 to 15 years, sodium valproate (n=54) was initiated at 10 mg/kg/day in 2 divided doses and titrated based on clinical response and tolerability up to a maximum dose of 40 mg/kg/day in divided doses; similar efficacy to propranolol (n=56) was observed with regards to decrease in headache frequency by >50%, mean headache duration, headache severity, and improved response to rescue medications (Ashrafi 2005). A small (n=10) open-label trial of pediatric patients 9 to 17 years showed a statistically significant decrease in mean frequency of headache attacks, severity, and duration with divalproex sodium therapy using a daily dose range of 500 to 1,000 mg/day (Serdaroglu 2002).
Adolescents ≥17 years: Depakote: Oral: 250 mg twice daily; adjust dose based on patient response; maximum daily dose: 1,000 mg/day.
Depakote ER: Limited data available: Children ≥12 years and Adolescents: Oral: 500 mg once daily for 15 days, may increase to 1,000 mg once daily; adjust dose based on patient response; usual dosage range: 250 to 1,000 mg/day; dose should be individualized; if smaller dosage adjustments are needed, use Depakote delayed-release tablets; results from a Phase 3, long-term (12 months) open-label trial of 241 patients (age: 12 to 17 years) showed a 75% decrease in median 4-week headache days between the first and fourth months of the trial (Apostol 2009a). In a short-term (12 weeks), double-blind, randomized placebo-controlled trial of 304 patients (age: 12 to 17 years), Depakote ER (250 to 1,000 mg/day) was no different than placebo at reducing the 4-week headache rate; however, a large placebo effect was observed in the study population (Apostol 2008).
Migraine, treatment; refractory: Limited data available, efficacy results variable, optimal regimen not established:
Intermittent IV: Adolescents 500 or 1,000 mg infused at 50 mg/minute; a repeat dose of 500 mg may be administered if pain relief not observed (Reiter 2005; Sheridan 2015); dosing based on two retrospective reports that evaluated experience in 43 patients treated for acute migraine attack(s) (n=60; some subjects presented with multiple attacks); the mean age in both reports was 15 years and the majority of patients received 1,000 mg doses. One trial evaluated 48 clinic visits for acute migraine attack in 31 patients; adequate pain relief was reported in 77.6% of visits (n=45) after a single valproic acid dose; the mean time to achieve maximum pain relief was 63 ± 31 minutes (range: 15 to 160 minutes) after a single dose of valproic acid; maximum pain reduction following a repeat 500 mg dose was observed at 124 ± 62 minutes (range: 20 to 250 minutes) (Reiter 2005).
Continuous IV infusion: Children ≥4 years and Adolescents:
Loading dose: IV: 20 mg/kg; maximum dose: 2,000 mg/dose infused over 30 to 60 minutes.
Continuous infusion: IV: Initial: 1 mg/kg/hour; adjust to maintain target serum concentrations of 80 to 100 mcg/mL (assessed at 2 to 4 hours and at 24 hours after loading dose) (Cook 2016; Taylor 2007; Zafar 2018). Dosing based on a retrospective report including 83 patients (mean age: 12.9 years; range: 4 to 18 years) who received IV valproate for status migrainosus after failing home oral therapy and initial IV therapy in the emergency department (diphenhydramine, metoclopramide, and ketorolac); the mean reported rate was 1 mg/kg/hour, and an excellent response (100% pain reduction) was reported in 55 (66.3%) patients; within the responder group, 56% reported response within 16 hours and 76% within 24 hours. Patients were then transitioned to oral valproic acid therapy migraine prophylaxis therapy on the delayed-released formulation initiated at the same dosage as last 24 hours of IV infusion (Zafar 2018).
Seizures disorders: Note: Due to the increased risk of valproic acid and derivatives-associated hepatotoxicity in patients <2 years, valproic acid and derivatives are not preferred agents in this population.
Oral:
General dosing (including focal onset seizures with impaired consciousness or awareness [complex partial seizures], mixed seizure disorders, tonic-clonic): Children and Adolescents: Limited data available for some seizure types and ages <10 years (Piña-Garza 2013): Initial: 10 to 15 mg/kg/day in 1 to 3 divided doses; increase by 5 to 10 mg/kg/day at weekly intervals until seizures are controlled or side effects preclude further increases; daily doses >250 mg should be given in divided doses; maintenance: 30 to 60 mg/kg/day in 2 to 3 divided doses; Depakote and Depakote Sprinkle can be given twice daily; Note: Children receiving more than 1 anticonvulsant (ie, polytherapy) may require doses up to 100 mg/kg/day in 3 to 4 divided doses.
Generalized nonmotor (absence) seizures, focal onset seizures with or without impaired consciousness or awareness (simple and complex): Children and Adolescents: Initial: 15 mg/kg/day in 1 to 3 divided doses; increase by 5 to 10 mg/kg/day at weekly intervals until seizures are controlled or side effects preclude further increases; daily doses >250 mg should be given in divided doses; maintenance: 30 to 60 mg/kg/day in 2 to 3 divided doses; Depakote and Depakote Sprinkle can be given twice daily.
