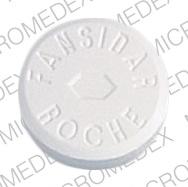
Pyrimethamine and sulfadoxine (Oral)
Generic name: pyrimethamine and sulfadoxine [ pir-i-METH-a-meen, sul-fa-DOX-een ]
Brand name: Fansidar
Drug class: Antimalarial combinations
Medically reviewed by Drugs.com. Last updated on May 17, 2023.
Fatalities associated with the administration of pyrimethamine/sulfadoxine have occurred due to severe reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis. Pyrimethamine/sulfadoxine prophylaxis must be discontinued at the first appearance of skin rash, if a significant reduction in the count of any formed blood elements is noted, or upon the occurrence of active bacterial or fungal infections .
Uses for pyrimethamine and sulfadoxine
Sulfadoxine , a sulfa medicine, and pyrimethamine combination is used to treat malaria. This medicine may also be used to prevent malaria in people who are living in, or will be traveling to, an area where there is a chance of getting malaria. Sulfadoxine and pyrimethamine combination may also be taken with other medicines for malaria, or may be used for other problems as determined by your doctor.
Since sulfadoxine and pyrimethamine combination may cause some serious side effects, it generally is used only to prevent or treat serious malaria infections in areas where it is known that other medicines may not work.
This medicine is available only with your doctor's prescription.
Before using pyrimethamine and sulfadoxine
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Sulfadoxine and pyrimethamine combination should not be used in infants up to 2 months of age.
Geriatric
Many medicines have not been studied specifically in older people. Therefore, it may not be known whether they work exactly the same way they do in younger adults or if they cause different side effects or problems in older people. There is no specific information comparing use of sulfadoxine and pyrimethamine combination in the elderly with use in other age groups.
Breast Feeding
Studies in women breastfeeding have demonstrated harmful infant effects. An alternative to this medication should be prescribed or you should stop breastfeeding while using this medicine.
Interactions with Medicines
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Aurothioglucose
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Carbamazepine
- Cholera Vaccine, Live
- Methotrexate
- Sapropterin
- Sulfamethoxazole
- Trimethoprim
- Zidovudine
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Aminolevulinic Acid
- Lorazepam
Interactions with Food/Tobacco/Alcohol
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your medicine with food, alcohol, or tobacco.
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Anemia or other blood problems—Patients with these problems may have an increase in side effects involving the blood
- Kidney disease or
- Liver disease—Patients with kidney and/or liver disease may have an increased chance of side effects
- Porphyria—This medicine may cause an attack of porphyria
- Seizure disorders, such as epilepsy—High doses of this medicine may increase the chance of convulsions (seizures)
Proper use of pyrimethamine and sulfadoxine
Do not give this medicine to infants younger than 2 months of age unless otherwise directed by your doctor. Also, keep this medicine out of the reach of children. Overdose is especially dangerous in children.
Sulfa-containing medicines are best taken with a full glass (8 ounces) of water. Several additional glasses of water should be taken every day, unless otherwise directed by your doctor. Drinking extra water will help to prevent some unwanted effects (e.g., kidney stones) of this medicine. If this medicine upsets your stomach or causes vomiting, it may be taken with meals or a snack.
For patients taking this medicine to prevent malaria :
- Your doctor may want you to start taking this medicine 1 to 2 weeks before you travel to an area where there is a chance of getting malaria. This will help you to see how you react to the medicine. Also, it will allow time for your doctor to change your medicine if you have a reaction to this medicine.
- Also, you should keep taking this medicine while you are in the area and for 4 weeks after you leave the area. No medicine will protect you completely from malaria. However, to protect you as completely as possible, it is important that you keep taking this medicine for the full time your doctor ordered. Also, if fever develops during your travels or within 2 months after you leave the area, check with your doctor immediately.
- This medicine works best when you take it on a regular schedule. For example, if you are to take it once a week, it is best to take it on the same day each week. Do not miss any doses. If you have any questions about this, check with your health care professional.
For patients taking this medicine to treat malaria :
- To help clear up your infection completely, take this medicine exactly as directed by your doctor.
For patients taking this medicine to self-treat presumed malaria:
- After you take this medicine to self-treat presumed malaria, you should continue to take your other medicine for malaria once a week.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For treatment of malaria:
- Adults and teenagers: 3 tablets as a single dose on the third day of quinine therapy.
- Children: Dose is based on body weight and must be determined by your doctor.
- For self-treatment of presumed malaria:
- Adults and teenagers: 3 tablets as a single dose when you get a fever and medical care is not available.
