Vandetanib (Monograph)
Brand name: Caprelsa
Drug class: Antineoplastic Agents
Warning
Risk Evaluation and Mitigation Strategy (REMS):
FDA approved a REMS for vandetanib to ensure that the benefits outweigh the risks. The REMS may apply to one or more preparations of vandetanib and consists of the following: elements to assure safe use and implementation system. See https://www.accessdata.fda.gov/scripts/cder/rems/.
Warning
- Prolongation of QT Interval, Torsades de Pointes, and Sudden Death
-
Risk of QT interval prolongation, torsades de pointes, ventricular tachycardia, and sudden death. Do not use in patients with long QT syndrome, hypocalcemia, hypokalemia, or hypomagnesemia. Correct hypocalcemia, hypokalemia, and/or hypomagnesemia before administering vandetanib.
-
Monitor serum electrolytes periodically.
-
Avoid concomitant use with drugs known to prolong QT interval.
- REMS
-
Available only through the CAPRELSA REMS Program. Only prescribers and pharmacies certified with the program can prescribe and dispense vandetanib.
Introduction
Antineoplastic agent; an inhibitor of multiple receptor tyrosine kinases.
Uses for Vandetanib
Medullary Thyroid Cancer
Treatment of symptomatic or progressive medullary thyroid cancer in patients with unresectable locally advanced or metastatic disease (designated an orphan drug by FDA for this use).
Use in patients with indolent, asymptomatic, or slowly progressing disease only after careful consideration of treatment-related risks of the drug.
Vandetanib Dosage and Administration
General
Pretreatment Screening
-
Measure ECG, serum electrolytes (i.e., calcium, magnesium, potassium), and thyroid-stimulating hormone (TSH) concentrations at baseline.
-
Verify the pregnancy status of females of reproductive potential prior to initiating treatment with vandetanib.
Patient Monitoring
-
Measure ECG, serum electrolytes (i.e., calcium, magnesium, potassium), and TSH concentrations 2–4 weeks and 8–12 weeks after initiating vandetanib, and then every 3 months thereafter.
-
Following dosage reduction for QT prolongation or therapy interruption lasting >2 weeks, monitor ECG 2–4 weeks and 8–12 weeks after resuming vandetanib, and then every 3 months thereafter.
-
If diarrhea occurs, monitor electrolytes and ECG frequently.
-
In patients with moderate renal impairment, closely monitor ECG.
-
If vandetanib is used concomitantly with a drug known to prolong the QT interval, monitor ECG more frequently.
-
Monitor for manifestations of heart failure.
-
Monitor blood pressure.
-
Perform ophthalmologic examination, including slit lamp examinations, in patients who report visual changes.
-
Adverse reactions may not resolve quickly because the drug has a long half-life. Monitor patients appropriately.
Dispensing and Administration Precautions
- Handling and Disposal
-
Consult specialized references for procedures for proper handling and disposal of antineoplastics.
-
Avoid direct contact of crushed tablets with skin or mucous membranes. If such contact occurs, wash affected area thoroughly.
REMS
-
FDA requires a Risk Evaluation and Mitigation Strategy (REMS) for vandetanib because of risk of QT interval prolongation, torsades de pointes, and sudden death.
-
Available only under a restricted distribution program (CAPRELSA REMS Program). Contact 800-817-2722 or visit [Web] for additional information and to enroll in the program for vandetanib.
Other General Considerations
-
Discontinue vandetanib ≥1 month prior to scheduled surgery. Do not resume vandetanib for ≥2 weeks following major surgery and until adequate wound healing has occurred.
-
Use sun protection during vandetanib therapy and for ≥4 months after discontinuance of the drug.
Administration
Oral Administration
Administer tablets orally once daily without regard to meals; do not crush tablets.
If a dose is missed, do not take the missed dose if it is <12 hours until the next scheduled dose.