Conversion to Depakote ER from a stable dose of immediate release or delayed release: May require an increase in the total daily dose between 8% and 20% administered once daily to maintain similar serum concentrations. For doses that do not directly convert to a Depakote ER dose form, clinicians may consider increasing to the next highest dose of the immediate or delayed-release (eg, Depakote) formulation before converting to the appropriate daily dose of Depakote ER.
Conversion to monotherapy from adjunctive therapy: The concomitant antiepileptic drug (AED) can be decreased by ~25% every 2 weeks. This reduction may be started at initiation of valproic acid therapy or delayed by 1 to 2 weeks if there is a concern that seizures are likely to occur with a reduction. The speed and duration of withdrawal of the concomitant AED can be highly variable, and patients should be monitored closely during this period for increased seizure frequency.
Parenteral: Children and Adolescents: Limited data available in some cases depending on seizure types and age (Piña-Garza 2013): IV: Total daily IV dose is equivalent to the total daily oral dose; however, IV dose should be divided with a frequency of every 6 hours; if IV form is administered 2 to 3 times/day, close monitoring of trough concentrations is recommended; switch patients to oral product as soon as clinically possible as IV use >14 days has not been studied.
Rectal: Limited data available: Children and Adolescents: Dilute oral syrup 1:1 with water for use as a retention enema (Graves 1987):
Loading dose: 17 to 20 mg/kg once.
Maintenance: 10 to 15 mg/kg/dose every 8 hours.
Status epilepticus; urgent therapy/second-line therapy or refractory: Limited data available:
Loading dose: Initial:
American Epilepsy Society guidelines (AES [Glauser 2016]): Infants, Children, and Adolescents: IV: 40 mg/kg as a single dose; maximum dose: 3,000 mg/dose.
Neurocritical care guidelines (NCS [Brophy 2012]): Infants, Children, and Adolescents: IV: 20 to 40 mg/kg; may be followed by an additional 20 mg/kg after 10 minutes if needed.
Maintenance dose: Continuous IV infusion: 5 mg/kg/hour after the loading dose was used in pediatric continuous IV infusion studies (Mehta 2007; Uberall 2000); once patients were seizure-free for 6 hours, the infusion rate was decreased by 1 mg/kg/hour every 2 hours (Mehta 2007). Lower initial infusion rates of 1 mg/kg/hour have also been described (Malamiri 2012).
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Reconstitution
Parenteral: IV: Manufacturer's labeling recommends diluting dose in 50 mL of D5W, NS, or LR.
Rectal: Dilute oral solution or syrup 1:1 with an equal volume of water prior to administration (Graves 1987)
Administration
Oral: Oral valproate products may cause GI upset; taking with food or slowly increasing the dose may decrease GI upset should it occur.
Divalproex sodium tablets (delayed release, extended release, and enteric coated [Canadian product]) and valproic acid capsules (immediate release): Swallow whole; do not crush or chew.
Divalproex sodium delayed release sprinkle capsules: May be swallowed whole or capsule opened and sprinkled on small amount (1 teaspoonful) of soft food (eg, pudding, applesauce) to be used immediately (do not store or chew).
Bariatric surgery: Tablet, extended and delayed release: Some institutions may have specific protocols that conflict with these recommendations; refer to institutional protocols as appropriate. Delayed-release and extended-release tablets should be swallowed whole. Do not crush or chew. Immediate-release capsule formulation is available but should not be chewed or crushed. Sprinkle capsules, oral solution, and injectable formulations are available. If safety and efficacy can be effectively monitored, no change in formulation or administration is required after bariatric surgery; however, close clinical monitoring is advised in the immediate postoperative phase for the theoretical circumstance of reduced absorption after bariatric surgery. Conversion to oral solution should be considered for high-risk labeled and off-label clinical indications (ie, seizure, mania, agitation).
IV: For IV use only.
Seizures: Following dilution to final concentration, manufacturer's labeling recommends administering over 60 minutes at a rate ≤20 mg/minute.
Status epilepticus: Loading dose: 3 to 6 mg/kg/minute (NCS [Brophy 2012]); however, evidence suggest rates of 10 mg/kg/minute may be safely used with doses up to 30 mg/kg (Limdi 2007).
Storage
Oral capsules:
Immediate release: Store at 15°C to 25°C (59°F to 77°F).
Delayed release: Store at 25°C (77° F); excursions are permitted between 15°C and 30°C (59°F and 86°F).
Oral sprinkle capsules: Delayed release: Store below 25°C (77°F).
Oral solution: Immediate release: Store below 30°C (86°F).
Oral tablets:
Delayed release: Store below 30°C (86°F).
Extended release: Store tablets at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F).
Immediate release [Canadian product]: Store at 15°C and 25°C (59°F and 77°F). Protect from light.
IV: Store at controlled room temperature 15°C to 30°C (59°F to 86°F). Stable in D5W, NS, and LR for at least 24 hours when stored in glass or PVC.
