Aspirin (Monograph)
Brand names: Ascriptin, Aspergum, Bayer, Bufferin, Easprin,
... show all 11 brands
Drug class: Salicylates
- Antithrombotic Agents
- Platelet-aggregation Inhibitors
VA class: CN103
CAS number: 50-78-2
Aspirin is also contained as an ingredient in the following combinations:
Acetaminophen and Aspirin
Acetaminophen, Aspirin, and Caffeine
Oxycodone and Aspirin
Pentazocine Hydrochloride and Aspirin
Propoxyphene Hydrochloride, Aspirin, and Caffeine
Introduction
NSAIA; salicylate ester of acetic acid.
Uses for Aspirin
Pain
Symptomatic relief of mild to moderate pain.
Self-medication in children for the temporary relief of minor aches and pains and headache.
Self-medication in adolescents and adults for the temporary relief of minor aches and pains associated with headache, common cold, toothache, muscular aches, backache, arthritis, menstrual cramps, and sore throat.
Self-medication in fixed combination with acetaminophen and caffeine for the temporary relief of mild to moderate pain associated with migraine headache; also can be used for the treatment of severe migraine headache if previous attacks have responded to similar non-opiate analgesics or NSAIAs.
Fever
Self-medication for reduction of fever associated with colds, sore throats, and teething. (See Contraindications and see Pediatric Use under Cautions.)
Inflammatory Diseases
Symptomatic treatment of rheumatoid arthritis, juvenile rheumatoid arthritis, osteoarthritis, spondyloarthropathies, and systemic lupus erythematosus (SLE).
Rheumatic Fever
Symptomatic treatment of rheumatic fever† [off-label]. A drug of choice in patients with mild carditis (without cardiomegaly or CHF, with or without polyarthritis) or with polyarthritis only.
Transient Ischemic Attacks and Ischemic Stroke
Reduction of the risk of recurrent TIAs or stroke or of death in patients with a history of TIAs or ischemic stroke (secondary prevention).
Also used in fixed combination with extended-release dipyridamole to reduce the risk of recurrent stroke, death from all vascular causes, or nonfatal MI in patients who have had TIAs or completed ischemic stroke caused by thrombosis.
The American College of Chest Physicians (ACCP), the American Stroke Association (ASA), and AHA consider aspirin or the combination of aspirin and extended-release dipyridamole acceptable antiplatelet regimens for secondary prevention of noncardioembolic ischemic stroke and TIAs; other options include cilostazol or clopidogrel. When selecting an appropriate antiplatelet regimen, consider factors such as the patient's individual risk for recurrent stroke, tolerance, and cost of the different agents.
Oral anticoagulation (e.g., dabigatran, warfarin) rather than antiplatelet therapy is recommended in patients with a history of ischemic stroke or TIA and concurrent atrial fibrillation; however, in patients who cannot take or choose not to take oral anticoagulants (e.g., those with difficulty maintaining stable INRs, compliance issues, dietary restrictions, or cost limitations), dual antiplatelet therapy with aspirin and clopidogrel is recommended.
Also used for acute treatment of ischemic stroke in children† [off-label].
Coronary Artery Disease
Recommended by AHA and the American College of Cardiology Foundation (ACCF) for reduction of the risk of vascular events (e.g., stroke, recurrent MI) in all patients with CAD, unless contraindicated.
Recommended by American Diabetes Association (ADA) for secondary prevention of cardiovascular events in patients with diabetes mellitus and a history of atherosclerotic cardiovascular disease (ASCVD).
ST-Segment-Elevation MI (STEMI)
Reduction of the risk of stroke, recurrent infarction, and death in patients with STEMI.
Use in conjunction with a P2Y12 platelet adenosine diphosphate (ADP)-receptor antagonist (e.g., clopidogrel, prasugrel, ticagrelor).
The addition of warfarin to antiplatelet therapy is recommended in patients with STEMI who have indications for anticoagulation (e.g., atrial fibrillation, left ventricular dysfunction, cerebral emboli, extensive wall-motion abnormality, mechanical heart valves).
Primary Prevention of Ischemic Cardiac Events
Use of aspirin for primary prevention of cardiovascular disease remains controversial; may reduce the risk of a first cardiac event (e.g., STEMI)† [off-label] in certain patient populations (primary prevention). Balance of risks and benefits is most favorable in patients at higher ASCVD risk who have a low risk of bleeding.
Some experts recommend reserving low-dose aspirin for primary prevention in adults 40–70 years of age who have a higher risk of cardiovascular disease without an increased risk of bleeding (e.g., history of previous GI bleed, peptic ulcer disease, thrombocytopenia, coagulopathy, chronic kidney disease, concomitant use of drugs that increase bleeding risk [e.g., NSAIAs, corticosteroids, direct oral anticoagulants, warfarin]).
Consider totality of patient risk factors when determining risk for ASCVD, (e.g., strong family history of premature MI; inability to achieve lipid, BP, or blood glucose targets; substantial elevation in coronary artery calcium score) in conjunction with patient and clinician preferences. High-risk patients also include adults 40–70 years of age without diabetes mellitus who have a 10-year ASCVD risk ≥20% and those with diabetes mellitus who have a 10-year ASCVD risk ≥10%.
The US Preventive Services Task Force (USPSTF) states that the beneficial effects of aspirin for primary prevention of cardiovascular disease are modest and occur at daily dosages of ≤100 mg, with a potentially greater relative benefit for MI prevention in older adults.
ADA states may be considered for primary prevention in patients with type 1 or type 2 diabetes mellitus who are at high risk for cardiovascular events (i.e., familial history of premature ASCVD, smoking, hypertension, chronic kidney disease/albuminuria, elevated blood cholesterol or triglyceride concentrations) after evaluating risks versus benefits.
Not currently recommended for primary prevention in patients with a low risk of ASCVD. Not routinely recommended for primary prevention in individuals <40 or >70 years of age.
Non-ST-Segment-Elevation Acute Coronary Syndromes (NSTE ACS)
Reduction of the risk of death and/or nonfatal MI in patients with NSTE ACS (unstable angina or non-ST-segment-elevation MI [NSTEMI]).
Dual-drug antiplatelet therapy with aspirin and a P2Y12-receptor antagonist (e.g., clopidogrel, ticagrelor) is considered part of the current standard of care for treatment and secondary prevention in patients with NSTE ACS.
Experts state that aspirin should be administered as soon as possible after presentation (and continued indefinitely) in all patients with NSTE ACS unless contraindicated; in addition, a P2Y12-receptor antagonist should be administered for up to 12 months.
Chronic Stable Angina
Reduction of the risk of MI and/or sudden death in patients with chronic stable angina.
Experts recommend that aspirin therapy (75–162 mg daily) be continued indefinitely in patients with stable ischemic heart disease who do not have contraindications.
Percutaneous Coronary Intervention and Revascularization Procedures
Reduction of cardiovascular risks (e.g., early ischemic complications, graft closure) in patients with ACS undergoing PCI (e.g., coronary angioplasty, coronary artery stent implantation) or CABG.
Pretreatment with aspirin prior to PCI recommended by ACCF, AHA, and the Society for Cardiovascular Angiography and Interventions (SCAI). Adjunctive therapy with a P2Y12-receptor antagonist (e.g., clopidogrel, prasugrel, ticagrelor) also recommended in patients undergoing PCI with stent placement.