If tablets cannot be swallowed whole, prepare dispersion by placing tablet in a glass containing 60 mL of noncarbonated water (do not use other liquids). Without crushing the tablet, stir water for approximately 10 minutes until tablet is dispersed; tablet will not completely dissolve. Swallow aqueous dispersion immediately; to ensure full dose is administered, mix any residue in the glass with an additional 120 mL of noncarbonated water and swallow.
Avoid direct contact of crushed tablets with skin or mucous membranes. If such contact occurs, wash affected area thoroughly.
NG or Gastrostomy Tube
May administer aqueous dispersion through a nasogastric or gastrostomy tube.
Dosage
Adults
Medullary Thyroid Cancer
Oral
300 mg once daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Dosage Modification for Toxicity
Oral
If grade 3 or greater toxicity occurs, interrupt vandetanib therapy. When toxicity resolves or improves to grade 1, resume at a reduced dosage. Adjust dosage in decrements of 100 mg daily (i.e., from 300 to 200 mg daily, from 200 to 100 mg daily).
Dosage Modification for Cardiovascular Toxicity
OralIf QTcF interval >500 msec, interrupt vandetanib therapy. When QTcF returns to <450 msec, resume vandetanib at a reduced dosage.
If hypertension occurs, may need to reduce dosage or interrupt therapy to control BP. If hypertension cannot be controlled, do not resume.
Dosage Modification for Dermatologic Toxicity
OralIf severe skin reactions occur, permanently discontinue vandetanib therapy and refer patient for urgent medical evaluation. Systemic therapy (e.g., corticosteroids) may be required.
Dosage Modification for Diarrhea
OralIf severe diarrhea occurs, interrupt vandetanib therapy. When diarrhea improves, resume at a reduced dosage.
Special Populations
Hepatic Impairment
Do not use in patients with moderate (Child-Pugh class B) or severe (Child-Pugh class C) hepatic impairment.
Renal Impairment
Reduce initial dosage to 200 mg once daily in patients with moderate (Clcr of 30–49 mL/minute) renal impairment.
Not recommended for use in patients with severe (Clcr <30 mL/minute) renal impairment.
Use in patients with end-stage renal disease requiring dialysis: not evaluated.
Geriatric Patients
Manufacturer makes no specific dosage recommendations in patients ≥65 years of age.
Related/similar drugs
doxorubicin, Armour Thyroid, NP Thyroid, Lenvima, cabozantinib, lenvatinib
Cautions for Vandetanib
Contraindications
-
Congenital long QT syndrome.
Warnings/Precautions
Warnings
Prolongation of QT Interval and Torsades de Pointes
QT interval prolongation, torsades de pointes, ventricular tachycardia, and sudden death reported (see Boxed Warning).
Do not initiate vandetanib therapy in patients with QTcF interval >450 msec. Do not use in patients with a history of torsades de pointes, congenital long QT syndrome, bradyarrhythmias, uncompensated heart failure, or in patients with electrolyte disturbances; correct hypocalcemia, hypokalemia, and/or hypomagnesemia before administering.
Monitor ECG, serum electrolytes (i.e., calcium, magnesium, potassium), and TSH concentrations at baseline, at 2–4 weeks and 8–12 weeks after initiating vandetanib, and then every 3 months thereafter. Following dosage reduction for QT interval prolongation or therapy interruption lasting >2 weeks, monitor ECG as described above. Maintain serum potassium concentrations at ≥4 mEq/L (within normal range) and serum magnesium and calcium concentrations within normal range.
Vandetanib exposure is increased in patients with impaired renal function. Reduce initial vandetanib dosage to 200 mg in patients with moderate renal impairment and monitor QT interval frequently.
Monitor electrolytes and ECG more frequently in patients who experience diarrhea.
Avoid concomitant use with drugs known to prolong QT interval. If concomitant use cannot be avoided, monitor ECG more frequently.
