Ivermectin (Monograph)
Brand name: Stromectol
Drug class: Anthelmintics
Warning
[Posted 04/10/2020]
AUDIENCE: Consumer, Health Professional, Pharmacy, Veterinary
ISSUE: FDA is concerned about the health of consumers who may self-medicate by taking ivermectin products intended for animals, thinking they can be a substitute for ivermectin intended for humans.
BACKGROUND: The FDA's Center for Veterinary Medicine has recently become aware of increased public visibility of the antiparasitic drug ivermectin after the announcement of a research article that described the effect of ivermectin on SARS-CoV-2 in a laboratory setting. The Antiviral Research pre-publication paper, “The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro” documents how SARS-CoV-2 (the virus that causes COVID-19) responded to ivermectin when exposed in a petri dish.
Ivermectin is FDA-approved for use in animals for prevention of heartworm disease in some small animal species, and for treatment of certain internal and external parasites in various animal species.
RECOMMENDATION:
-
People should never take animal drugs, as the FDA has only evaluated their safety and effectiveness in the particular animal species for which they are labeled. These animal drugs can cause serious harm in people.
-
People should not take any form of ivermectin unless it has been prescribed by a licensed health care provider and is obtained through a legitimate source.
-
Ivermectin is an important part of a parasite control program for certain species and should only be given to animals for approved uses or as prescribed by a veterinarian in compliance with the requirements for extra-label drug use.
-
If you are having difficulty locating a particular ivermectin product for your animal(s), FDA recommends that you consult with your veterinarian.
For more information visit the FDA website at: [Web] and [Web].
Introduction
Anthelmintic, pediculicide, scabicide; avermectin derivative.
Uses for Ivermectin
Pending revision, the material in this section should be considered in light of more recently available information in the MedWatch notification at the beginning of this monograph.
Ascariasis
Treatment of ascariasis† [off-label] caused by Ascaris lumbricoides. Albendazole and mebendazole are drugs of choice. Ivermectin also recommended as a drug of choice, but efficacy not clearly established.
Filariasis
Treatment of onchocerciasis (filariasis caused by Onchocerca volvulus; commonly referred to as river blindness). Drug of choice. Used in individual patients and in mass treatment and control programs. Does not kill adult O. volvulus worms, but decreases microfilarial load in skin for approximately 6–12 months following a single dose.
Treatment of filariasis caused by Mansonella streptocerca† [off-label]. Diethylcarbamazine (available in US from CDC) and ivermectin are drugs of choice. Diethylcarbamazine is potentially curative since it is active against both adult worms and microfilariae; ivermectin is effective only against microfilariae.
Has been used for treatment of filariasis caused by M. ozzardi† [off-label].
Treatment of filariasis caused by Wuchereria bancrofti† [off-label] or Brugia malayi† [off-label]; used alone or in conjunction with albendazole or diethylcarbamazine (available in US from CDC). Ivermectin does not kill adult worms, but may play an important role in mass treatment programs to suppress microfilaremia and thereby interrupt transmission in endemic areas. Diethylcarbamazine is usual drug of choice, especially for individual patients when the goal is to kill the adult worm.
Has been used in conjunction with albendazole to treat co-infection with W. bancrofti† and O. volvulus.
Has been used to reduce microfilaremia in the treatment of loiasis caused by Loa loa†. Generally not recommended since rapid killing of microfilariae increases risk of encephalopathy. (See Encephalopathy Risk in Onchocerciasis and Loiasis under Cautions.) Drug of choice for loiasis is diethylcarbamazine (available in US from CDC); preferred alternative is albendazole since it has a slower onset of action and decreased risk of encephalopathy compared with ivermectin.
Gnathostomiasis
Treatment of gnathostomiasis† caused by Gnathostoma spinigerum. Drug of choice (with or without surgical removal) is albendazole or ivermectin.