Continue low-dose aspirin therapy indefinitely (as part of dual-drug antiplatelet therapy with a P2Y12-receptor antagonist for at least 12 months and possibly longer) as secondary prevention against cardiovascular events, including stent thrombosis, following PCI.
Embolism Associated with Atrial Fibrillation
Used as an alternative or adjunct to warfarin therapy for reduction of the incidence of thromboembolism in selected patients with chronic atrial fibrillation† [off-label].
ACCP, ASA, ACC, AHA, and other experts currently recommend that antithrombotic therapy be given to all patients with nonvalvular atrial fibrillation (i.e., atrial fibrillation in the absence of rheumatic mitral stenosis, a prosthetic heart valve, or mitral valve repair) who are considered to be at increased risk of stroke, unless such therapy is contraindicated.
Choice of antithrombotic therapy is based on patient's risk for stroke and bleeding. In general, oral anticoagulant therapy (traditionally warfarin) is recommended in patients with high risk for stroke and acceptably low risk of bleeding, while aspirin or no antithrombotic therapy may be considered in patients at low risk of stroke.
In patients with atrial fibrillation at increased risk of stroke who cannot take or choose not to take oral anticoagulants for reasons other than concerns about major bleeding (e.g., those with difficulty maintaining stable INRs), combination therapy with clopidogrel and aspirin rather than aspirin alone is recommended.
Antithrombotic therapy in patients with atrial flutter generally managed in the same manner as in patients with atrial fibrillation.
Peripheral Arterial Disease
Has been used for primary and secondary prophylaxis of cardiovascular events in patients with peripheral arterial disease, including those with intermittent claudication or carotid stenosis and those undergoing revascularization procedures (peripheral artery percutaneous transluminal angioplasty or peripheral arterial bypass graft surgery).
ACCP suggests the use of low-dose aspirin for primary prevention in patients with asymptomatic peripheral arterial disease.
For patients with symptomatic peripheral arterial disease or those undergoing revascularization procedures, single-drug antiplatelet therapy with aspirin or clopidogrel generally is recommended.
Valvular Heart Disease
Recommended by ACC and AHA for use in selected patients with mitral valve prolapse and atrial fibrillation, and also in symptomatic patients with mitral valve prolapse who experience TIAs.
Prosthetic Heart Valves
Used for the prevention of thromboembolism in selected patients with prosthetic heart valves† [off-label].
ACCP and ACC/AHA suggest the use of low-dose aspirin for initial (i.e., first 3 months after valve insertion) and long-term antithrombotic therapy in patients with a bioprosthetic heart valve in the aortic position who are in sinus rhythm and have no other indications for warfarin. Aspirin also may be considered after initial (3 months) warfarin therapy in patients with a bioprosthetic heart valve in the mitral position who are in sinus rhythm.
Addition of an antiplatelet agent such as low-dose aspirin to warfarin therapy recommended in all patients with mechanical heart valves who are at low risk of bleeding. Combination therapy with aspirin and warfarin also recommended in patients with bioprosthetic heart valves who have additional risk factors for thrombosis (e.g., atrial fibrillation, previous thromboembolism, left ventricular dysfunction, hypercoagulable condition).
May be added to therapy with a low molecular weight heparin (LMWH) or heparin (referring throughout this monograph to unfractionated heparin) in pregnant women with prosthetic heart valves† who are at high risk for thrombosis.
Thrombosis Associated with Fontan Procedure in Children
Has been used for prevention of thromboembolic complications following Fontan procedure† (definitive palliative surgical treatment for most congenital univentricular heart lesions) in children.
Thromboprophylaxis in Orthopedic Surgery
Has been used for the prevention of venous thromboembolism in patients undergoing major orthopedic surgery (total-hip replacement, total-knee replacement, or hip-fracture surgery†). Aspirin generally not considered the drug of choice for this use; however, some evidence suggests some benefit over placebo or no antithrombotic prophylaxis in patients undergoing major orthopedic surgery.
ACCP considers aspirin an acceptable option for pharmacologic thromboprophylaxis in patients undergoing major orthopedic surgery.
When selecting an appropriate thromboprophylaxis regimen, consider factors such as relative efficacy and bleeding risk in addition to other logistics and compliance issues.
Thromboprophylaxis in General Surgery
Has been used for thromboprophylaxis in patients undergoing general (e.g., abdominal) surgery who are at high risk of venous thromboembolism; however, generally recommended as an alternative to LMWHs and low-dose heparin.
Pericarditis
Drug of choice for the management of pain associated with acute pericarditis† following MI.
Kawasaki Disease
Treatment of Kawasaki disease; used in conjunction with immune globulin IV (IGIV).
Complications of Pregnancy
Has been used alone or in combination with other drugs (e.g., heparin, corticosteroids, immune globulin) for prevention of complications of pregnancy† (e.g., preeclampsia, pregnancy loss in women with a history of antiphospholipid syndrome and recurrent fetal loss).
Low-dose aspirin in combination with sub-Q heparin or an LMWH is recommended by ACCP in women with antiphospholipid antibody (APLA) syndrome† and a history of multiple (≥3) pregnancy losses.
Routine use of aspirin prophylaxis to reduce the incidence and severity of preeclampsia (even in patients at increased risk of preeclampsia) generally not recommended; can consider prophylaxis in women with prior severe or early-onset preeclampsia, chronic hypertension, severe diabetes, or moderate to severe renal disease. In women at high risk for preeclampsia, ACCP recommends low-dose aspirin during pregnancy, starting from the second trimester. (See Pregnancy under Cautions.)
Prevention of Cancer
Limited data (observational studies) suggest that aspirin or other NSAIAs may reduce the risk of various cancers† (e.g., colorectal, breast, gastric cancer); such results generally not confirmed in randomized controlled trials.
Regular use (e.g., daily) associated with a reduction in the risk of recurrent colorectal adenomas and colorectal cancer† in some studies. Beneficial effects of NSAIAs in reducing colorectal cancer risk dissipate following discontinuance of such therapy. Preventive therapy with aspirin currently not recommended because aspirin does not completely eliminate adenomas; aspirin therapy should not be considered a replacement for colorectal cancer screening and surveillance.
Related/similar drugs
Benlysta, Cimzia, Saphnelo, amlodipine, gabapentin, acetaminophen, prednisone
Aspirin Dosage and Administration
Administration
Administer orally; may administer rectally as suppositories in patients who cannot tolerate oral therapy.
Do not use aspirin preparation if strong vinegar-like odor is present.
Oral Administration
Usually administer orally with food or a full glass of water (240 mL).
Film-coated, extended-release, or enteric-coated may be associated with less GI irritation and/or symptomatic GI disturbances than uncoated tablets.
Do not use delayed-release or extended-release tablets if rapid response is required.
Swallow delayed-release and extended-release tablets whole; do not crush or chew.
Prepare oral solution by dissolving 2 tablets for solution (Alka-Seltzer) in 120 mL of water; ingest the entire solution to ensure adequate dosing.
Do not chew aspirin preparations for ≥7 days following tonsillectomy or oral surgery; do not place preparations directly on tooth or gum surface (possible tissue injury from prolonged contact).
Rectal Administration
Do not administer aspirin tablets rectally.
Dosage
When used for pain, fever, or inflammatory diseases, attempt to titrate to the lowest effective dosage.
