Leucovorin (Monograph)
Brand name: Wellcovorin
Drug class: Antidotes
VA class: VT102
CAS number: 6035-45-6
Introduction
Folic acid derivative; antidote for folic acid antagonists.
Uses for Leucovorin
Toxicity Associated with Folic Acid Antagonists
Antidote for unintentional overdosage of methotrexate (e.g., resulting from impaired elimination) and other folic acid antagonists (e.g., pyrimethamine, trimethoprim).
IV rescue therapy after high-dose methotrexate regimen (to control duration of exposure of sensitive cells to methotrexate) in the treatment of osteosarcoma (designated an orphan drug by FDA for this use).
Prevention of hematologic toxicity† [off-label] associated with pyrimethamine, trimethoprim, or trimetrexate therapy.
Megaloblastic Anemia
IV treatment of folate deficient megaloblastic anemias (e.g., serum folate concentration <0.002 mcg/mL) of infancy, pregnancy, sprue, and nutritional deficiencies when oral folic acid therapy is not feasible. No advantage over folic acid injection since ability to convert folic acid to tetrahydrofolic acid (THF) is not impaired in these anemias.
Effective in the treatment of megaloblastic anemia resulting from congenital dihydrofolate reductase deficiency† [off-label].
Not effective in the treatment of pernicious anemia and other megaloblastic anemias secondary to lack of vitamin B12; avoid such use. (See Contraindications under Cautions.)
Colorectal Cancer
Adjunct to fluorouracil to prolong survival in the palliative treatment of advanced colorectal cancer (designated an orphan drug by FDA for this use).
First-line therapy for management of advanced colorectal cancer in a combination regimen consisting of fluorouracil, leucovorin, and either irinotecan or oxaliplatin.
Related/similar drugs
Opdivo, azithromycin, clindamycin, sulfamethoxazole / trimethoprim, Bactrim, folic acid, Zithromax
Leucovorin Dosage and Administration
General
Toxicity Associated with Folic Acid Antagonists
- Methotrexate Overdosage or Rescue after High-dose Methotrexate Therapy
-
Monitoring of serum methotrexate concentration required to determine optimum dose and duration of leucovorin therapy.
-
Maintain adequate hydration (3 L daily) and administer sodium bicarbonate to maintain urinary pH at ≥7 during therapy.
-
Monitor fluid and electrolyte status in patients experiencing delayed early methotrexate elimination and nonoliguric renal failure until methotrexate concentration declines to <0.023 mcg/mL (0.05 μM) and renal failure has resolved.
- Prevention of Pyrimethamine Toxicity† [off-label]
-
Dosage of leucovorin necessary to prevent hematologic toxicity varies depending on the dosage of the folic acid antagonist and patient’s clinical status.
- Prevention of Trimetrexate Toxicity† [off-label]
-
Monitoring of neutrophil counts and platelet counts required; modify dosage of trimetrexate and leucovorin based on the worst of the two blood cell counts. (See Table 4.)
Administration
Administer orally or by IV or IM injection.
Administer parenterally rather than orally in patients with GI toxicity (e.g., nausea, vomiting) and in those receiving individual doses >25 mg. Parenteral administration also preferred if possibility of vomiting and/or decreased GI absorption exists.
Do not administer intrathecally (potentially harmful or fatal).
Oral Administration
Saturable absorption; administration of doses >25 mg not recommended. (See Absorption under Pharmacokinetics.)
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
If used concomitantly with fluorouracil, administer separately to avoid possible formation of a precipitate. However, no visually apparent precipitate was detected when the drugs were injected sequentially (with no flush between) into Y-site. (See Compatibility under Stability.)
Reconstitution
Add 5, 10, or 20 mL of sterile water for injection or bacteriostatic water for injection (benzyl alcohol-preserved) to vial containing 50, 100, or 200 mg of leucovorin, respectively, to provide a solution containing 10 mg/mL.
For vial containing 350 mg of leucovorin, reconstitute with 17.5 mL of sterile water for injection or bacteriostatic water for injection to provide a solution containing 20 mg/mL.
Due to benzyl alcohol content in bacteriostatic water for injection, reconstitute with sterile water for injection when preparing doses >10 mg/m2.