Hookworm Infections
Treatment of cutaneous larva migrans† (creeping eruption) caused by Ancylostoma braziliense (dog and cat hookworm) or Ancylostoma caninum (dog hookworm). Usually self-limited with spontaneous cure after several weeks or months; when treatment is indicated, drug of choice is albendazole or ivermectin.
Do not use for treatment of intestinal hookworm infections caused by Ancylostoma duodenale or Necator americanus. Appears to have little or no activity against these hookworms. Albendazole, mebendazole, and pyrantel pamoate are drugs of choice.
Strongyloidiasis
Treatment of intestinal (i.e., nondisseminated) strongyloidiasis caused by Strongyloides stercoralis. Drug of choice; alternative is albendazole.
Has been used for treatment of strongyloidiasis hyperinfection with disseminated disease† and for treatment of strongyloidiasis in immunocompromised patients. Drug of choice; alternative is albendazole. Repeated or prolonged ivermectin therapy or use with other drugs may be necessary; treatment failures reported.
Empiric treatment of strongyloidiasis before transplantation to prevent hyperinfection in hematopoietic stem cell transplant (HSCT) recipients†. Such treatment recommended by CDC, IDSA, ASBMT, and others for HSCT candidates with positive strongyloidiasis screening tests or possible exposure (e.g., unexplained eosinophilia and travel or residence history suggestive of S. stercoralis exposure [even if seronegative or stool-negative]). Data insufficient to recommend prophylaxis after HSCT to prevent recurrence of strongyloidiasis in such patients.
Trichuriasis
Treatment of trichuriasis† caused by Trichuris trichiura (whipworm). Albendazole is drug of choice; alternatives are mebendazole and ivermectin.
Pediculosis
Treatment of pediculosis capitis† (head lice infestation). AAP and others usually recommend topical treatment with OTC preparation of permethrin 1% or pyrethrins with piperonyl butoxide for initial treatment; other topical pediculicides (e.g., malathion 0.5%, benzyl alcohol 5%, spinosad 0.9%) recommended if OTC preparations ineffective or permethrin or pyrethrin resistance suspected. Oral ivermectin recommended as an alternative for infestations not responding to or resistant to topical agents.
Alternative for treatment of pediculosis pubis† (pubic lice infestation). Drug of choice is topical permethrin 1% or topical pyrethrins with piperonyl butoxide.
Alternative for treatment of pediculosis corporis† (body lice infestation). In some cases, body louse infestations may be treated by improved hygiene and by decontaminating clothes and bedding by washing at temperatures that kill lice. If infestation severe and a pediculicide necessary, use agents recommended for pediculosis capitis (i.e., topical permethrin or topical pyrethrins with piperonyl butoxide or, alternatively, other topical pediculicides or oral ivermectin).
Scabies
Treatment of scabies† (mite infestation). CDC, AAP, and others usually recommend topical permethrin 5% as scabicide of choice; CDC also recommends oral ivermectin as a drug of choice.
May be particularly useful in refractory scabies infestations, for control of outbreaks in institutions, and when compliance with topical therapy is difficult.
Has been used for treatment of severe or crusted (i.e., Norwegian) scabies†. May be a drug of choice in immunocompromised patients. Aggressive treatment (multiple-dose oral ivermectin regimen with concomitant topical scabicide) usually necessary.
Ivermectin Dosage and Administration
General
Onchocerciasis
-
Does not kill adult O. volvulus worms, but may decrease microfilarial load in skin for approximately 6–12 months following a single dose. Follow-up and retreatment required since adult female worms continue to produce microfilaria for 9–15 years.
-
Recommendations for retreatment intervals vary. For individual patients, retreatment once every 6–12 months until asymptomatic has been recommended; intervals as short as 3 months can be considered. When used in mass treatment and control programs (community-wide mass drug administration [MDA] programs), retreatment often given at 6- or 12-month intervals; some programs use 3-month intervals to suppress microfilarial counts to a level where transmission can be interrupted.