When used in anti-inflammatory dosages, development of tinnitus can be used as a sign of elevated plasma salicylate concentrations (except in patients with high-frequency hearing impairment).
Pediatric Patients
Dosage in children should be guided by body weight or body surface area.
Do not use in children and teenagers with varicella or influenza, unless directed by a clinician. (See Contraindications under Cautions.)
Pain
Oral
Children 2–11 years of age: 1.5 g/m2 daily administered in 4–6 divided doses (maximum 2.5 g/m2 daily).
Dose may be given every 4 hours as necessary (up to 5 times in 24 hours).
|
Age |
Weight |
Oral Dose |
|---|---|---|
|
<3 years of age |
<14.5 kg |
Consult clinician |
|
3–<4 years |
14.5–16 kg |
160 mg |
|
4–<6 years |
16–20.5 kg |
240 mg |
|
6–<9 years |
20.5–30 kg |
320 mg |
|
9–<11 years |
30–35 kg |
320–400 mg |
|
11 years |
35–38 kg |
320–480 mg |
For self-medication in children ≥12 years of age, 325–650 mg every 4 hours (maximum 4 g daily) or 1 g every 6 hours as necessary.
For self-medication in children ≥12 years of age, 454 mg (as chewing gum pieces) every 4 hours as necessary (maximum 3.632 g daily).
For self-medication in children ≥12 years of age, 650 mg (as highly buffered effervescent solution [Alka-Seltzer Original]) every 4 hours (maximum 2.6 g daily); alternatively, 1 g (Alka-Seltzer Extra Strength) every 6 hours (maximum 3.5 g daily).
Rectal
Children 2–11 years of age: 1.5 g/m2 daily administered in 4–6 divided doses (maximum 2.5 g/m2 daily).
Children ≥12 years of age: 325–650 mg every 4 hours as necessary (maximum 4 g daily).
Fever
Oral
Children 2–11 years of age: 1.5 g/m2 daily administered in 4–6 divided doses (maximum 2.5 g/m2 daily).
Dose may be given every 4 hours as necessary (up to 5 times in 24 hours).
|
Age |
Weight |
Oral Dose |
|---|---|---|
|
<3 years of age |
<14.5 kg |
Consult physician |
|
3–<4 years |
14.5–16 kg |
160 mg |
|
4–<6 years |
16–20.5 kg |
240 mg |
|
6–<9 years |
20.5–30 kg |
320 mg |
|
9–<11 years |
30–35 kg |
320–400 mg |
|
11 years |
35–38 kg |
320–480 mg |
Children ≥12 years of age: 325–650 mg every 4 hours as necessary (maximum 4 g daily).
For self-medication in children ≥12 years of age, 454 mg (as chewing gum pieces) every 4 hours as necessary (maximum 3.632 g daily).
Rectal
Children 2–11 years of age: 1.5 g/m2 daily administered in 4–6 divided doses (maximum 2.5 g/m2 daily).
Children ≥12 years of age: 325–650 mg every 4 hours as necessary (maximum 4 g daily).
Inflammatory Diseases
Juvenile Rheumatoid Arthritis
OralInitially, 90–130 mg/kg daily in divided doses. Increase dosage as necessary for anti-inflammatory efficacy; target plasma salicylate concentration is 150–300 mcg/mL. Plasma concentrations >200 mcg/mL associated with an increased incidence of toxicity.
Rheumatic Fever†
Oral
Initially, 90–130 mg/kg daily given in divided doses every 4–6 hours for up to 1–2 weeks for maximal suppression of acute inflammation, followed by 60–70 mg/kg daily in divided doses for 1–6 weeks. Adjust dosage based on response, tolerance, and plasma salicylate concentrations. Gradually withdraw over 1–2 weeks.
Various regimens suggested depending on severity of initial manifestations. Consult published protocols for more information on specific dosages and schedules.
Thrombosis
Acute Arterial Ischemic Stroke†
OralACCP recommends 1–5 mg/kg daily initially until cerebral arterial dissection and cardioembolic causes have been excluded; subsequently, continue same dosage for ≥2 years.
In children with acute arterial ischemic stroke secondary to non-Moyamoya vasculopathy, at least 3 months of therapy recommended; ongoing antithrombotic therapy should be guided by repeat cerebrovascular imaging.
Fontan Procedure†
Oral1–5 mg/kg daily recommended by ACCP; optimal duration of therapy unknown.
Prosthetic Heart Valves (Mechanical or Biological)†
OralACCP recommends that clinicians follow same recommendations as in adults.
Kawasaki Disease
Oral
Initially, 80–100 mg/kg daily given in 4 equally divided doses (in combination with IGIV) for up to 14 days; initiate within 10 days of onset of fever. When fever subsides, decrease dosage to 1–5 mg/kg once daily.
Continue indefinitely in those with coronary artery abnormalities; in the absence of such abnormalities, continue low-dose aspirin for 6–8 weeks.
Adults
Pain
Oral
For self-medication, 325–650 mg every 4 hours (maximum 4 g daily) or 0.5–1 g every 6 hours as necessary.
For self-medication, 454 mg (as chewing gum pieces) every 4 hours as necessary (maximum 3.632 g daily).
Adults <60 years of age for self-medication: 650 mg (as a highly buffered effervescent solution [Alka-Seltzer Lemon-Lime or Original]) every 4 hours (maximum 2.6 g daily); alternatively, 1 g (Alka-Seltzer Extra Strength) every 6 hours (maximum 3.5 g daily).
Adults ≥60 years of age for self-medication: 650 mg (as a highly buffered effervescent solution [Alka-Seltzer Lemon-Lime or Original]) every 4 hours (maximum 1.3 g daily); alternatively, 1 g (Alka-Seltzer Extra Strength) every 6 hours (maximum 1.5 g daily).
Rectal
325–650 mg every 4 hours as necessary (maximum 4 g daily).
Pain Associated with Migraine Headache
OralFor self-medication, 500 mg (combined with acetaminophen 500 mg and caffeine 130 mg) as a single dose.
Fever
Oral
325–650 mg every 4 hours as necessary (maximum 4 g daily).
For self-medication, 454 mg (as chewing gum pieces) every 4 hours as necessary (maximum 3.632 g daily).
Rectal
325–650 mg every 4 hours as necessary (maximum 4 g daily).
Inflammatory Diseases
Rheumatoid Arthritis and Arthritis and Pleurisy of SLE
OralInitially, 3 g daily in divided doses. Increase dosage as necessary for anti-inflammatory efficacy; target plasma salicylate concentration is 150–300 mcg/mL. Plasma concentrations >200 mcg/mL associated with an increased incidence of toxicity.
Osteoarthritis
OralUp to 3 g daily in divided doses.
Spondyloarthropathies
OralUp to 4 g daily in divided doses.
Rheumatic Fever†
Oral
Initially, 4.9–7.8 g daily in divided doses given for maximal suppression of acute inflammation. Adjust dosage based on response, tolerance, and plasma salicylate concentrations.
Various regimens suggested depending on severity of initial manifestations. Consult published protocols for more information on specific dosages and schedules.
Transient Ischemic Attacks and Acute Ischemic Stroke
Secondary Prevention
Oral50–325 mg daily; some data suggest lower dosages (75–81 mg daily) may have similar benefits and possibly less bleeding risk.
In patients with noncardioembolic ischemic stroke or TIA, 75–100 mg daily (or 25 mg twice daily, in combination with extended-release dipyridamole 200 mg twice daily) recommended; continue long term.