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Azelastine (Nasal): May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Barbiturates: Valproate Products may increase the serum concentration of Barbiturates. Barbiturates may decrease the serum concentration of Valproate Products. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Management: Use caution if coadministering blonanserin and CNS depressants; dose reduction of the other CNS depressant may be required. Strong CNS depressants should not be coadministered with blonanserin. Consider therapy modification
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Bupivacaine: Valproate Products may enhance the adverse/toxic effect of Bupivacaine. Specifically, the risk of methemoglobinemia may be increased. Monitor therapy
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabidiol: Valproate Products may enhance the hepatotoxic effect of Cannabidiol. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: Valproate Products may increase serum concentrations of the active metabolite(s) of CarBAMazepine. Parent carbamazepine concentrations may be increased, decreased, or unchanged. CarBAMazepine may decrease the serum concentration of Valproate Products. Monitor therapy
Carbapenems: May decrease the serum concentration of Valproate Products. Management: Concurrent use of carbapenem antibiotics with valproic acid is generally not recommended. Alternative antimicrobial agents should be considered, but if a concurrent carbapenem is necessary, consider additional anti-seizure medication. Consider therapy modification
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
ChlorproMAZINE: May increase the serum concentration of Valproate Products. Monitor therapy
Cholestyramine Resin: May decrease the serum concentration of Valproic Acid and Derivatives. Management: Separate administration of valproic acid and cholestyramine by at least 3 hours whenever possible in order to minimize this interaction. The impact of concurrent cholestyramine on delayed- or extended-release valproic acid is uncertain. Consider therapy modification
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Cosyntropin: May enhance the hepatotoxic effect of Valproate Products. Management: Avoid concomitant use of Synacthen Depot (dosage form available in Canada) with valproic acid. Avoid combination
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Estrogen Derivatives (Contraceptive): May decrease the serum concentration of Valproate Products. Monitor therapy
Ethosuximide: May decrease the serum concentration of Valproate Products. Valproate Products may increase the serum concentration of Ethosuximide. Monitor therapy
Felbamate: May increase the serum concentration of Valproate Products. Management: Initiate felbamate at 1200 mg/day in 3-4 divided doses in patients receiving valproate products. Also reduce the valproate product dose by 20%. Monitor for increased valproate concentrations/effects and decreased concentrations/effects of felbamate. Consider therapy modification
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Management: Reduce the dose of CNS depressants when combined with flunitrazepam and monitor patients for evidence of CNS depression (eg, sedation, respiratory depression). Use non-CNS depressant alternatives when available. Consider therapy modification
Fosphenytoin-Phenytoin: Valproate Products may decrease the protein binding of Fosphenytoin-Phenytoin. This appears to lead to an initial increase in the percentage of unbound (free) phenytoin and to a decrease in total phenytoin concentrations. Whether concentrations of free phenytoin are increased is unclear. With long-term concurrent use, total phenytoin concentrations may increase. Fosphenytoin-Phenytoin may decrease the serum concentration of Valproate Products. Monitor therapy
Fotemustine: Valproate Products may enhance the adverse/toxic effect of Fotemustine. Monitor therapy
GuanFACINE: May increase the serum concentration of Valproate Products. Monitor therapy
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
LamoTRIgine: Valproate Products may enhance the adverse/toxic effect of LamoTRIgine. Valproate Products may increase the serum concentration of LamoTRIgine. Management: Lamotrigine dose reductions are needed when combined with valproate. See full interaction monograph for details. Increase monitoring for lamotrigine toxicity (eg, rash, hematologic toxicities) when these agents are combined. Consider therapy modification
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lesinurad: Valproate Products may increase the serum concentration of Lesinurad. Avoid combination
Lisuride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
LORazepam: Valproate Products may increase the serum concentration of LORazepam. Management: Reduce lorazepam dose 50% during coadministration with valproate products. Monitor for increased lorazepam effects, particularly CNS depression. Consider therapy modification
Lumateperone: Valproate Products may increase the serum concentration of Lumateperone. Avoid combination
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. If anticonvulsants are being used for another indication, monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce the usual dose of CNS depressants by 50% if starting methotrimeprazine until the dose of methotrimeprazine is stable. Monitor patient closely for evidence of CNS depression. Consider therapy modification
Methylfolate: May decrease the serum concentration of Valproate Products. Monitor therapy