-
Adjunctive surgical excision of subcutaneous nodules may help eliminate microfilariae-producing adult worms, but there is no evidence that nodulectomies reduce blindness associated with onchocerciasis.
Strongyloidiasis
-
After treatment, perform follow-up stool examinations to verify eradication of S. stercoralis; retreatment indicated if recrudescence of larvae observed.
-
Optimal dosage for treatment of intestinal strongyloidiasis in immunocompromised (e.g., HIV-infected) patients not established. Several courses of therapy (i.e., at intervals of 2 weeks) may be necessary; cure may not be achieved. Control of extra-intestinal strongyloidiasis in such patients is difficult; once-monthly suppressive treatment may be helpful.
Pediculosis†
-
To avoid reinfestation or transmission of lice, most experts recommend that clothing, hats, bed linen, and towels worn or used by infested individual during the 2 days prior to treatment be decontaminated (machine-washed in hot water and dried in a hot dryer).
-
Items that cannot be laundered can be dry-cleaned or sealed in a plastic bag for 2 weeks.
-
Decontaminate combs, brushes, and hair clips used by infested individual by soaking in hot water (>54°C) for 5–10 minutes.
-
Thoroughly vacuum car seats, upholstered furniture, and floors of rooms inhabited by infested individual. Fumigation of living areas not necessary.
-
Evaluate other family members and close contacts of infested individual and treat if lice infestation present. Some clinicians suggest treating family members who share a bed with infested individual, even if no live lice found on this family member. Ideally, treat all infested household members and close contacts at same time.
-
A fine-toothed or nit comb may be used to remove any remaining nits (eggs) or nit shells from hair. Some clinicians do not consider nit removal necessary since only live lice can be transmitted, but recommend it for aesthetic reasons and to decrease diagnostic confusion and unnecessary retreatment. Other clinicians recommend removal of nits (especially those within 1 cm of scalp) to decrease risk of reinfestation since no pediculicide is 100% ovicidal and potentially viable nits may remain on hair after treatment. Although many schools will not allow children with nits to attend, AAP and other experts consider these no-nit policies excessive.
Scabies†
-
Consider treating family members of patients with scabies since asymptomatic scabies is common.
-
Skin eruptions at scabies infestation sites may worsen (increased lesion count and inflammation) during first few days after initiation of treatment.
-
Pruritus may persist 2–4 weeks after treatment while dead mites in the outer skin layers slough off with normal exfoliation.
-
HIV-infected patients with uncomplicated scabies should receive same treatment as those without HIV infection.
-
If used for treatment of crusted scabies†, multiple-dose regimen in conjunction with a topical scabicide recommended to reduce risk of treatment failure. Immunocompromised patients, including those with HIV infection, are at increased risk of developing crusted scabies; manage such patients in consultation with an expert.
Administration
Oral Administration
Administer orally. Take tablets on an empty stomach with water.
Dosage
Pending revision, the material in this section should be considered in light of more recently available information in the MedWatch notification at the beginning of this monograph.
Pediatric Patients
Safety and efficacy not established in children weighing <15 kg.
Ascariasis†
Ascaris lumbricoides infections†
OralChildren weighing ≥15 kg: 150–200 mcg/kg as a single dose.
Filariasis
Onchocerciasis (Filariasis Caused by Onchocerca volvulus)
OralChildren weighing ≥15 kg: Approximately 150 mcg/kg as a single dose.
For individual patients, retreat once every 6–12 months until asymptomatic; can consider intervals as short as 3 months.