Acute Treatment†
OralACCP recommends 160–325 mg daily, initiated ideally within 48 hours of stroke onset; may decrease dosage after 1–2 weeks to reduce bleeding risk. (See Transient Ischemic Attacks and Acute Ischemic Stroke: Secondary Prevention, under Dosage.) ACCP states that initiation of aspirin therapy should be delayed for 24 hours following administration of recombinant tissue-type plasminogen activator (r-tPA, e.g., alteplase).
Coronary Artery Disease and Myocardial Infarction
STEMI
Oral162–325 mg as soon as acute STEMI is suspected, continued indefinitely at a dosage of 81–325 mg daily. Some experts prefer use of a maintenance dosage of 81 mg daily because of a decreased risk of bleeding and lack of definitive evidence demonstrating that higher dosages confer greater benefit.
Use in conjunction with a P2Y12-receptor antagonist (e.g., clopidogrel, prasugrel, ticagrelor). If used with ticagrelor, do not exceed aspirin maintenance dosage of 100 mg daily; possible reduced efficacy of ticagrelor with such aspirin dosages.
Primary Prevention† of STEMI
OralSome experts recommend 75–162 mg once daily in carefully selected patients. (See Primary Prevention of Ischemic Cardiac Events under Uses.)
Established Coronary Artery Disease
Oral75–100 mg daily recommended by ACCP; continue indefinitely. Some data suggest lower dosages (75–81 mg daily) may have similar benefits and possibly less bleeding risk.
NSTE ACS
OralACC and AHA recommend an initial dose of 162–325 mg as soon as possible after presentation, unless contraindicated. Continue with maintenance dosage of 81–325 mg daily.
Use in conjunction with a P2Y12-receptor antagonist (e.g., clopidogrel, ticagrelor). If used with ticagrelor, do not exceed aspirin maintenance dosage of 100 mg daily; possible reduced efficacy of ticagrelor with such aspirin dosages.
Percutaneous Coronary Intervention and Coronary Artery Bypass Grafting Surgery
OralPCI in patients already receiving aspirin: 81–325 mg initiated ≥2 hours, and preferably 24 hours, before the procedure in conjunction with a P2Y12-receptor antagonist.
PCI in patients not already receiving long-term aspirin therapy: 325 mg daily (as non-enteric-coated formulation), initiated ≥2 hours, preferably 24 hours, prior to PCI in conjunction with a P2Y12-receptor antagonist.
Maintenance therapy following PCI and stent placement (drug-eluting or bare-metal): 75–162 mg daily in combination with a P2Y12-receptor antagonist. If used with ticagrelor, do not exceed aspirin maintenance dosage of 100 mg daily; possible reduced efficacy of ticagrelor with such aspirin dosages. Administer P2Y12-receptor antagonist for ≥12 months; continue aspirin indefinitely.
CABG: Some manufacturers recommend 325 mg daily, initiated 6 hours after surgery. AHA and ACCF recommend 100–325 mg daily, initiated within 6 hours after CABG and continued for up to 1 year. For long-term therapy after 1 year, ACCP recommends aspirin 75–100 mg daily.
Embolism Associated with Atrial Fibrillation†
Oral
75–325 mg daily suggested for prevention of thromboembolism.
Manage atrial flutter in the same manner as atrial fibrillation.
Mitral Valve Prolapse†
Oral
75–325 mg daily.
Peripheral Arterial Disease
Oral
Primary prevention of cardiovascular events in patients with asymptomatic disease: 75–100 mg daily.
Secondary prevention of cardiovascular events in patients with symptomatic disease: 75–100 mg daily; continue long term.
Patients with refractory intermittent claudication: ACCP suggests the use of cilostazol in addition to aspirin therapy.
Peripheral Artery Bypass Graft Surgery
Oral
To reduce graft occlusion: 75–100 mg daily recommended by ACCP; initiate preoperatively and continue long term.
ACCP suggests addition of clopidogrel 75 mg daily to aspirin therapy in patients undergoing below-the-knee prosthetic graft bypass surgery.
Prosthetic Heart Valves
Mechanical Prosthetic Heart Valves†
OralAspirin 50–100 mg daily in addition to warfarin therapy recommended in all patients with a mechanical heart valve who have a low risk of bleeding.
Aspirin 75–325 mg once daily as monotherapy recommended as an alternative to warfarin in patients who are unable to take warfarin.
Bioprosthetic Heart Valves†
OralPatients with bioprosthetic valves in the aortic position: 50–100 mg daily suggested by ACCP for initial (i.e., first 3 months after valve insertion) and long-term therapy.
Patients with bioprosthetic heart valves in the mitral position: 50–100 mg daily may be used for long-term antithrombotic therapy after initial 3-month treatment with warfarin.
Combination aspirin (75–100 mg daily) and warfarin therapy recommended by ACC/AHA for patients with bioprosthetic heart valves and additional risk factors for thromboembolism.
Aspirin 75–325 mg once daily also recommended as an alternative to warfarin therapy in any patient who is unable to take warfarin.
Complications of Pregnancy†
Oral
Antiphospholipid syndrome† and a history of multiple (≥ 3) pregnancy losses: Antepartum prophylaxis with aspirin (75–100 mg daily) in combination with sub-Q heparin or an LMWH recommended by ACCP.
Patients at risk for preeclampsia: ACCP recommends low-dose aspirin during pregnancy (starting from the second trimester).
Prescribing Limits
Pediatric Patients
Pain
Oral
Children 2–11 years of age: Maximum 2.5 g/m2 daily.
Children ≥12 years of age: Maximum 4 g daily. Maximum 2.6 g as highly buffered effervescent solution (Alka-Seltzer Original) or 3.5 g (Alka-Seltzer Extra Strength) in 24 hours.
For self-medication, do not exceed recommended daily dosage. Treatment duration for self-medication for pain: ≤ 5 days. (See Advice to Patients.) Treatment duration for self-medication of sore throat pain using chewing gum: ≤2 days.
Rectal
Children 2–11 years of age: Maximum 2.5 g/m2 daily.
Children ≥12 years of age: Maximum 4 g daily.
Fever
Oral
Children 2–11 years of age: Maximum 2.5 g/m2 daily.
Children ≥12 years of age: Maximum 4 g daily.
For self-medication, do not exceed recommended daily dosage. Treatment duration for self-medication: <3 days. (See Advice to Patients.)
Rectal
Children 2–11 years of age: Maximum 2.5 g/m2 daily.
Children ≥12 years of age: Maximum 4 g daily.
Adults
Pain
Oral
Maximum 4 g daily. Treatment duration for self-medication for pain: ≤10 days. Aspirin chewing gum should not be used for self-medication of sore throat pain for longer than 2 days. (See Advice to Patients.)
Adults <60 years of age taking highly buffered effervescent solutions: Maximum 2.6 g (Alka-SeltzerLemon-lime or Original) or 3.5 g (Alka-Seltzer Extra Strength) in 24 hours.
Adults ≥60 years of age taking highly buffered effervescent solutions: Maximum 1.3 g (Alka-SeltzerLemon-lime or Original) or 1.5 g (Alka-Seltzer Extra Strength) in 24 hours.
Rectal
Maximum 4 g daily.
Pain Associated with Migraine Headache
OralFor self-medication, maximum 500 mg (in combination with acetaminophen 500 mg and caffeine 130 mg) in 24 hours.