Rate of Administration
Due to calcium content, administer no more than 160 mg per minute (16 mL of a 10-mg/mL solution or 8 mL of a 20-mg/mL solution per minute).
For prevention of trimetrexate toxicity† [off-label], administer dose over 5–10 minutes.
Dosage
Available as leucovorin calcium; dosage expressed in terms of leucovorin.
Pediatric Patients
Toxicity Associated with Folic Acid Antagonists
Prevention of Pyrimethamine Toxicity†
OralFor pyrimethamine dosages of 25–100 mg daily or 1–2 mg/kg daily (for treatment of toxoplasmosis): 10–25 mg administered with each pyrimethamine dose.
For pyrimethamine dosages of 25–50 mg once daily (given with clindamycin or sulfadiazine for secondary prophylaxis of toxoplasmosis in adolescents): 10–25 mg once daily.
For pyrimethamine dosage of 1 mg/kg once daily (given with dapsone or clindamycin for primary or secondary prophylaxis of toxoplasmosis, respectively, in HIV-infected children): 5 mg once every 3 days.
For pyrimethamine dosage of 25 mg once daily (given with atovaquone for primary or secondary prophylaxis against toxoplasmosis in HIV-infected adolescents): 10 mg daily, administered concomitantly with pyrimethamine.
For pyrimethamine dosage of 50 or 75 mg once weekly (given with dapsone for primary prevention of Pneumocystis jiroveci [formerly Pneumocystis carinii] pneumonia or toxoplasmosis or for secondary prophylaxis of P. jiroveci pneumonia in HIV-infected adolescents): 25 mg once weekly, administered concomitantly with pyrimethamine.
Adults
Toxicity Associated with Folic Acid Antagonists
Methotrexate Overdosage
Dosage is approximately twice that of levoleucovorin (the active l-isomer).
Oral, IV, or IM15 mg (approximately 10 mg/m2) every 6 hours until serum methotrexate concentration declines to <0.005 mcg/mL (0.01 μM); initiate administration as soon as possible after overdosage and within 24 hours following methotrexate administration if delayed elimination is detected. (See Table 1 and Table 2 under Dosage and Administration.)
If 24-hour Scr increases 50% over baseline, 24-hour methotrexate concentration is >2.27 mcg/mL (5 μM, or 48-hour methotrexate concentration is >0.409 mcg/mL (0.9 μM), increase dosage immediately to 150 mg (approximately 100 mg/m2) IV every 3 hours until serum methotrexate concentration declines to <0.005 mcg/mL (0.01 μM).
Pyrimethamine or Trimethoprim Overdosage
Oral5–15 mg daily is recommended by some clinicians.
Rescue after High-dose Methotrexate Therapy
Dosage is approximately twice that of levoleucovorin (the active l-isomer).
Oral, IV, or IM15 mg (approximately 10 mg/m2) every 6 hours for 10 doses, starting at 24 hours after initiation of methotrexate (12–15 g/m2) infusion for patients with normal methotrexate elimination (i.e., serum methotrexate concentration approximately 4.54 mcg/mL [10 μM] at 24 hours after administration, 0.454 mcg/mL [1 μM] at 48 hours, and <0.091 mcg/mL [0.2 μM] at 72 hours).
Continue therapy and maintain adequate hydration and urinary alkalization (pH ≥7) until methotrexate concentration declines to <0.023 mcg/mL (0.05 μM).
If substantial clinical toxicity occurs in patients with mild abnormalities in methotrexate elimination or renal function, extend rescue therapy for an additional 24 hours (i.e., 14 doses over 84 hours) for subsequent methotrexate courses.