In international mass treatment and control programs (MDA programs), typically administered at 6- or 12-month intervals. Some (e.g., in hyperendemic areas) use 3-month intervals.
|
Patient Weight (kg) |
Single Oral Dose |
|---|---|
|
15–25 |
3 mg |
|
26–44 |
6 mg |
|
45–64 |
9 mg |
|
65–84 |
12 mg |
|
≥85 |
150 mcg/kg |
Alternatively, in MDA programs, dosage is estimated based on height† since weighing recipients may be impractical (e.g., in rural areas of developing countries).
|
Patient Height (cm) |
Single Oral Dose |
|---|---|
|
90–119 |
3 mg |
|
120–140 |
6 mg |
|
141–158 |
9 mg |
|
≥159 |
12 mg |
Mansonella streptocerca Infections†
OralChildren weighing ≥15 kg: 150 mcg/kg as a single dose.
Wuchereria bancrofti Infections†
Oral150–400 mcg/kg as a single dose has been used; often used in conjunction with a single dose of albendazole or diethylcarbamazine (available in US from CDC).
Gnathostomiasis†
Gnathostoma spinigerum Infections†
OralChildren weighing ≥15 kg: 200 mcg/kg once daily for 2 days.
Hookworm Infections†
Cutaneous Larva Migrans (Creeping Eruption Caused by Dog and Cat Hookworms)†
OralChildren weighing ≥15 kg: 200 mcg/kg once daily for 1–2 days.
Strongyloidiasis
Treatment of Intestinal Strongyloides stercoralis Infections
OralChildren weighing ≥15 kg: Approximately 200 mcg/kg as a single dose. Alternatively, some clinicians recommend 200 mcg/kg once daily for 2 days.
Manufacturer states additional doses not generally necessary, but follow-up stool examinations required to verify eradication. Retreat if recrudescence of larvae observed.
|
Patient Weight (kg) |
Single Oral Dose |
|---|---|
|
15–24 |
3 mg |
|
25–35 |
6 mg |
|
36–50 |
9 mg |
|
51–65 |
12 mg |
|
66–79 |
15 mg |
|
≥80 |
200 mcg/kg |
Prevention of Strongyloides Hyperinfection in HSCT Candidates at Risk†
OralChildren weighing ≥15 kg: 200 mcg/kg once daily for 2 days; repeat after 2 weeks. Complete regimen prior to HSCT.
In immunocompromised candidates, multiple courses at 2-week intervals may be required and cure may not be achievable.
Trichuriasis†
Trichuris trichiura Infections†
OralChildren weighing ≥15 kg: 200 mcg/kg once daily for 3 days.
Pediculosis†
Pediculosis Capitis (Head Lice Infestation)†
OralChildren weighing ≥15 kg: 200 or 400 mcg/kg . Although >1 dose usually necessary, optimal number of doses and dosing interval not established.
A 2-dose regimen of 200- or 400-mcg/kg doses given 7–10 days apart has been used.
Pediculosis Pubis (Pubic Lice Infestation)†
OralA 2-dose regimen of 250-mcg/kg doses given 2 weeks apart recommended by CDC.
Scabies†
Oral
Children weighing ≥15 kg: A 2-dose regimen of 200-mcg/kg doses given 2 weeks apart recommended by CDC.
Others recommend 2-dose regimen of 200-mcg/kg doses given ≥7 days apart.
Optimal number of doses not determined; 2 doses usually recommended, especially in immunocompromised patients.
Crusted (Norwegian) Scabies†
OralChildren weighing ≥15 kg: Multiple-dose regimen consisting of 200-mcg/kg doses. CDC and others recommend doses be given once daily on days 1, 2, 8, 9, and 15; severe cases may also require doses on days 22 and 29.
Usually used in conjunction with a topical scabicide (e.g., topical benzyl benzoate 5%, topical permethrin 5%).
Adults
Ascariasis†
Ascaris lumbricoides Infections†
Oral150–200 mcg/kg as a single dose.
Filariasis
Onchocerciasis (Filariasis Caused by Onchocerca volvulus)
OralApproximately 150 mcg/kg as a single dose.