If QTcF interval >500 msec, interrupt vandetanib therapy. When QTcF interval returns to <450 msec, resume at a reduced dosage.
Sensitivity Reactions
Photosensitivity Reactions
Risk of photosensitivity reactions during treatment and for up to 4 months after final dose. In patients receiving vandetanib for malignancies other than medullary thyroid cancer (i.e., non-small cell lung cancer, hepatocellular carcinoma, brain tumor), photosensitivity reactions (including hyperpigmentation and erythematous edematous lesions) occurred within 3 weeks to 2 months after initiating the drug.
Other Warnings and Precautions
Dermatologic Effects
Severe, sometimes fatal, skin reactions (including toxic epidermal necrolysis [TEN] and Stevens-Johnson syndrome) reported.
If severe skin reactions occur, permanently discontinue vandetanib and refer patient for urgent medical evaluation. Systemic therapy (e.g., corticosteroids) may be required.
Pulmonary Effects
Interstitial lung disease or pneumonitis, sometimes fatal, reported.
Consider possible interstitial lung disease in patients presenting with nonspecific respiratory signs or symptoms.
In case of acute or worsening pulmonary symptoms, temporarily interrupt vandetanib therapy.
If interstitial lung disease is confirmed, discontinue vandetanib.
Cerebrovascular Events
Ischemic cerebrovascular events reported. Discontinue vandetanib in patients who experience a severe ischemic cerebrovascular event. Safety of resuming vandetanib therapy after resolution of an ischemic cerebrovascular event not studied.
Hemorrhage
Serious, sometimes fatal, hemorrhagic events reported. Do not use in patients with a recent history of hemoptysis (≥2.5 mL of red blood). Discontinue in patients with severe hemorrhage.
Cardiovascular Effects
Heart failure reported; monitor for manifestations. If heart failure occurs, may need to discontinue vandetanib; heart failure may not be reversible following discontinuance.
Hypertension and hypertensive crisis reported. Monitor and control BP in all patients as appropriate. May need to reduce dosage or interrupt vandetanib therapy. If hypertension cannot be controlled, do not resume vandetanib.
Diarrhea
Diarrhea occurs frequently. Routine use of antidiarrheal drugs recommended.
Monitor serum electrolytes and ECG carefully and more frequently in patients with diarrhea.
If severe diarrhea occurs, interrupt vandetanib therapy. When symptoms improve, resume at a reduced dosage.
Hypothyroidism
Increases in dosages of thyroid replacement therapy were required in 49% of patients in a phase 3 clinical study.
Monitor TSH concentrations at baseline, at 2–4 weeks and 8–12 weeks after initiating vandetanib, and then every 3 months thereafter.
If manifestations of hypothyroidism occur, determine thyroid hormone concentrations and adjust thyroid replacement therapy accordingly.
Reversible Posterior Leukoencephalopathy Syndrome
Reversible posterior leukoencephalopathy syndrome (RPLS) reported.
Consider possible RPLS in patients presenting with seizures, headache, visual disturbances, confusion, or altered mental function.
If RPLS occurs, discontinue vandetanib.
Renal Failure
Renal failure reported; withhold, reduce, or permanently discontinue vandetanib therapy based on severity.
Reduce the starting dose of vandetanib in moderate renal impairment. Notrecommended for use in severe renal impairment.
Impaired Wound Healing
Potential risk of impaired wound healing in patients receiving drugs that inhibit the VEGF signaling pathway, including vandetanib.
The manufacturer recommends that vandetanib be discontinued ≥1 month prior to scheduled surgery. Do not administer vandetanib for at least 2 weeks following major surgery and until adequate wound healing has occurred.
Safety of resuming vandetanib after resolution of wound healing complications not established.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm. Embryotoxic, fetotoxic, and teratogenic in animals.
Advise females of reproductive potential to use effective contraception during treatment with vandetanib and for ≥ 4 months following the last dose. If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.