Fever
Oral or Rectal
Maximum 4 g daily.
Special Populations
Geriatric Patients
Highly buffered effervescent solution: Maximum 1.3 g (Alka-SeltzerLemon-Lime or Original) or 1.5 g (Alka-Seltzer Extra Strength) in 24 hours.
Cautions for Aspirin
Contraindications
-
Known hypersensitivity to aspirin or any ingredient in the formulation.
-
History of asthma, urticaria, or other sensitivity reaction precipitated by other NSAIAs.
-
Syndrome of asthma, rhinitis, and nasal polyps.
-
Children or adolescents with viral infections (with or without fever) because of the possibility that the infection may be one associated with an increased risk of Reye’s syndrome. (See Pediatric Use under Cautions.)
Warnings/Precautions
Warnings
Alcohol
Long-term heavy alcohol use (≥3 alcoholic beverages daily) associated with an increased risk of aspirin-induced bleeding. (See Advice to Patients.)
Hematologic Effects
Inhibits platelet aggregation and may prolong bleeding time. These effects may be particularly important in patients with inherited (e.g., hemophilia) or acquired (e.g., liver disease, vitamin K deficiency) bleeding disorders.
Because of the increased risk of bleeding, avoid aspirin-containing chewing gum tablets or gargles for ≥1 week after tonsillectomy or oral surgery.
GI Effects
Serious GI toxicity (e.g., bleeding, ulceration, perforation) can occur with or without warning symptoms. Increased risk in those with a history of GI bleeding or ulceration, geriatric patients, and those receiving an anticoagulant or corticosteroid, receiving excessive dosages or prolonged therapy, taking multiple NSAIAs concomitantly, or consuming ≥3 alcohol-containing beverages daily.
Avoid in patients with active peptic ulcer disease; can cause gastric mucosal irritation and bleeding.
Despite current warnings on OTC product labels, serious bleeding events continue to occur in patients receiving aspirin in fixed combination with antacids for self-medication. FDA is evaluating whether additional actions are needed to address this safety concern.
Thrombosis Associated with Drug-eluting Stents
Stent thrombosis with potentially fatal sequelae, particularly with drug-eluting stents (DES), associated with premature discontinuance (<12 months) of dual-drug therapy with a thienopyridine derivative and aspirin. (See Percutaneous Coronary Intervention and Revascularization Procedures under Uses.)
At least 12 months of dual-drug antiplatelet therapy is recommended in patients with any type of coronary artery stent (bare-metal or drug-eluting). Preliminary evidence from a randomized controlled study suggests that an even longer duration (up to 30 months) of dual-drug antiplatelet therapy may be beneficial in reducing stent thrombosis and other cardiovascular events in patients with a drug-eluting stent; however, such prolonged therapy was associated with increased bleeding and an unexpected finding of increased all-cause mortality. FDA is continuing to evaluate these findings and will communicate final conclusions and recommendations once the analysis is complete.
For non-elective procedures that mandate premature discontinuance of thienopyridine-derivative therapy, continue aspirin therapy if at all possible. Restart thienopyridine therapy as soon as possible after the procedure. (See Advice to Patients.)
Sensitivity Reactions
Anaphylactoid reactions, severe urticaria, angioedema, or bronchospasm reported. Immediate medical intervention and discontinuance for anaphylaxis.
Potentially fatal or life-threatening syndrome of multi-organ hypersensitivity (i.e., drug reaction with eosinophilia and systemic symptoms [DRESS]) reported in patients receiving NSAIAs. Clinical presentation is variable, but typically includes eosinophilia, fever, rash, lymphadenopathy, and/or facial swelling, possibly associated with other organ system involvement (e.g., hepatitis, nephritis, hematologic abnormalities, myocarditis, myositis). Symptoms may resemble those of acute viral infection. Early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present in the absence of rash. If signs or symptoms of DRESS develop, discontinue the drug and immediately evaluate the patient.
Contraindicated in patients with syndrome of asthma, rhinitis, and nasal polyps; caution in patients with asthma.
General Precautions
Sodium Content
Avoid highly buffered aspirin preparations in patients with CHF, renal failure, or other conditions in which high sodium content would be harmful.
Individuals with Phenylketonuria
Some preparations contain aspartame (NutraSweet), which is metabolized in the GI tract to phenylalanine.
Use of Fixed Combinations
When aspirin is used in fixed combination with other agents, consider the cautions, precautions, and contraindications associated with the other agent(s).
Specific Populations
Pregnancy
Use of NSAIAs during pregnancy at about ≥30 weeks’ gestation can cause premature closure of the fetal ductus arteriosus; use at about ≥20 weeks’ gestation associated with fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment.
Effects of NSAIAs on the human fetus during third trimester of pregnancy include prenatal constriction of the ductus arteriosus, tricuspid incompetence, and pulmonary hypertension; nonclosure of the ductus arteriosus during the postnatal period (which may be resistant to medical management); and myocardial degenerative changes, platelet dysfunction with resultant bleeding, intracranial bleeding, renal dysfunction or renal failure, renal injury or dysgenesis potentially resulting in prolonged or permanent renal failure, oligohydramnios, GI bleeding or perforation, and increased risk of necrotizing enterocolitis.
Avoid use of NSAIAs in pregnant women at about ≥30 weeks’ gestation; if use required between about 20 and 30 weeks’ gestation, use lowest effective dosage and shortest possible duration of treatment, and consider monitoring amniotic fluid volume via ultrasound examination if treatment duration >48 hours; if oligohydramnios occurs, discontinue drug and follow up according to clinical practice. However, FDA states that these recommendations do not apply to low-dose aspirin therapy; low (e.g., 81-mg) doses of aspirin may be used under the direction of a clinician at any time during pregnancy for the treatment of certain pregnancy-related conditions. (See Advice to Patients.)
Fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment observed, on average, following days to weeks of maternal NSAIA use; infrequently, oligohydramnios observed as early as 48 hours after initiation of NSAIAs. Oligohydramnios is often, but not always, reversible (generally within 3–6 days) following NSAIA discontinuance. Complications of prolonged oligohydramnios may include limb contracture and delayed lung maturation. In limited number of cases, neonatal renal dysfunction (sometimes irreversible) occurred without oligohydramnios. Some neonates have required invasive procedures (e.g., exchange transfusion, dialysis). Deaths associated with neonatal renal failure also reported. Limitations of available data (lack of control group; limited information regarding dosage, duration, and timing of drug exposure; concomitant use of other drugs) preclude a reliable estimate of the risk of adverse fetal and neonatal outcomes with maternal NSAIA use. Available data on neonatal outcomes generally involved preterm infants; extent to which risks can be generalized to full-term infants is uncertain.
Animal data indicate important roles for prostaglandins in kidney development and endometrial vascular permeability, blastocyst implantation, and decidualization. In animal studies, inhibitors of prostaglandin synthesis increased pre- and post-implantation losses; also impaired kidney development at clinically relevant doses.
Maternal and fetal hemorrhagic complications observed with maternal ingestion of large doses (e.g., 12–15 g daily) of aspirin generally have not been observed in studies in which low doses (60–150 mg daily) of the drug were used for prevention of complications of pregnancy†.
Lactation
Distributed into milk; use not recommended. High doses may result in adverse effects (rash, platelet abnormalities, bleeding) in nursing infants.