Metoclopramide: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May diminish the therapeutic effect of Anticonvulsants. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Minoxidil (Systemic): Valproate Products may increase the serum concentration of Minoxidil (Systemic). Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
OLANZapine: Valproate Products may decrease the serum concentration of OLANZapine. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
OXcarbazepine: Valproate Products may decrease the serum concentration of OXcarbazepine. Monitor therapy
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Oxybate Salt Products: Valproate Products may increase the serum concentration of Oxybate Salt Products. Management: Decrease the dose of the oxybate salt product by at least 20% when initiating therapy with valproate products. When initiating oxybate salt products in patients taking valproate products, use a lower starting dose of the oxybate salt. Consider therapy modification
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paliperidone: Valproate Products may increase the serum concentration of Paliperidone. Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pivmecillinam: Valproate Products may enhance the adverse/toxic effect of Pivmecillinam. Specifically, the risk for carnitine deficiency may be increased. Avoid combination
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Primidone: Valproate Products may decrease the metabolism of Primidone. More specifically, the metabolism of phenobarbital, primidone's primary active metabolite, may be decreased. Primidone may increase the serum concentration of Valproate Products. Monitor therapy
Propofol: Valproate Products may enhance the therapeutic effect of Propofol. Monitor therapy
Protease Inhibitors: May decrease the serum concentration of Valproate Products. Monitor therapy
RifAMPin: May decrease the serum concentration of Valproate Products. Management: Doses of valproate products may require adjustment when starting or stopping concurrent rifampin. Monitor plasma valproate concentrations closely and monitor for possible changes in clinical response. Consider therapy modification
RisperiDONE: Valproate Products may enhance the adverse/toxic effect of RisperiDONE. Generalized edema has developed. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: Valproate Products may increase the serum concentration of Rufinamide. Management: Initiate rufinamide at a dose less than 10 mg/kg/day (children) or 400 mg/day (adults) in patients receiving valproic acid. In patients receiving rufinamide, initiate valproic acid at a low dose and titrate based on clinical response. Consider therapy modification
Salicylates: May increase the serum concentration of Valproate Products. Monitor therapy
Sapropterin: Valproate Products may decrease the serum concentration of Sapropterin. Specifically, valproate products may decrease tissue concentrations of tetrahydrobiopterin. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Temozolomide: Valproate Products may enhance the adverse/toxic effect of Temozolomide. Valproate Products may increase the serum concentration of Temozolomide. Monitor therapy
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Topiramate: May enhance the adverse/toxic effect of Valproate Products. Monitor therapy
Tricyclic Antidepressants: Valproate Products may increase the serum concentration of Tricyclic Antidepressants. Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Urea Cycle Disorder Agents: Valproate Products may diminish the therapeutic effect of Urea Cycle Disorder Agents. More specifically, Valproate Products may increase plasma ammonia concentrations and thereby increase the doses of Urea Cycle Disorder Agents needed to maintain concentrations in the target range. Monitor therapy
Vorinostat: Valproate Products may enhance the thrombocytopenic effect of Vorinostat. This may increase the risk of gastrointestinal bleeding. Monitor therapy
Warfarin: Valproate Products may decrease the protein binding of Warfarin. Monitor therapy
Zidovudine: Valproate Products may increase the serum concentration of Zidovudine. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
May cause a false-positive result for urine ketones (valproate partially eliminated as a keto-metabolite in the urine); may alter thyroid function tests
Adverse Reactions
The following adverse drug reactions and incidences are derived from product labeling unless otherwise specified.
As reported with oral administration, unless otherwise noted.
>10%:
Central nervous system: Headache (oral: 31%; intravenous: 3% to 4%), drowsiness (oral: 7% to 30%; intravenous: 2% to 11%), dizziness (oral: 12% to 25%; intravenous: 5% to 7%), insomnia (>1% to 15%), pain (oral: 11%; intravenous: 1%), nervousness (oral: 7% to 11%; intravenous: <1%)
Dermatologic: Alopecia (>1% to 24%)
Gastrointestinal: Nausea (oral: 15% to 48%; intravenous: 3% to 6%), vomiting (oral: 7% to 27%; intravenous: 1%), abdominal pain (oral: 7% to 23%; intravenous: 1%), diarrhea (oral: 7% to 23%; intravenous: <1%), dyspepsia (7% to 23%), anorexia (>1% to 12%)
Hematologic & oncologic: Thrombocytopenia (1% to 27%; dose related)
Infection: Infection (≤20%)
Neuromuscular & skeletal: Tremor (≤57%), asthenia (6% to 27%; intravenous: 7%)
Ophthalmic: Diplopia (>1% to 16%), visual disturbance (amblyopia, blurred vision ≤1% to 12%)
Respiratory: Flu-like symptoms (>1% to 12%)
Miscellaneous: Accidental injury (>1% to 11%)
1% to 10%:
Cardiovascular: Peripheral edema (>1% to 8%), edema (>1% to 5%), facial edema (>1% to 5%), hypertension (>1% to 5%), hypotension (1% to 5%), orthostatic hypotension (1% to 5%), palpitations (>1% to 5%), vasodilation (oral: >1% to 5%; intravenous: <1%), tachycardia (>1% to <5%), chest pain (2%)
Central nervous system: Ataxia (>1% to 8%), amnesia (>1% to 7%), paresthesia (≤7%), abnormality in thinking (>1% to 6%), emotional lability (>1% to 6%), abnormal dreams (>1% to 5%), abnormal gait (>1% to 5%), confusion (>1% to 5%), depression (>1% to 5%), hallucination (>1% to 5%), hypertonia (>1% to 5%), speech disturbance (>1% to 5%), tardive dyskinesia (>1% to 5%), agitation (1% to 5%), catatonia (1% to 5%), chills (1% to 5%), hyperreflexia (1% to 5%), vertigo (1% to 5%), anxiety (>1% to <5%), malaise (>1% to <5%), myasthenia (>1% to <5%), personality disorder (>1% to <5%), twitching (>1% to <5%), sleep disorder (>1%)
Dermatologic: Skin rash (>1% to 6%), maculopapular rash (>1% to 5%), pruritus (>1% to 5%), xeroderma (>1% to 5%), diaphoresis (oral: >1%; intravenous: <1%), erythema nodosum (>1%), vesiculobullous dermatitis (>1%), furunculosis (1% to 5%), seborrhea (1% to 5%)
Endocrine & metabolic: Weight gain (>1% to 9%), weight loss (6%), amenorrhea (>1% to <5%), menstrual disease (>1%)
Gastrointestinal: Increased appetite (>1% to 6%), constipation (>1% to 5%), flatulence (>1% to 5%), periodontal abscess (>1% to 5%), fecal incontinence (1% to 5%), gastroenteritis (1% to 5%), glossitis (1% to 5%), stomatitis (1% to 5%), xerostomia (1% to 5%), eructation (>1% to <5%), hematemesis (>1% to <5%), pancreatitis (>1% to <5%), dysgeusia (2%), dysphagia (>1%), gingival hemorrhage (>1%), hiccups (>1%), oral mucosa ulcer (>1%)
Genitourinary: Cystitis (>1% to 5%), dysmenorrhea (>1% to 5%), dysuria (>1% to 5%), urinary incontinence (>1% to 5%), vaginal hemorrhage (>1% to 5%), urinary frequency (>1% to <5%), vaginitis (>1% to <5%)
Hematologic & oncologic: Ecchymoses (>1% to 5%), petechia (>1% to <5%), hypoproteinemia (>1%), prolonged bleeding time (>1%)
Hepatic: Increased serum alanine aminotransferase (>1% to <5%), increased serum aspartate aminotransferase (>1% to <5%)
Infection: Viral infection (>1% to 5%), fungal infection (>1%)
Local: Pain at injection site (intravenous: 3%), injection site reaction (intravenous: 2%)
Neuromuscular & skeletal: Back pain (>1% to 8%), arthralgia (>1% to 5%), discoid lupus erythematosus (>1% to 5%), lower limb cramps (>1% to 5%), hypokinesia (1% to 5%), neck pain (1% to 5%), neck stiffness (1% to 5%), osteoarthritis (1% to 5%), dysarthria (>1% to <5%), myalgia (>1% to <5%)
Ophthalmic: Nystagmus disorder (1% to 8%), conjunctivitis (1% to 5%), dry eye syndrome (1% to 5%), eye pain (1% to 5%), photophobia (>1%)
Otic: Tinnitus (1% to 7%), deafness (>1% to 5%), otitis media (>1% to <5%)
Respiratory: Pharyngitis (oral: 2% to 8%; intravenous: <1%), bronchitis (5%), rhinitis (>1% to 5%), dyspnea (1% to 5%), cough (>1% to <5%), epistaxis (>1% to <5%), pneumonia (>1% to <5%), sinusitis (>1% to <5%)
Miscellaneous: Fever (>1% to 6%)
<1%, postmarketing, and/or case reports: Abnormal behavior, abnormal thyroid function tests, acute intermittent porphyria, aggressive behavior, agranulocytosis, anaphylaxis, anemia, aplastic anemia, asthenospermia, azoospermia, bone fracture, bone marrow depression, bradycardia, brain disease (rare), breast hypertrophy, cerebral atrophy (reversible or irreversible), change in prothrombin time, changes of hair (color, texture), coma (rare), decreased bone mineral density, decreased plasma carnitine concentrations, decreased platelet aggregation, decreased spermatozoa motility, dementia, developmental delay (learning disorder), disturbance in attention, drug reaction with eosinophilia and systemic symptoms, emotional disturbance, eosinophilia, erythema multiforme, euphoria, Fanconi-like syndrome (rare, in children), female hyperandrogenism, galactorrhea not associated with childbirth, hemorrhage, hepatic failure, hepatotoxicity, hirsutism, hostility, hyperactive behavior, hyperammonemia, hyperammonemic encephalopathy (in patients with UCD), hyperglycinemia, hypersensitivity angiitis, hypersensitivity reaction, hypoesthesia, hypofibrinogenemia, hyponatremia, hypothermia, increased testosterone level, injection site inflammation, leukopenia, lymphocytosis, macrocytosis, male infertility, myelatelia, nail bed changes, nail disease, oligospermia, ostealgia, osteopenia, osteoporosis, pancytopenia, parkinsonism (Easterford 2004), parotid gland enlargement, polycystic ovary syndrome (rare), psychomotor disturbance, psychosis, seizure (paradoxical), severe hypersensitivity reaction (with multiorgan dysfunction), SIADH, skin photosensitivity, sleep disturbance, spermatozoa disorder (abnormal morphology), Stevens-Johnson syndrome, suicidal ideation, suicidal tendencies, toxic epidermal necrolysis (rare), urinary incontinence, urinary tract infection
ALERT: U.S. Boxed Warning
Hepatotoxicity:Hepatic failure resulting in fatalities has occurred in patients receiving valproate. These incidents usually have occurred during the first 6 months of treatment. Serious or fatal hepatotoxicity may be preceded by nonspecific symptoms such as malaise, weakness, lethargy, facial edema, anorexia, and vomiting. In patients with epilepsy, a loss of seizure control may also occur. Patients should be monitored closely for appearance of these symptoms. Serum liver tests should be performed prior to therapy and at frequent intervals thereafter, especially during the first 6 months.