Monitor Scr and methotrexate concentration at least once daily. Adjust dosage and duration of therapy based on methotrexate elimination pattern and patient’s renal function. (See Tables 1 and 2.)
|
Serum Methotrexate Concentration |
Leucovorin Dosage Adjustment |
|---|---|
|
>0.091 mcg/mL (0.2 μM) at 72 hours and >0.023 mcg/mL (0.05 μM) at 96 hours following methotrexate administration |
Continue leucovorin 15 mg every 6 hours until methotrexate concentration declines to <0.023 mcg/mL (0.05 μM) |
|
Serum Methotrexate and/or Scr Concentration |
Leucovorin Dosage Adjustment and Monitoring |
|---|---|
|
≥22.7 mcg/mL (50 μM) at 24 hours or ≥2.27 mcg/mL (5 μM) at 48 hours after methotrexate administration and/or ≥100% increase in Scr at 24 hours after administration |
Leucovorin 150 mg IV every 3 hours until methotrexate concentration declines to <0.454 mcg/mL (1 μM), then leucovorin 15 mg IV every 3 hours until methotrexate concentration declines to <0.023 mcg/mL (0.05 μM) If nonoliguric renal failure develops, monitor fluid and electrolyte status until methotrexate concentration declines to 0.023 mcg/mL (0.05 μM) and renal failure has resolved |
Prevention of Pyrimethamine Toxicity†
OralFor pyrimethamine dosages of 25–100 mg daily or 1–2 mg/kg daily (for treatment of toxoplasmosis): 10–25 mg administered with each pyrimethamine dose.
For pyrimethamine dosages of 25–50 mg once daily (given with clindamycin or sulfadiazine for secondary prophylaxis of toxoplasmosis): 10–25 mg once daily.
For pyrimethamine dosage of 25 mg once daily (given with atovaquone for primary or secondary prophylaxis of toxoplasmosis in HIV-infected individuals): 10 mg daily, administered concomitantly with pyrimethamine.
For pyrimethamine dosage of 50 or 75 mg once weekly (given with dapsone for primary prevention of P. jiroveci pneumonia or toxoplasmosis or for secondary prophylaxis of P. jiroveci pneumonia in HIV-infected individuals): 25 mg once weekly, administered concomitantly with pyrimethamine.
Prevention of Trimetrexate Toxicity†
Oral or IVFor trimetrexate dose of 45 mg/m2: 20 mg/m2 every 6 hours (total daily dose: 80 mg/m2).
Alternatively, dose may be based on body weight. (See Table 3.)
|
Body Weight (kg) |
Trimetrexate Dosage (mg/kg/day) |
Leucovorin Dosage (mg/kg Every 6 Hours) |
|---|---|---|
|
<50 |
1.5 |
0.6 |
|
50–80 |
1.2 |
0.5 |
|
>80 |
1.0 |
0.5 |
Round calculated oral dose up to the next 25-mg increment.
Continue leucovorin therapy for at least 72 hours after last trimetrexate dose (usual duration: 24 days).
Adjust dosage if hematologic toxicities occur, based on the worst of the two blood cell counts. (See Table 4.)
Adjust dosage based on the worse of the two blood counts
|
Toxicity Grade |
ANC (cells/mm3) |
Platelets (cells/mm3) |
Dosage Adjustments |
|---|---|---|---|
|
1 |
>1000 |
>75,000 |
No adjustment in trimetrexate or leucovorin dosages |
|
2 |
750–1000 |
50,000–75,000 |
No adjustment in trimetrexate dosage; increase leucovorin to 40 mg/m2 every 6 hours |
|
3 |
500–749 |
25,000–49,999 |
Decrease trimetrexate dose to 22 mg/m2 once daily; increase leucovorin to 40 mg/m2 every 6 hours |
|
4 |
<500 |
<25,000 |
Day 1–9: Discontinue trimetrexate; increase leucovorin to 40 mg/m2 every 6 hours for an additional 72 hours Day 10–21: Discontinue trimetrexate; increase leucovorin to 40 mg/m2 every 6 hours for an additional 72 hours. If hematologic toxicity improves within 96 hours to grade 3 or grade 2, reinitiate trimetrexate at 22 mg/m2 or 45 mg/m2, respectively, once daily; continue leucovorin for 72 hours after the last trimetrexate dose |
Megaloblastic Anemia
IM
Up to 1 mg daily; no evidence that doses >1 mg daily are more effective.
Duration of therapy depends on hematologic response. In general, improved sense of well-being occurs within first 24 hours; bone marrow begins to become normoblastic within 48 hours; and reticulocytosis begins within 2–5 days after initiation of therapy.