For individual patients, retreat once every 6–12 months until asymptomatic; can consider intervals as short as 3 months.
|
Patient Weight (kg) |
Single Oral Dose |
|---|---|
|
15–25 |
3 mg |
|
26–44 |
6 mg |
|
45–64 |
9 mg |
|
65–84 |
12 mg |
|
≥85 |
150 mcg/kg |
Alternatively, in some mass treatment and control programs, dosage is estimated based on height†; weighing recipients may be impractical (e.g., in rural areas of developing countries).
|
Patient Height (cm) |
Single Oral Dose |
|---|---|
|
90–119 |
3 mg |
|
120–140 |
6 mg |
|
141–158 |
9 mg |
|
≥159 |
12 mg |
Mansonella Infections†
OralFilariasis caused by M. streptocerca†: 150 mcg/kg as a single dose.
Filariasis caused by M. ozzardi†: 200 mcg/kg as a single dose has been used.
Wuchereria bancrofti Infections†
Oral150–400 mcg/kg as a single dose has been used; often used in conjunction with a single dose of albendazole or diethylcarbamazine (available in US from CDC).
Gnathostomiasis†
Gnathostoma spinigerum Infections†
Oral200 mcg/kg once daily for 2 days.
Hookworm Infections†
Cutaneous Larva Migrans (Creeping Eruption Caused by Dog and Cat Hookworms)†
Oral200 mcg/kg once daily for 1–2 days.
Strongyloidiasis
Treatment of Intestinal Strongyloides stercoralis Infections
OralApproximately 200 mcg/kg as a single dose. Alternatively, some clinicians recommend 200 mcg/kg once daily for 2 days.
Manufacturer states additional doses not generally necessary, but follow-up stool examinations required to verify eradication. Retreat if recrudescence of larvae observed.
|
Patient Weight (kg) |
Single Oral Dose |
|---|---|
|
15–24 |
3 mg |
|
25–35 |
6 mg |
|
36–50 |
9 mg |
|
51–65 |
12 mg |
|
66–79 |
15 mg |
|
≥80 |
200 mcg/kg |
Prevention of Strongyloides Hyperinfection in HSCT Candidates at Risk†
Oral200 mcg/kg once daily for 2 days; repeat after 2 weeks. Complete regimen prior to HSCT.
In immunocompromised candidates, multiple courses at 2-week intervals may be required and cure may not be achievable.
Trichuriasis†
Trichuris trichiura Infections†
Oral200 mcg/kg once daily for 3 days.
Pediculosis†
Pediculosis Capitis (Head Lice Infestation)†
Oral200 or 400 mcg/kg. Although >1 dose usually necessary, optimal number of doses and dosing interval not established.
A 2-dose regimen of 200- or 400-mcg/kg doses given 7–10 days apart has been used.
Pediculosis Pubis (Pubic Lice Infestation)†
OralA 2-dose regimen of 250-mcg/kg doses given 2 weeks apart recommended by CDC.
Scabies†
Oral
A 2-dose regimen of 200-mcg/kg doses given 2 weeks apart recommended by CDC.
Others recommend 2-dose regimen of 200-mcg/kg doses given ≥7 days apart.
Optimal number of doses not determined; 2 doses usually recommended, especially in immunocompromised patients.
Crusted (Norwegian) Scabies†
OralMultiple-dose regimen consisting of 200-mcg/kg doses. CDC and others recommend doses be given once daily on days 1, 2, 8, 9, and 15; severe cases may also require doses on days 22 and 29.
Use in conjunction with a topical scabicide (e.g., topical benzyl benzoate 5%, topical permethrin 5%).
Cautions for Ivermectin
Contraindications
Pending revision, the material in this section should be considered in light of more recently available information in the MedWatch notification at the beginning of this monograph.
-
Hypersensitivity to ivermectin or any ingredient in the formulation.
Warnings/Precautions
Warnings
Mazzotti Reactions
Cutaneous and/or systemic reactions of varying severity (Mazzotti reactions) may occur in patients with onchocerciasis receiving microfilaricidal drugs (e.g., diethylcarbamazine, ivermectin). These may be secondary to allergic and inflammatory responses to death of microfilariae.