Children <2 years of age are at a considerably increased risk of developing fatal hepatotoxicity, especially those on multiple anticonvulsants, those with congenital metabolic disorders, those with severe seizure disorders accompanied by mental retardation, and those with organic brain disease. When these products are used in this patient group, they should be used with extreme caution and as a sole agent. The benefits of therapy should be weighed against the risks. The incidence of fatal hepatotoxicity decreases considerably in progressively older patient groups.
Patients with mitochondrial disease:There is an increased risk of valproate-induced acute liver failure and resultant deaths in patients with hereditary neurometabolic syndromes caused by DNA mutations of the mitochondrial DNA polymerase gamma (POLG) gene (eg, Alpers-Huttenlocher syndrome). Valproate is contraindicated in patients known to have mitochondrial disorders caused by POLG mutations and children younger than 2 years who are clinically suspected of having a mitochondrial disorder. In patients >2 years of age who are clinically suspected of having a hereditary mitochondrial disease, only use after other anticonvulsants have failed. This older group of patients should be closely monitored during treatment with valproate for the development of acute liver injury with regular clinical assessments and serum liver testing. POLG mutation screening should be performed in accordance with current clinical practice.
Fetal risk:Valproate can cause major congenital malformations, particularly neural tube defects (eg, spina bifida). In addition, valproate can cause decreased IQ scores and neurodevelopmental disorders following in utero exposure. Valproate is therefore contraindicated for prophylaxis of migraine headaches in pregnant women and in women of childbearing potential who are not using effective contraception. Valproate should not be used to treat women with epilepsy or bipolar disorder who are pregnant or who plan to become pregnant unless other medications have failed to provide adequate symptom control or are otherwise unacceptable. Valproate should not be administered to a woman of childbearing potential unless other medications have failed to provide adequate symptom control or are otherwise unacceptable. In such situations, effective contraception should be used.
A Medication Guide describing the risks of valproate is available for patients.
Pancreatitis:Cases of life-threatening pancreatitis have been reported in both children and adults receiving valproate. Some of the cases have been described as hemorrhagic with a rapid progression from initial symptoms to death. Cases have been reported shortly after initial use as well as after several years of use. Patients and guardians should be warned that abdominal pain, nausea, vomiting, and/or anorexia can be symptoms of pancreatitis that require prompt medical evaluation. If pancreatitis is diagnosed, valproate should ordinarily be discontinued. Alternative treatment for the underlying medical condition should be initiated as clinically indicated.
Warnings/Precautions
Concerns related to adverse effects:
• Blood disorders: May cause dose-related thrombocytopenia, inhibition of platelet aggregation, and bleeding. In some cases, platelet counts may be normalized with continued treatment; however, reduce dose or discontinue drug if patient develops evidence of hemorrhage, bruising, or a disorder of hemostasis/coagulation. Evaluate platelet counts prior to initiating therapy and periodically thereafter. Probability of thrombocytopenia increases with total valproate levels ≥110 mcg/mL in females or ≥135 mcg/mL in males. In addition to platelets, valproate may be associated with a decrease in other cell lines and myelodysplasia.
• Brain atrophy: Reversible and irreversible cerebral and cerebellar atrophy have been reported; motor and cognitive function should be routinely monitored to assess for signs and symptoms of brain atrophy.
• CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
• Hepatic failure: [US Boxed Warning]: Hepatic failure resulting in fatalities has occurred in patients, usually in the initial 6 months of therapy; children <2 years of age are at considerable risk. Risk is also increased in patients with hereditary neurometabolic syndromes caused by DNA mutations of the mitochondrial DNA polymerase gamma (POLG) gene (eg, Alpers-Huttenlocher syndrome [AHS]). Other risk factors include organic brain disease, mental retardation with severe seizure disorders, congenital metabolic disorders, and patients on multiple anticonvulsants. Monitor patients closely for appearance of malaise, weakness, facial edema, anorexia, jaundice, and vomiting; discontinue immediately with signs/symptom of significant or suspected impairment. Liver function tests should be performed at baseline and at regular intervals after initiation of therapy, especially within the first 6 months. Hepatic dysfunction may progress despite discontinuing treatment. Should only be used as monotherapy and with extreme caution in children <2 years of age and/or patients at high risk for hepatotoxicity.
• Hyperammonemia/encephalopathy: Hyperammonemia and/or encephalopathy, sometimes fatal, has been reported following the initiation of valproate therapy and may be present with normal transaminase levels. Ammonia levels should be measured in patients who develop unexplained lethargy and vomiting, or changes in mental status or in patients who present with hypothermia. Discontinue therapy if ammonia levels are increased and evaluate for possible urea cycle disorder (UCD). Hyperammonemic encephalopathy has been reported in patients with UCD, particularly ornithine transcarbamylase deficiency. Use is contraindicated in patients with known UCD. Evaluation of UCD should be considered for the following patients prior to the start of therapy: History of unexplained encephalopathy or coma; encephalopathy associated with protein load; pregnancy or postpartum encephalopathy; unexplained mental retardation; history of elevated plasma ammonia or glutamine; history of cyclical vomiting and lethargy; episodic extreme irritability, ataxia; low BUN or protein avoidance; family history of UCD or unexplained infant deaths (particularly male); or signs or symptoms of UCD (hyperammonemia, encephalopathy, respiratory alkalosis). Hyperammonemia and/or encephalopathy may also occur with concomitant topiramate therapy in patients who previously tolerated monotherapy with either medication.