- Children 2 months of age and older: Dose is based on body weight and must be determined by your doctor. The dose may range from ½ tablet to 3 tablets taken as a single dose.
- For prevention of malaria:
- Adults and teenagers: 1 tablet once every seven days, or 2 tablets once every fourteen days.
- Children 2 months of age and older: Dose is based on body weight and must be determined by your doctor. The dose may range from ¼ tablet to ¾ tablet taken once every seven days, or ½ tablet to 1½ tablets taken once every fourteen days.
Missed Dose
If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Precautions while using pyrimethamine and sulfadoxine
If this medicine causes skin rash, itching, redness, sores in the mouth or on the genitals (sex organs), or sore throat, check with your doctor immediately. These may be early warning signs of more serious skin or related problems that could develop later.
Malaria is spread by mosquitoes. If you are living in, or will be traveling to, an area where there is a chance of getting malaria, the following mosquito-control measures will help to prevent infection:
- If possible, sleep under mosquito netting to avoid being bitten by malaria-carrying mosquitoes.
- Wear long-sleeved shirts or blouses and long trousers to protect your arms and legs, especially from dusk through dawn when mosquitoes are out.
- Apply mosquito repellant to uncovered areas of the skin from dusk through dawn when mosquitoes are out.
For patients taking this medicine to prevent malaria :
- It is very important that your doctor check your progress at regular visits. This medicine may cause blood problems, especially if it is taken for a long time.
- If this medicine causes anemia, your doctor may want you to take leucovorin (e.g., folinic acid, Wellcovorin) to help clear up the anemia. If so, it is important to take the leucovorin every day while you are taking this medicine. Do not miss any doses.
- Sulfadoxine and pyrimethamine combination may cause blood problems. These problems may result in a greater chance of certain infections, slow healing, and bleeding of the gums. Therefore, you should be careful when using regular toothbrushes, dental floss, and toothpicks. Dental work should be delayed until your blood counts have returned to normal. Check with your medical doctor or dentist if you have any questions about proper oral hygiene (mouth care) during treatment.
- Sulfadoxine and pyrimethamine combination may cause your skin to be more sensitive to sunlight than it is normally. Exposure to sunlight, even for brief periods of time, may cause a skin rash, itching, redness or other discoloration of the skin, or a severe sunburn. When you begin taking this medicine:
- Stay out of direct sunlight, especially between the hours of 10:00 a.m. and 3:00 p.m., if possible.
- Wear protective clothing, including a hat. Also, wear sunglasses.
- Apply a sun block product that has a skin protection factor (SPF) of at least 15. Some patients may require a product with a higher SPF number, especially if they have a fair complexion. If you have any questions about this, check with your health care professional.
- Apply a sun block lipstick that has an SPF of at least 15 to protect your lips.
- Do not use a sunlamp or tanning bed or booth.
If you have a severe reaction from the sun, check with your doctor.
For patients taking this medicine to self-treat presumed malaria:
- Seek medical help as soon as possible, especially if your symptoms do not improve within 48 hours.
Side Effects of pyrimethamine and sulfadoxine
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common
- Fever
- increased sensitivity of skin to sunlight
- irritation or soreness of tongue
- skin rash
Less common
- Black, tarry stools
- bleeding or crusting sores on lips
- blood in urine or stools
- chest pain
- chills
- cough or hoarseness
- loss of appetite
- lower back or side pain
- muscle cramps or pain
- nausea
- painful or difficult urination
- pinpoint red spots on skin
- redness, blistering, peeling, or loosening of skin
- sore mouth
- sore throat
- sores, ulcers, and/or white spots in mouth
- sores on lips
- swelling in upper abdominal area
- unusual bleeding or bruising
- unusual tiredness or weakness
- vomiting
- yellow eyes or skin
Rare
- Abdominal or stomach pain
- changes in facial skin color
- constipation
- fast or irregular breathing
- tenderness, itching, or burning of skin
- puffiness or swelling of the eyelids or around the eyes
- shortness of breath, troubled breathing, tightness in chest, and/or wheezing
- swelling of front part of neck
Symptoms of overdose
- Bleeding or bruising (severe)
- clumsiness or unsteadiness
- convulsions (seizures)
- fever and sore throat
- irritation or soreness of tongue
- loss of appetite
- unusual tiredness or weakness
- trembling
- vomiting (severe)
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Anxiety
- diarrhea
- drowsiness
- headache
- nervousness
Less common
- Pain in joints
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Commonly used brand name(s)
In the U.S.
- Fansidar
Pharmacologic Class: Folic Acid Antagonist
Chemical Class: Sulfonamide
More about pyrimethamine / sulfadoxine
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: antimalarial combinations
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.