Mazzotti reactions may include pruritus, edema, frank urticarial rash (papular and pustular), fever, arthralgia/synovitis, and lymph node enlargement/tenderness (e.g., axillary, cervical, inguinal).
Mazzotti-type reactions appear to be less severe and occur less frequently with ivermectin than with diethylcarbamazine.
These reactions may be most severe in previously untreated patients and may diminish with subsequent treatment (e.g., annual mass treatment and control programs).
Optimal treatment of severe Mazzotti reactions not determined. Oral or IV hydration, recumbency, and/or parenteral corticosteroids have been used to treat postural hypotension; for supportive treatment of mild to moderate reactions, antihistamines, corticosteroids, and/or aspirin have been used.
Mazzotti-type reactions observed with treatment of onchocerciasis or the disease itself would not be anticipated in patients being treated for strongyloidiasis.
Ocular Effects
Ocular reactions (e.g., abnormal sensation in the eyes, eyelid edema, anterior uveitis, conjunctivitis, limbitis, keratitis, chorioretinitis or choroiditis) may occur in patients being treated for onchocerciasis or may occur secondary to the disease itself.
Ocular reactions observed with treatment of onchocerciasis or the disease itself would not be anticipated in patients being treated for strongyloidiasis.
Neurotoxicity
Not recommended in patients with an impaired blood-brain barrier (e.g., meningitis, African trypanosomiasis) or CNS disorders that may increase CNS penetration of the drug; potential interaction with CNS GABA receptors. (See Interactions.)
P-glycoprotein, encoded by the multi-drug resistance gene (MDR1), functions as a drug efflux transporter; appears to limit CNS uptake and prevent potentially fatal neurotoxicity.
Theoretical increased risk of neurotoxicity in patients with altered expression or function of P-glycoprotein (e.g. through genetic polymorphism, concomitant use of inhibitors of the P-glycoprotein transport system); if such increased susceptibility exists, apparently rare. (See Interactions.)
Although not reported in humans to date, neurotoxicity (e.g., tremors, ataxia, sweating, lethargy, coma, death) has occurred in certain animals with extreme sensitivity (e.g., collie dogs, inbred strains of mice); increased CNS sensitivity appears to be secondary to absent or dysfunctional MDR and P-glycoprotein.
General Precautions
Encephalopathy Risk in Onchocerciasis and Loiasis
Consider possible severe adverse effects when treating onchocerciasis in patients from areas where onchocerciasis and loiasis are co-endemic.
Patients with onchocerciasis who also are heavily infected with L. loa may develop serious or fatal neurologic events (e.g., encephalopathy, coma) either spontaneously or following rapid killing of microfilariae with effective microfilaricidal agents, including ivermectin.
Back pain, conjunctival hemorrhage, dyspnea, urinary and/or fecal incontinence, difficulty standing or walking, mental status changes, confusion, lethargy, stupor, seizures, coma, dysarthria or aphasia, fever, headache, or chills also reported.
Reported rarely in patients receiving ivermectin, but a definite causal relationship not established.
Pretreatment assessment for loiasis and careful post-treatment follow-up recommended when treatment is planned for any reason in patients with significant exposure to L. loa in endemic areas (West or Central Africa).
Other Precautions in Filariasis
Increased risk of severe adverse reactions (e.g., edema, aggravation of onchodermatitis) in patients with hyperreactive onchodermatitis (sowdah).
Does not kill adult O. volvulus worms, but decreases microfilarial load in skin for approximately 6–12 months following a single dose. Follow-up and retreatment required since the adult female worms continue to produce microfilaria for 9–15 years.
Specific Populations
Pregnancy
Category C.
Has been inadvertently given to pregnant women during mass distribution campaigns for treatment and control of onchocerciasis or lymphatic filariasis, but was not associated with adverse pregnancy outcomes, congenital malformations, or differences in developmental status or disease patterns in the offspring of such women.