Ocular Effects
Blurred vision and corneal opacities (which can lead to halos and decreased visual acuity) reported. Not known if corneal opacities will improve after discontinuance of vandetanib.
If visual changes occur, ophthalmologic evaluation, including slit lamp examination, recommended.
Specific Populations
Pregnancy
Based on its mechanism of action, may cause fetal harm. Embryotoxic, fetotoxic, and teratogenic at clinically relevant exposures in rats; adverse effects on female fertility, embryofetal development, and postnatal development of pups also observed.
Advise females of reproductive potential of the potential hazard to a fetus. Advise females of reproductive potential to use effective contraception during treatment with vandetanib and for ≥4 months following the last dose.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Advise females not to breast-feed during vandetanib therapy and for ≥4 months after the final dose.
Females and Males of Reproductive Potential
Verify the pregnancy status of females of reproductive potential prior to initiating treatment with vandetanib. Advise females of reproductive potential to use effective contraception during treatment with vandetanib and for 4 months after the final dose.
No data on the effects of vandetanib on human fertility. Based on animal studies, may impair male and female fertility.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Geriatric Use
Insufficient numbers of patients ≥65 years of age included in studies to determine whether they respond differently compared with younger adults.
Hepatic Impairment
Safety and efficacy not established in patients with moderate (Child-Pugh class B) or severe (Child-Pugh class C) hepatic impairment; use not recommended in these patients.
Renal Impairment
A lower initial dosage is recommended in patients with moderate (Clcr of 30–49 mL/minute) renal impairment. Monitor ECG closely. Not recommended for use in patients with severe (Clcr <29 mL/minute) renal impairment.
Not evaluated systematically in patients with end-stage renal disease requiring dialysis.
Common Adverse Effects
Adverse effects (reported in >20% of patients): Diarrhea/colitis, rash, acneiform dermatitis, hypertension, nausea, headache, upper respiratory tract infections, decreased appetite, abdominal pain, hypocalcemia, increased ALT concentrations, hypoglycemia.
Drug Interactions
Metabolized partially by CYP3A4.
Drugs Affecting Hepatic Microsomal Enzymes
Potent inhibitors of CYP3A4: No clinically important interaction.
Potent inducers of CYP3A4: Potential decreased plasma vandetanib concentrations.
Drugs that Prolong QT Interval
Potential additive effect on QT interval prolongation. Avoid concomitant use. If concomitant use cannot be avoided, monitor ECG more frequently.
Drugs Affecting OCT2
Possible increase in concentrations of drugs that are transported by the organic cation transporter type 2 (OCT2). Use caution and closely monitor for toxicities when vandetanib is used concomitantly with drugs that are transported by OCT2.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antiarrhythmic agents, class Ia and III (e.g., amiodarone, disopyramide, dofetilide, procainamide, quinidine, sotalol) |
Possible additive effect on QT interval prolongation |
Avoid concomitant use; if concomitant use cannot be avoided, monitor ECG more frequently |
|
Anticonvulsants (carbamazepine, phenobarbital, phenytoin) |
Possible decrease in plasma vandetanib concentrations |
Avoid concomitant use |
|
Antiemetic agents that prolong QT interval, type 3 serotonin (5-HT3) receptor antagonists (e.g., dolasetron, granisetron, ondansetron) |
Possible additive effect on QT interval prolongation |
Avoid concomitant use; if concomitant use is necessary, granisetron preferred by some clinicians because of less pronounced effects on ECG intervals compared with dolasetron or ondansetron Monitor ECG more frequently during concomitant use |
|
Antimycobacterials (rifabutin, rifampin, rifapentine) |
Possible decrease in plasma vandetanib concentrations |
Avoid concomitant use |
|