Colorectal Cancer
IV
Leucovorin 20 mg/m2 followed by IV fluorouracil (425 mg/m2) daily for 5 days or leucovorin 200 mg/m2 by slow IV injection (over a minimum of 3 minutes) followed by IV fluorouracil (370 mg/m2) daily for 5 days; no evidence of superiority of either regimen.
Repeat either regimen at 4-week intervals for 2 additional courses, then at 4- to 5-week intervals provided toxicity from the previous course has subsided.
Do not administer repeat courses until WBC >4000/mm3 and platelet count >130,000/mm3. If blood counts do not return to these levels within 2 weeks, discontinue therapy. Discontinue therapy when there is clear evidence of tumor progression. (See Patient Evaluation and Monitoring under Cautions.)
If WBC and platelet count return to >4000/mm3 and >130,000/mm3, respectively, within 2 weeks, adjust subsequent fluorouracil dosages based on severity of GI toxicity and nadir blood counts from previous course; leucovorin dosage generally not adjusted according to toxicity. (See Table 5.) If no toxicity occurred in the prior course, increase subsequent fluorouracil dosage by 10%.
Adjust dosage based on the most severe toxicity.
|
Toxicity after Prior Dose |
Fluorouracil Daily Dosage for Subsequent Course |
|---|---|
|
If moderate diarrhea and/or stomatitis or WBC nadir of 1000–1900/mm3 or Platelet nadir of 25,000–75,000/mm3 occurs |
Reduce dosage by 20% |
|
If severe diarrhea and/or stomatitis or WBC nadir of <1000/mm3 or Platelet nadir of <25,000/mm3 occurs |
Reduce dosage by 30% |
Prescribing Limits
Pediatric Patients
Oral
Administration of doses >25 mg not recommended. (See Absorption under Pharmacokinetics.)
Adults
Oral
Administration of doses >25 mg not recommended. (See Absorption under Pharmacokinetics.)
Special Populations
Patients with Delayed Methotrexate Elimination
Higher dosages and extended duration of therapy may be required if delayed methotrexate excretion is caused by third space fluid accumulation (i.e., ascites, pleural effusion), renal impairment, or inadequate hydration.
Cautions for Leucovorin
Contraindications
-
Pernicious anemia or other megaloblastic anemias secondary to lack of vitamin B12; such use may obscure diagnosis of pernicious anemia by alleviating hematologic manifestations while allowing neurologic complications to progress.
Warnings/Precautions
Warnings
Use as Antidote
Administer as soon as possible following unintentional overdosage. Delayed administration may reduce effectiveness in counteracting hematologic toxicity associated with folic acid antagonists.
Toxicity Potentiation with Concomitant Therapy
When used concomitantly with other chemotherapeutic agents (e.g., fluorouracil, methotrexate), administer only under the supervision of a qualified clinician experienced in the use of cancer chemotherapeutic agents.
Possible potentiation of fluorouracil toxicity. GI toxicities (particularly stomatitis and diarrhea) observed more frequently, and possibly more severe and prolonged, compared with fluorouracil monotherapy. Diarrhea may result in clinical deterioration, leading to death; if diarrhea occurs, monitor patients until manifestations have completely resolved. Do not initiate or continue combination therapy in patients with manifestations of GI toxicity until such manifestations have completely resolved. Increased risk of severe GI toxicity in debilitated or geriatric patients; use with extreme caution. (See Geriatric Use under Cautions.)
Concomitant use with co-trimoxazole for treatment of P. jiroveci pneumonia in HIV-infected patients associated with increased rates of treatment failure, morbidity, and mortality.
Seizures and/or syncope reported rarely, usually following concomitant therapy with fluoropyrimidines; most commonly reported in cancer patients with CNS metastases or other predisposing factors.
Sensitivity Reactions
Anaphylactoid Reactions
Anaphylactoid reactions and urticaria reported.
General Precautions
Patient Evaluation and Monitoring
Treatment of advanced colorectal cancer: When used in combination with fluorouracil, perform physical examination prior to each treatment course and appropriate radiological examination as needed; discontinue therapy when there is clear evidence of tumor progression. Monitor CBC (with differential) and platelet count prior to initiation of therapy. During first 2 courses, monitor CBC (with differential) and platelet count weekly; thereafter, monitor once each cycle at time of anticipated WBC nadir. Monitor electrolytes and liver function tests prior to each course for the first 3 courses, then prior to every other course.