World Health Organization (WHO) and other experts state that use for treatment of onchocerciasis after the first trimester probably is acceptable based on the high risk of infection-associated blindness if untreated.
Lactation
Distributed into milk. Use in nursing women only when risk of delayed treatment in the woman outweighs risks to the nursing infant.
Pediatric Use
Safety and efficacy not established in children weighing <15 kg.
Some clinicians state that use not recommended in young children (e.g., those weighing <15 kg or <2 years of age) partly because the blood-brain barrier may be less developed than in older patients. (See Neurotoxicity under Cautions.)
Limited data suggest that safety in those 6–13 years of age similar to that in adults.
Geriatric Use
Insufficient experience in controlled clinical studies in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults. Other clinical experience has not revealed age-related differences in response.
Use with caution due to greater frequency of decreased hepatic, renal, and/or cardiac function and of concomitant disease and drug therapy observed in the elderly.
Common Adverse Effects
Treatment of onchocerciasis: Worsening of Mazzotti reactions (see Mazzotti Reactions under Cautions), ocular effects, peripheral edema, tachycardia, eosinophilia.
Treatment of strongyloidiasis: GI effects (diarrhea, nausea, anorexia, constipation, vomiting, abdominal pain, abdominal distention), decreased leukocyte count, eosinophilia, increased hemoglobin, increased serum ALT or AST, nervous system effects (dizziness, asthenia or fatigue, somnolence, tremor, vertigo), pruritus, rash, urticaria.
Drug Interactions
Appears to be metabolized principally by CYP3A4 and, to lesser extent, by 2D6 and 2E1. Does not inhibit CYP3A4, 2D6, 2C9, 1A2, and 2E1.
Drugs with GABA-potentiating Activity
Concomitant use with drugs with GABA-potentiating activity (e.g., barbiturates, benzodiazepines, sodium oxybate, valproic acid) not recommended. Ivermectin may interact with GABA receptors in the CNS.
Drugs Affecting or Affected by P-glycoprotein Transport
Appears to be a substrate of P-glycoprotein transport system. Theoretical possibility of interactions with inducers (e.g., amprenavir, clotrimazole, phenothiazines, rifampin, ritonavir, St. John’s wort) or inhibitors (e.g., amiodarone, carvedilol, clarithromycin, cyclosporine, erythromycin, itraconazole, ketoconazole, quinidine, ritonavir, tamoxifen, verapamil) of this system. Concomitant use with inhibitors theoretically could result in increased brain concentrations of ivermectin and neurotoxicity
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
Increased plasma ivermectin concentrations |
Clinical importance unknown |
|
Anticoagulants |
Postmarketing reports of elevated INR when used concomitantly with warfarin |
|
|
Benzodiazepines |
Benzodiazepine effects may be potentiated |
Concomitant use not recommended |
Ivermectin Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed following oral administration; peak plasma concentrations attained in about 4 hours.
Food
High-fat meal may increase absorption, but effect of food on bioavailability not evaluated using usual dosage (150–200 mcg/kg).
Distribution
Extent
Concentrated in liver and adipose tissue.
Does not readily cross blood-brain barrier. Brain uptake apparently limited by P-glycoprotein transport system. (See Neurotoxicity under Cautions.)
Distributed into milk in low concentrations.
Plasma Protein Binding
Approximately 93%; principally albumin and, to a lesser extent, α 1-acid glycoprotein.
Elimination
Metabolism
Metabolized in the liver, principally by CYP3A4.
Appears to be a substrate of the P-glycoprotein transport system.
Elimination Route
Excreted almost exclusively in feces (within approximately 12 days); <1% excreted in urine.
Half-life
Approximately 18 hours following oral administration.
Stability
Storage
Oral
Tablets
≤30°C.