Pediatric Use
Dosing recommendations for juvenile rheumatoid arthritis based on well controlled clinical studies. High dosages that result in plasma concentrations >200 mcg/mL associated with an increased incidence of toxicity.
Use in children with varicella infection or influenza-like illnesses reportedly is associated with an increased risk of developing Reye’s syndrome. US Surgeon General, AAP Committee on Infectious Diseases, FDA, and other authorities advise that salicylates not be used in children and teenagers with varicella or influenza, unless directed by a clinician. Generally avoid salicylates in children and teenagers with suspected varicella or influenza and during presumed outbreaks of influenza, since accurate diagnosis of these diseases may be impossible during the prodromal period; use of salicylates in the management of viral infections in children or adolescents is contraindicated, since the infection may be one associated with an increased risk of Reye’s syndrome.
Use with caution in pediatric patients who are dehydrated (increased susceptibility to salicylate intoxication).
Safety and efficacy of aspirin in fixed combination with extended-release dipyridamole not established.
Risk of overdosage and toxicity (including death) in children <2 years of age receiving preparations containing antihistamines, cough suppressants, expectorants, and nasal decongestants alone or in combination for relief of symptoms of upper respiratory tract infection. Limited evidence of efficacy for these preparations in this age group; appropriate dosages not established. Use such preparations in children <2 years of age with caution and only as directed by clinician. Clinicians should ask caregivers about use of OTC cough/cold preparations to avoid overdosage.
Hepatic Impairment
Avoid in patients with severe hepatic impairment.
Renal Impairment
Avoid in patients with GFR <10 mL/minute.
Common Adverse Effects
Minor upper GI symptoms (dyspepsia).
Drug Interactions
Protein-bound Drugs
Potential for salicylate to be displaced from binding sites by, or to displace from binding sites, other protein-bound drugs. Aspirin acetylates serum albumin, which may alter binding of other drugs to the protein.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Reduced BP response to ACE inhibitors Possible attenuation of hemodynamic actions of ACE inhibitors in patients with CHF Reduced hyponatremic effect of ACE inhibitors |
Monitor BP |
|
Acidifying agents |
Drugs that decrease urine pH may decrease salicylate excretion |
|
|
Alcohol |
Increased risk of bleeding (see Advice to Patients) |
|
|
Alkalinizing agents |
Drugs that increase urine pH may increase salicylate excretion |
Monitor plasma salicylate concentrations in patients receiving high-dose aspirin therapy if antacids are initiated or discontinued |
|
Anticoagulants (warfarin, heparin) |
Increased risk of bleeding May displace warfarin from protein-binding sites, leading to prolongation of PT and bleeding time |
Use with caution |
|
Anticonvulsants |
May displace phenytoin from binding sites; possible decrease in total plasma phenytoin concentrations, with increased free fraction May displace valproic acid from binding sites; possible increase in free plasma valproic acid concentrations; possible increased risk of bleeding |
Monitor patients receiving aspirin with valproic acid |
|
Antidiabetic drugs (sulfonylureas) |
Potential for increased hypoglycemic effect |
Monitor closely |
|
β-adrenergic blocking agents |
Reduced BP response to β-adrenergic blocking agents Potential for salt and fluid retention |
Monitor BP |
|
Carbonic anhydrase inhibitors (acetazolamide) |
Increased risk of salicylate toxicity Increased plasma acetazolamide concentrations; increased risk of acetazolamide toxicity |
Avoid concomitant use in patients receiving high-dose aspirin |
|
Corticosteroids |
Decreased plasma salicylate concentrations |
Monitor for adverse effects of either drug |
|
Diuretics |
Possible reduced natriuretic effect |
|
|
Methotrexate |
Increased plasma methotrexate concentrations Inhibition of renal clearance of methotrexate leading to bone marrow toxicity, especially in geriatric patients or patients with renal impairment |
Monitor for methotrexate toxicity |
|
NSAIAs |
Increased risk of bleeding, GI ulceration, decreased renal function, or other complications No consistent evidence that low-dose aspirin mitigates increased risk of serious cardiovascular events associated with NSAIAs Pharmacokinetic interactions with many NSAIAs Antagonism (ibuprofen, naproxen) of the irreversible platelet-aggregation inhibitory effect of aspirin; may limit the cardioprotective effects of aspirin Minimal risk of attenuating effects of low-dose aspirin with occasional use of ibuprofen Not known whether ketoprofen interferes with the antiplatelet effect of aspirin Decreased peak plasma concentration and AUC of diclofenac; limited data indicate that diclofenac does not inhibit antiplatelet effect of aspirin |
Concomitant use not recommended Pharmacokinetic interactions unlikely to be clinically important Immediate-release aspirin: Administer a single dose of ibuprofen 400 mg for self-medication≥8 hours before or ≥30 minutes after administration of aspirin Enteric-coated low-dose aspirin: No recommendations regarding timing of administration with single dose of ibuprofen Consider use of alternative analgesics that do not interfere with antiplatelet effect of low-dose aspirin (e.g., acetaminophen, opiates) for patients at high risk of cardiovascular events Concomitant use with prescription NSAIAs not recommended because of potential for increased adverse effects |
|
Pyrazinamide |
Possible prevention or reduction of hyperuricemia associated with pyrazinamide |
|
|
Tetracycline |
Decreased oral absorption of tetracyclines when administered with aspirin preparations containing divalent or trivalent cations (Bufferin) |
Administer preparations containing divalent or trivalent cations (Bufferin) 1 hr before or after tetracycline |
|
Thrombolytic agents |
Additive reduction in mortality reported in patients with AMI receiving aspirin in low dosages and thrombolytic agents (streptokinase, alteplase) |
Used for therapeutic effect |
|
Uricosuric agents (probenecid, sulfinpyrazone) |
Reduced uricosuric effect of uricosuric agents |
|
|
Varicella virus vaccine live |
Theoretical possibility of Reye’s syndrome |
Manufacturer of varicella virus vaccine live recommends that individuals who receive the vaccine avoid use of salicylates for 6 weeks following vaccination For children who are receiving long-term salicylate therapy, AAP suggests weighing theoretical risks of vaccination against known risks of wild-type virus; ACIP states that children who have rheumatoid arthritis or other conditions requiring therapeutic salicylate therapy probably should receive varicella virus vaccine live in conjunction with subsequent close monitoring |
Aspirin Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration. Rapidly metabolized to salicylic acid; plasma aspirin concentrations are undetectable 1–2 hours after administration. Peak plasma salicylic acid concentrations attained within 1–2 hours following administration of uncoated tablets.
Slowly and variably absorbed following rectal administration.
Onset
Single oral doses of rapidly absorbed preparations: 30 minutes for analgesic and antipyretic effects.
Rectal suppositories: 1–2 hours for antipyretic effects.
Continuous oral therapy: 1–4 days for anti-inflammatory effect.
Food
Food decreases rate but not extent of absorption; peak plasma concentrations of aspirin and salicylate may be decreased.
Plasma Concentrations
Plasma salicylate concentrations of 30–100 mcg/mL produce analgesia and antipyresis; the concentration required for anti-inflammatory effect is 150–300 mcg/mL; toxicity noted at 300–350 mcg/mL.
Steady-state plasma salicylate concentrations increase more than proportionally with increasing doses as a result of capacity-limiting processes.
Special Populations
During the febrile phase of Kawasaki disease, oral absorption may be impaired or highly variable.