Specific Populations
Pregnancy
Category C.
Lactation
Not known whether distributed into milk. Use with caution.
Pediatric Use
Possible decreased anticonvulsant effect in pediatric patients receiving anticonvulsant therapy concomitantly with large amounts of folic acid; possible increased frequency of seizures in susceptible patients. (See Interactions.)
Geriatric Use
Treatment of advanced colorectal cancer: Increased risk of severe GI toxicity when used in combination with fluorouracil. Death secondary to severe enterocolitis, diarrhea, and dehydration reported in geriatric patients receiving weekly leucovorin and fluorouracil therapy; concomitant granulocytopenia and fever observed in some patients. Use with extreme caution.
Common Adverse Effects
Leucovorin in combination with fluorouracil: leukopenia, nausea, vomiting, diarrhea, stomatitis, lethargy/malaise/fatigue, alopecia, dermatitis, anorexia.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticonvulsants (phenobarbital, phenytoin, primidone) |
Decreased anticonvulsant effect if used concomitantly with large amounts of folic acid; possible increased frequency of seizures in susceptible pediatric patients |
Use concomitantly with caution |
|
Co-trimoxazole |
Increased rates of treatment failure, morbidity, and mortality in HIV-infected patients receiving combination therapy for treatment of P. jiroveci pneumonia |
|
|
Glucarpidase |
Administration of glucarpidase 2 hours before racemic leucovorin reduces peak concentrations and exposure of leucovorin and 5-methyl-THF; similar effects expected with levoleucovorin Methotrexate concentrations measured by immunoassay within 48 hours after glucarpidase administration are unreliable |
Do not administer leucovorin within 2 hours before or after glucarpidase During first 48 hours after glucarpidase administration, administer leucovorin at same dosage administered prior to glucarpidase; beyond 48 hours, base dosage on methotrexate concentration Continue leucovorin therapy until methotrexate concentration remains below the leucovorin treatment threshold for ≥3 days |
|
Fluorouracil |
Possible potentiation of fluorouracil antineoplastic activity and toxicity |
|
|
Methotrexate, intrathecal |
Possible decreased methotrexate efficacy if used concomitantly with high doses of leucovorin |
Leucovorin Pharmacokinetics
Absorption
Bioavailability
Peak serum concentrations of leucovorin (5-formyl-THF), active metabolite (5-methyl-THF), or total reduced folates attained within several hours. (See Table 6.)
Dose studied: 25 mg
Doses studied: 15 and 25 mg
|
Route |
Leucovorin |
5-Methyl-THF |
Total Reduced Folates |
|---|---|---|---|
|
Oral |
1.2 hours |
2.4 hours |
1.72 and 2.3 hours |
|
IV |
10 minutes |
1.3 hours |
10 minutes |
|
IM |
28 minutes |
2.8 hours |
40 and 52 minutes |
Oral absorption saturable at doses >25 mg. Apparent bioavailability is 97, 75, or 37% for 25-, 50-, or 100-mg dose, respectively.
AUC of leucovorin, 5-methyl-THF, and total reduced folates is similar following IV and IM administration. AUC of total reduced folates following oral administration of 25-mg dose is 92% of that following IV administration. AUC is 8% less following IM injection in gluteal region than in deltoid region.
Distribution
Extent
THF and derivatives distributed to all body tissues; liver contains about one-half of total body folate stores.
Small amounts of 5-methyl-THF distributed into CSF.
Elimination
Metabolism
Rapidly metabolized to active metabolite 5-methyl-THF (major transport and storage form of folate in body).
Elimination Route
Excreted in urine, mainly as 10-formyl-THF and 5,10-methenyl-THF.
Urinary excretion of folate becomes approximately logarithmic at doses >1 mg.
Half-life
Oral administration: 3.5–5.7 hours.
IV or IM administration: 6.2 hours (for total reduced folates).
Stability
Storage
Oral
Tablets
15–30°C. Protect from light and moisture.
Parenteral
Injection
2–8°C. Protect from light; retain in original carton until time of use. Discard unused portion.
Powder for Injection
15–30°C. Protect from light.