Actions and Spectrum
-
An avermectin-derivative anthelmintic, pediculicide, and scabicide; a macrocyclic lactone similar to macrolide antibacterials but possesses no antibacterial properties.
-
In susceptible nematodes (roundworms), ivermectin affects ion channels in cell membranes.
-
Binds selectively and with high affinity to glutamate-gated chloride ion channels in nerve and muscle cells of invertebrates, leading to increased cell membrane permeability to chloride ions; cellular hyperpolarization ensues, followed by paralysis and death.
-
Also appears to interact with other ligand-gated chloride channels, such as those gated by GABA.
-
In susceptible parasites, may interfere with the GI function resulting in starvation of the parasite.
-
Nematodes (roundworms): Active against tissue microfilariae of Onchocerca volvulus; intestinal stages of Strongyloides stercoralis (threadworm); microfilariae of Acylostoma braziliense, A. caninum, Brugia malayi, Gnathostoma spinigerum, Loa loa, Mansonella streptocerca, M. ozzardi, and Wuchereria bancrofti; and intestinal stages of Ascaris lumbricoides and Enterobius vermicularis.
-
Activity against Trichuris trichiura reported to be less than that against other nematodes. Has little or no activity against Ancylostoma duodenale, Mansonella perstans, Necator americanus, Toxocara canis, and T. catis.
-
Ectoparasites: Active against adult lice, including Pediculus humanus var capitis (head louse) and Phthirus pubis (pubic or crab louse). Also active against the mite Sarcoptes scabiei. May have some activity against Demodex mites.
-
Resistance reported in some nematodes obtained from livestock after extensive exposure to ivermectin; similar resistance not reported to date in nematodes obtained from humans.
-
Although further study is needed, some data obtained from individuals in Ghana who received ivermectin in mass treatment programs of onchocerciasis (communities had received 6–18 rounds of treatment) suggest that ivermectin resistance in O. volvulus may be developing in some communities and is manifested as a more rapid return to high microfilarial load in the skin after treatment.
-
S. scabiei with reduced ivermectin susceptibility obtained from a few patients who received multiple doses (≥30 doses) for recurrent scabies episodes; may represent inadequate dosage rather than actual resistance.
Advice to Patients
Pending revision, the material in this section should be considered in light of more recently available information in the MedWatch notification at the beginning of this monograph.
-
Importance of taking on an empty stomach with water.
-
Advise patients treated for onchocerciasis that the drug does not kill adult Onchocerca worms and that follow-up and retreatment usually is required.
-
Advise patients treated for strongyloidiasis of the need for repeated stool examinations to document clearance of S. stercoralis infection.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal products (e.g., St. John’s wort), and any concomitant or past illnesses (e.g., meningitis, African trypanosomiasis, CNS disorders).
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
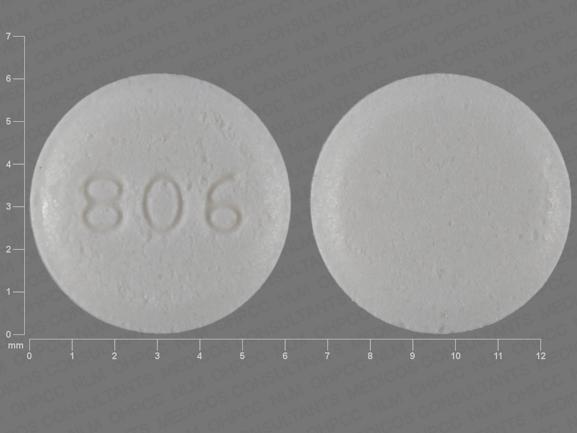
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
3 mg |
Stromectol |
Merck |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
- Can Ivermectin be used to treat COVID-19?
- How long does it take for ivermectin to kill head lice?
- How long does it take for Sklice (ivermectin) to kill head lice?
More about ivermectin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (49)
- Drug images
- Latest FDA alerts (1)
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: anthelmintics
- Breastfeeding
- En español