Distribution
Extent
Widely distributed; aspirin and salicylate distribute into synovial fluid. Crosses placenta and distributed into milk.
Plasma Protein Binding
Aspirin: 33%.
Salicylate: 90–95% bound at plasma salicylate concentrations <100 mcg/mL; 70–85% bound at concentrations of 100–400 mcg/mL; 25–60% bound at concentrations >400 mcg/mL.
Elimination
Metabolism
Partially hydrolyzed to salicylate by esterases in the GI mucosa. Unhydrolyzed aspirin subsequently undergoes hydrolysis by esterases mainly in the liver but also in plasma, erythrocytes, and synovial fluid.
Salicylate is metabolized in the liver by the microsomal enzyme system.
Elimination Route
Excreted in urine via glomerular filtration and renal tubular reabsorption as salicylate and its metabolites. Urinary excretion of salicylate is pH dependent; as urine pH increases from 5 to 8, urinary excretion of salicylate is greatly increased.
Half-life
Aspirin: 15–20 minutes.
Half-life of salicylate increases with increasing plasma salicylate concentrations.
Salicylate: 2–3 hours when aspirin administered in low doses (325 mg).
Salicylate: 15–30 hours when aspirin administered in higher dosages.
Special Populations
Salicylate and its metabolites readily removed by hemodialysis and, to a lesser extent, by peritoneal dialysis.
Stability
Storage
Oral
Capsules
Aspirin in fixed-combination with extended-release dipyridamole: 25°C (may be exposed to 15–30°C). Protect from excessive moisture.
Gum
15–25°C; protect from excessive moisture.
Tablets
Room temperature (Bayer products, excluding Alka-Seltzer products); avoid high humidity and excessive heat (40°C).
15–30°C (Easprin).
20–25°C (Anacin Extra Strength); protect from moisture.
Protect from excessive heat (Alka-Seltzer products).
Rectal
Suppositories
2–15°C.
Actions
-
Inhibits COX-1 and COX-2 activity.
-
Pharmacologic actions similar to those of prototypical NSAIAs; exhibits anti-inflammatory, analgesic, and antipyretic activity.
-
Irreversibly acetylates and inactivates COX-1 in platelets.
-
The existence of 2 COX isoenzymes with different aspirin sensitivities and extremely different recovery rates of their COX activity following inactivation by aspirin at least partially explains the different dosage requirements and durations of aspirin effects on platelet function versus the drug’s analgesic and anti-inflammatory effects.
-
Effects on urinary excretion of uric acid are dose related; large dosages (e.g., 1.3 g 4 times daily) enhance urinary excretion and decrease serum concentrations of uric acid , intermediate dosages (e.g., 650 mg to 1 g 3 times daily) usually do not alter uric acid excretion, and low dosages (e.g., <325 mg 3 times daily) inhibit excretion and may increase serum uric acid concentrations.
Advice to Patients
-
When used for self-medication, importance of reading the product labeling.
-
When used for self-medication, importance of asking clinician whether to use aspirin or another analgesic if alcohol consumption is ≥3 alcohol-containing drinks per day.
-
Importance of informing patients about risk of bleeding associated with chronic, heavy alcohol use while taking aspirin.
-
When used for self-medication in children, importance of basing the dose on the child’s weight or body surface area.
-
In patients with drug-eluting stents (DES) receiving aspirin in combination with clopidogrel or ticlopidine, importance of not discontinuing antiplatelet therapy without consulting cardiologist, even if instructed to do so by other health-care professional (e.g., dentist).
-
Importance of not using aspirin for chicken pox or flu symptoms in children or adolescents without consulting a clinician.
-
Patients receiving anticoagulants and those with asthma, gout, diabetes, arthritis, peptic ulcers, bleeding problems, or stomach problems that persist or recur should consult a clinician before using aspirin for self-medication.
-
Discontinue and consult clinician if pain or fever persists or progresses, new symptoms occur, redness or swelling is present in a painful area, or ringing in the ears or loss of hearing occurs.
-
Risk of GI bleeding or ulceration, particularly with prolonged therapy, and concomitant therapy with another NSAIA.
-
Risk of anaphylactoid and other sensitivity reactions.
-
Importance of notifying clinician if signs and symptoms of GI ulceration or bleeding or rash develop.
-
Importance of seeking immediate medical attention if an anaphylactic reaction occurs.
-
Importance of women informing clinicians if they are or plan to become pregnant or to breast-feed.
-
Importance of avoiding NSAIA use beginning at 20 weeks’ gestation unless otherwise advised by a clinician; importance of avoiding NSAIAs beginning at 30 weeks’ gestation because of risk of premature closure of the fetal ductus arteriosus; monitoring for oligohydramnios may be necessary if NSAIA therapy required for >48 hours’ duration between about 20 and 30 weeks’ gestation.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Pieces, chewing gum |
227 mg |
Aspergum |
Heritage |
|
Tablets |
81 mg* |
Aspirin Tablets |
||
|
325 mg* |
Aspirin Tablets |
|||
|
Norwich Aspirin |
Chattem |
|||
|
500 mg* |
Aspirin Tablets |
|||
|
Norwich Aspirin Maximum Strength |
Chattem |
|||
|
650 mg* |
Aspirin Tablets |
|||
|
Tablets, chewable |
81 mg* |
Aspirin Chewable Tablets |
||
|
Bayer Aspirin Children’s |
Bayer |
|||
|
St. Joseph Aspirin Low Strength Adult Chewable |
McNeil |
|||
|
Tablets, delayed-release (enteric-coated) |
81 mg* |
Aspirin Delayed-release (Enteric-coated) Tablets |
||
|
Bayer Aspirin Regimen Adult Low Strength |
Bayer |
|||
|
Ecotrin Adult Low Strength |
GlaxoSmithKline |
|||
|
Halfprin |
Kramer |
|||
|
St. Joseph Pain Reliever Adult |
McNeil |
|||
|
162 mg |
Halfprin |
Kramer |
||
|
325 mg* |
Aspirin Delayed-release (Enteric-coated) Tablets |
|||
|
Bayer Aspirin Regimen Regular Strength Caplets |
Bayer |
|||
|
Ecotrin Regular Strength |
GlaxoSmithKline |
|||
|