• Hypothermia: Hypothermia (unintentional drop in core body temperature to <35°C/95°F) has been reported with valproate therapy; hypothermia may or may not be associated with hyperammonemia; may also occur with concomitant topiramate therapy following topiramate initiation or dosage increase.
• Multiorgan hypersensitivity reactions (also known as drug reaction with eosinophilia and systemic symptoms [DRESS]): Potentially serious, sometimes fatal multiorgan hypersensitivity reactions have rarely been reported with some antiepileptic drugs including valproate therapy in adults and children; monitor for signs and symptoms of possible disparate manifestations associated with lymphatic, hepatic, renal, and/or hematologic organ systems; discontinuation and conversion to alternate therapy may be required.
• Pancreatitis: [US Boxed Warning]: Cases of life-threatening pancreatitis, occurring at the start of therapy or following years of use, have been reported in adults and children. Some cases have been hemorrhagic with rapid progression of initial symptoms to death. Promptly evaluate symptoms of abdominal pain, nausea, vomiting, and/or anorexia; should generally be discontinued if pancreatitis is diagnosed.
• Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify healthcare provider immediately if symptoms occur.
Disease-related concerns:
• Acute head trauma: Not recommended for post-traumatic seizure prophylaxis in patients with acute head trauma; study results for this indication suggested increased mortality with IV valproate sodium use compared to IV phenytoin.
• Hepatic impairment: Contraindicated with significant impairment.
• Mitochondrial disease: [US Boxed Warning]: Risk of valproate-induced acute liver failure and death is increased in patients with hereditary neurometabolic syndromes caused by DNA mutations of the mitochondrial polymerase gamma (POLG) gene (eg, Alpers Huttenlocher syndrome [AHS]). Use is contraindicated in patients with known mitochondrial disorders caused by POLG mutations and children <2 years of age suspected of having a POLG-related disorder. Use in children ≥2 years of age suspected of having a POLG-related disorder only after other anticonvulsants have failed and with close monitoring for the development of acute liver injury. POLG mutation testing should be performed in accordance with current clinical practice.
Special populations:
• Elderly: Use with caution as elderly patients may be more sensitive to sedating effects and dehydration; in some elderly patients with somnolence, concomitant decreases in nutritional intake and weight loss were observed. Reduce initial dosages in elderly and closely monitor fluid status, nutritional intake, somnolence, and other adverse events.
• Pediatric: Children <2 years of age are at increased risk for fatal hepatotoxicity; if valproate therapy is used in this age group, use with extreme caution and only as monotherapy.
• Pregnancy: [US Boxed Warning]: Valproate can cause major congenital malformations, particularly neural tube defects (eg, spina bifida). In addition, valproate can cause decreased IQ scores and neurodevelopmental disorders following in utero exposure. Valproate is contraindicated for prophylaxis of migraine headaches in pregnant women and in women of childbearing potential who are not using effective contraception. Valproate should not be used to treat women with epilepsy or bipolar disorder who are pregnant or who plan to become pregnant unless other medications have failed to provide adequate symptom control or are otherwise unacceptable. Valproate should not be administered to a woman of childbearing potential unless other medications have failed to provide adequate symptom control or are otherwise unacceptable. In such situations, effective contraception should be used.
Other warnings/precautions:
• Gastrointestinal: Medication residue in stool has been reported (rarely) with oral divalproex sodium formulations; some reports have occurred in patients with shortened GI transit times (eg, diarrhea) or anatomic GI disorders (eg, ileostomy, colostomy). In patients reporting medication residue in stool, it is recommended to monitor valproate level and clinical condition.
• Viral replication: In vitro studies have suggested valproate stimulates the replication of HIV and CMV viruses under experimental conditions. The clinical consequence of this is unknown, but should be considered when monitoring affected patients.
• Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal.
Monitoring Parameters
Liver enzymes (at baseline and frequently during therapy especially during the first 6 months), CBC with platelets (baseline and periodic intervals), PT/PTT (especially prior to surgery), serum ammonia (with symptoms of lethargy, mental status change), serum valproate levels; suicidality (eg, suicidal thoughts, depression, behavioral changes); motor and cognitive function (for signs or symptoms of brain atrophy); menstrual history to assess for polycystic ovary syndrome (at 3 to 6 month intervals for the first year, then annually) (CANMAT [Yatham 2018]).
Reproductive Considerations
[US Boxed Warning]: Due to the risks of adverse fetal events, valproate is contraindicated for prophylaxis of migraine headaches in women of childbearing potential who are not using effective contraception. Valproate should not be used to treat women with epilepsy or bipolar disorder who plan to become pregnant unless other medications have failed to provide adequate symptom control or are otherwise unacceptable. Valproate should not be administered to a woman of childbearing potential unless other medications have failed to provide adequate symptom control or are otherwise unacceptable. In such situations, effective contraception should be used.