Following reconstitution with sterile water for injection, use immediately and discard unused portion.
Following reconstitution with bacteriostatic water for injection, use within 7 days.
Compatibility
Parenteral
Solution CompatibilityHID
|
Compatible |
|---|
|
Dextrose 10% in sodium chloride 0.9% |
|
Dextrose 5 or 10% in water |
|
Ringer’s injection |
|
Ringer’s injection, lactated |
|
Variable |
|
Sodium chloride 0.9% |
Drug Compatibility
|
Compatible |
|---|
|
Cisplatin |
|
Cisplatin with floxuridine |
|
Floxuridine |
|
Incompatible |
|
Fluorouracil |
|
Compatible |
|---|
|
Amifostine |
|
Aztreonam |
|
Bleomycin sulfate |
|
Cefepime HCl |
|
Cisplatin |
|
Cladribine |
|
Cyclophosphamide |
|
Docetaxel |
|
Doxorubicin HCl |
|
Doxorubicin HCl liposome injection |
|
Etoposide phosphate |
|
Filgrastim |
|
Fluconazole |
|
Fluorouracil |
|
Furosemide |
|
Gemcitabine HCl |
|
Granisetron HCl |
|
Heparin sodium |
|
Linezolid |
|
Methotrexate sodium |
|
Metoclopramide HCl |
|
Mitomycin |
|
Oxaliplatin |
|
Pemetrexed disodium |
|
Piperacillin sodium–tazobactam sodium |
|
Tacrolimus |
|
Teniposide |
|
Thiotepa |
|
Vinblastine sulfate |
|
Vincristine sulfate |
|
Incompatible |
|
Amphotericin B cholesteryl sulfate complex |
|
Droperidol |
|
Foscarnet sodium |
|
Lansoprazole |
|
Sodium bicarbonate |
Actions
-
Racemic mixture of diastereoisomers of 5-formyl-THF; reduced form of folic acid. Consists of equal amounts of d- and l-isomers; l-isomer (levoleucovorin) is the pharmacologically active isomer. Does not require reduction by dihydrofolate reductase to participate in reactions utilizing folates.
-
Counteracts therapeutic and toxic effects (e.g., hematologic toxicity) of folic acid antagonists (e.g., methotrexate). No effect on other established toxicities of methotrexate resulting from drug and/or metabolite precipitation in kidneys (e.g., nephrotoxicity).
-
Enhances therapeutic and toxic effects of fluoropyrimidines (e.g., fluorouracil) by stabilizing binding of fluorouracil metabolite (fluorodeoxyridylic acid) to thymidylate synthase (enzyme responsible for DNA repair and replication), thus enhancing inhibition of this enzyme.
Advice to Patients
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
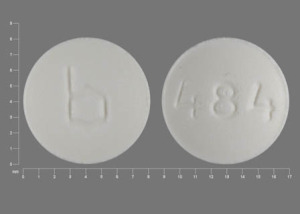
Oral |
Tablets |
5 mg (of leucovorin)* |
Leucovorin Calcium Tablets (scored) |
|
|
10 mg (of leucovorin)* |
Leucovorin Calcium Tablets (scored) |
|||
|
15 mg (of leucovorin)* |
Leucovorin Calcium Tablets (scored) |
|||
|
25 mg (of leucovorin)* |
Leucovorin Calcium Tablets (scored) |
|||
|
Parenteral |
For injection |
50 mg (of leucovorin)* |
Leucovorin Calcium for Injection |
|
|
100 mg (of leucovorin)* |
Leucovorin Calcium for Injection |
|||
|
200 mg (of leucovorin)* |
Leucovorin Calcium for Injection (preservative-free) |
|||
|
350 mg (of leucovorin)* |
Leucovorin Calcium for Injection |
|||
|
500 mg (of leucovorin)* |
Leucovorin Calcium for Injection (preservative-free) |
|||
|
Injection |
10 mg (of leucovorin) per mL (500 mg)* |
Leucovorin Calcium Injection (preservative-free) |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions January 24, 2013. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about leucovorin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: antidotes
- Breastfeeding
Patient resources
Professional resources
- Calcium Folinate Injection prescribing information
- Leucovorin Injection (FDA)
- Leucovorin Tablets (FDA)