Antipsychotic agents that prolong QT interval (e.g., asenapine, chlorpromazine, haloperidol, olanzapine, paliperidone, pimozide, quetiapine, thioridazine, ziprasidone) |
Possible additive effect on QT interval prolongation |
Avoid concomitant use; if concomitant use cannot be avoided, monitor ECG more frequently |
|
Chloroquine |
Possible additive effect on QT interval prolongation |
Avoid concomitant use; if concomitant use cannot be avoided, monitor ECG more frequently |
|
Clarithromycin |
Possible additive effect on QT interval prolongation |
Avoid concomitant use; if concomitant use cannot be avoided, monitor ECG more frequently |
|
Dexamethasone |
Possible decrease in plasma vandetanib concentrations |
Avoid concomitant use |
|
Digoxin |
Possible increase in plasma digoxin concentrations |
Use concomitantly with caution and closely monitor for digoxin toxicity |
|
Gatifloxacin |
Possible additive effect on QT interval prolongation |
Avoid concomitant use; if concomitant use cannot be avoided, monitor ECG more frequently |
|
Itraconazole |
Pharmacokinetic interaction unlikely |
|
|
Metformin |
Possible increase in plasma metformin concentrations |
Use concomitantly with caution and closely monitor for metformin toxicity |
|
Methadone |
Possible additive effect on QT interval prolongation |
Avoid concomitant use; if concomitant use cannot be avoided, monitor ECG more frequently |
|
Midazolam |
No clinically important effects on pharmacokinetics of midazolam (CYP 3A4 substrate) |
|
|
Moxifloxacin |
Possible additive effect on QT interval prolongation |
Avoid concomitant use; if concomitant use cannot be avoided, monitor ECG more frequently |
|
Omeprazole |
Pharmacokinetic interaction unlikely |
|
|
Ranitidine |
Pharmacokinetic interaction unlikely |
|
|
St. John’s wort (Hypericum perforatum) |
Possible unpredictable decreases in plasma vandetanib concentrations |
Avoid concomitant use |
|
Tetrabenazine |
Possible additive effect on QT interval prolongation |
Avoid concomitant use; if concomitant use cannot be avoided, monitor ECG more frequently |
Vandetanib Pharmacokinetics
Absorption
Bioavailability
Following oral administration, peak plasma concentrations are attained within 4–10 hours.
Steady-state concentrations achieved after approximately 3 months.
Food
Food has no effect on exposure.
Special Populations
Following administration of a single 800-mg dose, AUC was comparable between individuals with mild (Child-Pugh class A), moderate (Child-Pugh class B), or severe (Child-Pugh class C) hepatic impairment and individuals with normal hepatic function.
Following administration of a single 800-mg dose, mean AUC was comparable between individuals with mild renal impairment and individuals with normal renal function; however, in individuals with moderate or severe renal impairment, mean AUC of vandetanib was increased by 39 or 41%, respectively, compared with individuals with normal renal function.
Higher systemic exposure in Japanese and Chinese patients compared with Caucasian patients receiving the same dose.
Pharmacokinetics not evaluated in pediatric patients.
Distribution
Extent
Not known whether vandetanib is distributed into human milk.
Plasma Protein Binding
90–94% (mainly albumin and α1-acid glycoprotein).
Elimination
Metabolism
Metabolized by CYP3A4 and by flavin-containing monooxygenase enzymes FM01 and FM03 to N-desmethyl-vandetanib and vandetanib-N-oxide, respectively.
Elimination Route
Eliminated in feces (63%) and urine (25%) as unchanged drug or metabolites.
Half-life
Median terminal half-life: 19 days.
Special Populations
No relationship between clearance and age or sex.
Following administration of a single 800-mg dose, mean clearance was comparable between individuals with mild, moderate, or severe hepatic impairment and individuals with normal hepatic function.
Following administration of a single 800-mg dose, mean clearance was comparable between individuals with mild renal impairment and individuals with normal renal function.
Stability
Storage
Oral
Tablets
25°C (excursions permitted between 15–30°C).