Genacote |
Ivax |
|||
|
500 mg* |
Aspirin Delayed-release (Enteric-coated) Tablets |
|||
|
Ecotrin Maximum Strength |
GlaxoSmithKline |
|||
|
650 mg* |
Aspirin Delayed-release (Enteric-coated) Tablets |
|||
|
975 mg* |
Aspirin Delayed-release (Enteric-coated) Tablets |
|||
|
Easprin |
Rosedale |
|||
|
Tablets, extended-release |
800 mg |
ZORprin |
Par |
|
|
Tablets, film-coated |
325 mg* |
Aspirin Tablets |
||
|
Genuine Bayer Aspirin Tablets |
Bayer |
|||
|
500 mg |
Bayer Extra Strength Aspirin Caplets |
Bayer |
||
|
Rectal |
Suppositories |
60 mg* |
Aspirin Suppositories |
|
|
120 mg* |
Aspirin Suppositories |
|||
|
200 mg* |
Aspirin Suppositories |
|||
|
300 mg* |
Aspirin Suppositories |
|||
|
600 mg* |
Aspirin Suppositories |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, enteric-coated |
325 mg with buffers |
Ascriptin Enteric Regular Strength |
Novartis |
|
Tablets, film-coated |
81 mg with buffers |
Women’s Bayer Aspirin Plus Calcium Caplets |
Bayer |
|
|
325 mg with buffers |
Ascriptin Arthritis Pain Caplets |
Novartis |
||
|
Ascriptin Regular Strength |
Novartis |
|||
|
Bufferin Tablets |
Novartis |
|||
|
500 mg with buffers |
Ascriptin Maximum Strength Caplets |
Novartis |
||
|
Bayer Plus Extra Strength Caplets |
Bayer |
|||
|
Bufferin Extra Strength Caplets |
Novartis |
|||
|
Bufferin Extra Strength |
Novartis |
|||
|
Tablets, for solution |
325 mg |
Alka-Seltzer Effervescent Pain Reliever and Antacid |
Bayer |
|
|
Alka-Seltzer Lemon Lime Effervescent Pain Reliever and Antacid |
Bayer |
|||
|
500 mg |
Alka-Seltzer Extra Strength Effervescent Pain Reliever and Antacid |
Bayer |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
For solution |
325 mg/packet Acetaminophen and Aspirin 500 mg/packet |
Goody’s Back & Body Pain Powder |
Prestige |
|
Tablets, film-coated |
250 mg Acetaminophen, Aspirin 250 mg, and buffer |
Excedrin Back and Body Caplets |
Novartis |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, gel-coated |
250 mg Acetaminophen, Aspirin 250 mg, and Caffeine 65 mg* |
Acetaminophen, Aspirin, and Caffeine Gelcaps |
|
|
Excedrin Menstrual Complete Gelcaps |
Novartis |
|||
|
For solution |
260 mg/packet Acetaminophen, Aspirin 520 mg/packet, and Caffeine 32.5 mg/packet |
Goody’s Extra Strength Headache Powder |
Prestige |
|
|
325 mg/packet Acetaminophen, Aspirin 500 mg/packet, and Caffeine 65 mg/packet |
Goody’s Cool Orange Extra Strength Powder |
Prestige |
||
|
Tablets, film-coated |
194 mg Acetaminophen, Aspirin 227 mg, Caffeine 33 mg, and buffers |
Vanquish Caplets |
Moberg |
|
|
250 mg Acetaminophen, Aspirin 250 mg, and Caffeine 65 mg |
Excedrin Extra Strength Caplets |
Novartis |
||
|
Excedrin Migraine Caplets |
Novartis |
|||
|
Goody's Extra Strength Caplets |
Prestige |
|||
|
Pamprin Max |
Chattem |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
4.8355 mg Oxycodone Hydrochloride and Aspirin 325 mg* |
Endodan (C-II) |
Qualitest |
|
Oxycodone Hydrochloride and Aspirin Tablets (C-II) |
||||
|
Percodan (C-II; scored) |
Endo |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
325 mg with Butalbital 50 mg and Caffeine 40 mg* |
Butalbital, Aspirin, and Caffeine Capsules (C-III) |
|
|
Fiorinal (C-III) |
Actavis |
|||
|
325 mg with Butalbital 50 mg, Caffeine 40 mg, and Codeine Phosphate 30 mg* |
Butalbital, Aspirin, Caffeine, and Codeine Phosphate Capsules (C-III) |
|||
|
Fiorinal with Codeine (C-III) |
Actavis |
|||
|
356.4 mg with Caffeine 30 mg and Dihydrocodeine Bitartrate 16 mg |
Synalgos-DC (C-III) |
Leitner |
||
|
Capsules, extended-release core (dipyridamole only) |
25 mg with Dipyridamole 200 mg |
Aggrenox |
Boehringer Ingelheim |
|
|
For solution |
845 mg/packet with Caffeine 65 mg/packet |
BC Powder |
Prestige |
|
|
Stanback Powder |
Prestige |
|||
|
1000 mg/packet with Caffeine 65 mg/packet |
BC Powder Arthritis Strength |
Prestige |
||
|
Tablets |
325 mg with Butalbital 50 mg and Caffeine 40 mg* |
Butalbital, Aspirin, and Caffeine Tablets (C-III) |
||
|
Fortabs (C-III) |
United Research |
|||
|
325 mg with Carisoprodol 200 mg* |
Carisoprodol and Aspirin Tablets (C-IV) |
|||
|
Soma Compound (C-IV) |
Meda |
|||
|
325 mg with Carisoprodol 200 mg and Codeine Phosphate 16 mg* |
Carisoprodol, Aspirin, and Codeine Phosphate Tablets (C-III) |
|||
|
Soma Compound with Codeine (C-III) |
Meda |
|||
|
325 mg with Meprobamate 200 mg |
Equagesic (C-IV; scored) |
Leitner |
||
|
Micrainin (C-IV) |
Wallace |
|||
|
385 mg with Caffeine 30 mg and Orphenadrine Citrate 25 mg* |
Norgesic |
3M |
||
|
Orphenadrine Citrate, Aspirin, and Caffeine Tablets |
Sandoz |
|||
|
400 mg with Caffeine 32 mg |
P-A-C Analgesic |
Lee |
||
|
770 mg with Caffeine 60 mg, and Orphenadrine Citrate 50 mg* |
Norgesic Forte (scored) |
3M |
||
|
Orphenadrine Citrate, Aspirin, and Caffeine Tablets |
Sandoz |
|||
|
Tablets, film-coated |
400 mg with Caffeine 32 mg |
Anacin Caplets |
Wyeth |
|
|
Anacin Tablets |
Wyeth |
|||
|
421 mg with Caffeine 32 mg and buffers |
Cope |
Lee |
||
|
500 mg with Caffeine 32 mg |
Anacin Maximum Strength |
Wyeth |
||
|
500 mg with Caffeine 32.5 mg |
Extra Strength Bayer Back and Body Pain (with propylene glycol) |
Bayer |
||
|
Tablets, for solution |
500 mg with Caffeine 65 mg |
Alka Seltzer Morning Relief |
Bayer |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions November 29, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
- What's the difference between aspirin and ibuprofen?
- Can you take tramadol with acetaminophen, ibuprofen, or aspirin?
- What temperature is considered a fever?
- Aspirin Overdose: Symptoms, Diagnosis, Emergency Treatment
- Which painkiller should you use?
- Can I give Aspirin to my dog or cat?
- Can you take ibuprofen with Excedrin Migraine?
More about aspirin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (49)
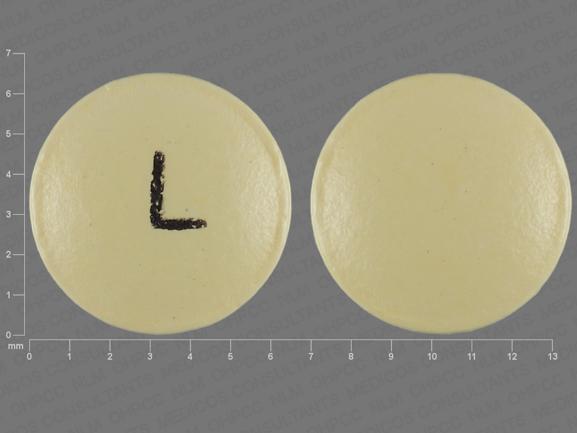
- Drug images
- Latest FDA alerts (3)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: platelet aggregation inhibitors
- Breastfeeding