Algorithms are available for the management of females of reproductive potential who are taking valproic acid for bipolar disorder. Non-pregnant women who are stable on mono-therapy and are planning a pregnancy should undergo a slow taper (>4 weeks); alternative treatment and a faster taper should be introduced in unstable patients during this time. Additional details are available for women planning a pregnancy who are on multiple medications (Anmella 2019).
When pregnancy is being planned in women with epilepsy, consider tapering off of therapy prior to conception if appropriate (Anmella 2019; Harden 2009a); abrupt discontinuation of therapy may cause status epilepticus and lead to maternal and fetal hypoxia.
Counsel women planning a pregnancy and girls at the onset of puberty regarding benefits and risk of valproate use during pregnancy. Folic acid decreases the risk of neural tube defects in the general population; supplementation with folic acid should be used prior to conception and during pregnancy in all females, including those taking valproate.
Cases of male infertility have been reported following valproate use.
Pregnancy Considerations
Valproate crosses the placenta (Harden 2009b).
[US Boxed Warning]: Valproate can cause major congenital malformations, particularly neural tube defects (eg, spina bifida). In addition, valproate can cause decreased IQ scores and neurodevelopmental disorders following in utero exposure. Neural tube defects, craniofacial defects (eg, oral clefts, craniosynostosis), cardiovascular malformations, hypospadias, and limb malformations (eg, clubfoot, polydactyly) have been reported. Information from the North American Antiepileptic Drug Pregnancy Registry notes the rate of major malformations to be 9% to 11% following an average exposure to valproate monotherapy 1,000 mg/day; this is an increase in congenital malformations when compared with monotherapy with other antiepileptic drugs (AED). Based on data from the CDC National Birth Defects Prevention Network, the risk of spinal bifida is approximately 1% to 2% following valproate exposure (general population risk estimated to be 0.06% to 0.07%).
Nonteratogenic adverse effects have also been reported. Decreased IQ scores have been noted in children exposed to valproate in utero when compared to children exposed to other antiepileptic medications or no antiepileptic medications; the risk of autism spectrum disorders may also be increased. Hearing loss or impairment may occur following in utero exposure. Fatal hepatic failure and hypoglycemia in infants have been noted in case reports following in utero exposure to valproate.
The pharmacokinetic properties of valproate in pregnancy are highly variable. If use is needed, monitoring of total and unbound serum concentrations should be done prior to and during pregnancy (Johannessen 2018). Clotting factor abnormalities (hypofibrinogenemia, thrombocytopenia, or decrease in other coagulation factors) may develop in the mother following valproate use during pregnancy; close monitoring of coagulation factors is recommended.
[US Boxed Warning]:Due to the risks of adverse fetal events, valproate is contraindicated for prophylaxisof migraine headaches in pregnant women. Valproate should not be used to treat women with epilepsy or bipolar disorder who are pregnant unless other medications have failed to provide adequate symptom control or are otherwise unacceptable. Current guidelines recommend complete avoidance of valproate for the treatment of epilepsy in pregnant women whenever possible (Harden 2009a).
A pregnancy registry is available for women who have been exposed to valproic acid. Patients may enroll themselves in the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling (888) 233-2334. Additional information is available at www.aedpregnancyregistry.org.
Patient Education
What is this drug used for?
• It is used to treat seizures.
• It is used to prevent migraine headaches.
• It is used to treat bipolar problems.
• It may be given to you for other reasons. Talk with the doctor.
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
• Headache
• Nausea
• Vomiting
• Dizziness
• Fatigue
• Constipation
• Diarrhea
• Abdominal pain
• Trouble sleeping
• Loss of strength and energy
• Lack of appetite
• Increased hunger
• Weight gain
• Weight loss
• Anxiety
• Flu-like signs
• Hair loss
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
• Infection
• Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
• Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
• Depression like thoughts of suicide, anxiety, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
• High ammonia level like abnormal heartbeat, abnormal breathing, confusion, pale skin, slow heartbeat, seizures, vomiting, or twitching.
• Chest pain
• Swelling of arms or legs
• Vision changes
• Trouble with memory
• Change in balance
• Abnormal gait
• Bruising
• Bleeding
• Purple or red spots on skin
• Unable to pass urine
• Change in amount of urine passed
• Swollen glands
• Muscle pain
• Muscle weakness
• Joint pain
• Joint swelling
• Tremors
• Involuntary eye movements
• Noise or ringing in the ears
• Cold sensation
• Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a limited summary of general information about the medicine's uses from the patient education leaflet and is not intended to be comprehensive. This limited summary does NOT include all information available about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not intended to provide medical advice, diagnosis or treatment and does not replace information you receive from the healthcare provider. For a more detailed summary of information about the risks and benefits of using this medicine, please speak with your healthcare provider and review the entire patient education leaflet.
More about valproic acid
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (62)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: fatty acid derivative anticonvulsants
- Breastfeeding
- En español
Patient resources
- Valproic acid drug information
- Valproic acid (Advanced Reading)
- Valproic Acid Capsules
- Valproate Injection
- Valproic Acid Liquid
Other brands
Valproate Sodium, Depakene, Depacon, Stavzor
Professional resources
- Valproate prescribing information
- Valproic Acid Capsules (FDA)
- Valproic Acid Oral Solution (FDA)
- Valproic Acid Syrup (FDA)
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.