Actions
-
Inhibits multiple receptor tyrosine kinases (RTKs), which are involved in the initiation of various cascades of intracellular signaling events that lead to cell proliferation and/or influence processes critical to cell survival and tumor progression (e.g., angiogenesis, metastasis, inhibition of apoptosis).
-
Various tyrosine kinases and pathways are abnormally activated in medullary thyroid carcinoma cells (e.g., rearranged during transfection [RET] proto-oncogene signaling is associated with development of hereditary medullary thyroid cancer).
-
In vitro, shown to inhibit activity of multiple receptor tyrosine kinases, including vascular endothelial growth factor receptors (i.e., VEGFR-1, VEGFR-2, VEGFR-3), members of the epidermal growth factor receptor (EGFR) family, RET, protein tyrosine kinase 6 (BRK), TIE2, members of the EPH receptor kinase family, and members of the Src family of tyrosine kinases.
-
The N-desmethyl metabolite of the drug, which represents 7 to 17.1% of vandetanib exposure, has similar inhibitory activity to the parent compound for VEGF receptors (KDR and Flt-1) and EGFR.
-
In vivo, shown to reduce tumor cell-induced angiogenesis and tumor vessel permeability; also shown to inhibit tumor growth and metastasis in mouse models of cancer.
Advice to Patients
-
A copy of the manufacturer’s patient information (medication guide) for vandetanib must be provided to all patients with each prescription of the drug. Advise patients to read the medication guide prior to initiation of therapy and each time the prescription is refilled.
-
Importance of not crushing vandetanib tablets. Avoid direct contact of crushed tablets with the skin or mucous membranes.
-
If a dose is missed, do not take the missed dose if it is <12 hours before the next dose.
-
Risk of QT interval prolongation, torsades de pointes, ventricular tachycardia, and sudden death. Importance of regular monitoring of ECG and serum electrolytes. Contact clinician promptly if feelings of lightheadedness or faintness or an irregular heartbeat occurs.
-
Risk of photosensitivity/phototoxicity reactions. Use sunscreen and protective clothing and limit sun exposure during therapy and for at least 4 months after discontinuance of the drug.
-
Risk of severe adverse dermatologic effects. Contact clinician promptly if dermatologic manifestations (e.g., rash; acne; dry skin; itching; blisters on skin or in mouth; peeling; fever; muscle or joint aches; redness or swelling of face, hands, or soles of feet) occur.
-
Risk of interstitial lung disease. Promptly report new or worsening respiratory manifestations (e.g., shortness of breath, persistent cough, fever).
-
Risk of diarrhea. Contact clinician if diarrhea occurs.
-
Risk of RPLS. Contact clinician promptly if seizures, headache, visual disturbances, confusion, or difficulty thinking occurs.
-
Risk of impaired wound healing. Inform clinician of any planned surgical procedure.
-
Advise females of reproductive potential to use an effective method of contraception while receiving vandetanib and for at least 4 months after discontinuance. Advise females to contact their clinician if they become pregnant, or if pregnancy is suspected, during treatment with vandetanib. Discontinue nursing while receiving vandetanib therapy and for at least 4 months after the final dose.
-
Risk of blurred vision. Avoid driving a vehicle or operating machinery if blurred vision occurs.
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements, as well as any concomitant illnesses (e.g., hepatic or renal impairment, cardiovascular disease).
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Distribution of vandetanib is restricted. Contact 800-817-2722 or visit [Web] for specific availability information.
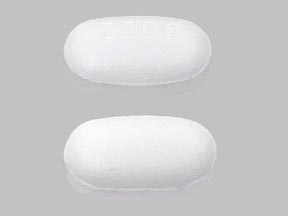
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
100 mg |
Caprelsa |
Genzyme Corporation |
|
300 mg |
Caprelsa |
Genzyme Corporation |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions March 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about vandetanib
- Check interactions
- Compare alternatives
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: EGFR inhibitors
- Breastfeeding
- En español