Telithromycin
Medically reviewed by Drugs.com. Last updated on Nov 20, 2023.
Pronunciation
(tel ith roe MYE sin)
Index Terms
- HMR 3647
Pharmacologic Category
- Antibiotic, Ketolide
Pharmacology
Inhibits bacterial protein synthesis by binding to two sites on the 50S ribosomal subunit. Telithromycin has also been demonstrated to alter secretion of IL-1alpha and TNF-alpha; the clinical significance of this immunomodulatory effect has not been evaluated.
Absorption
Rapid
Distribution
2.9 L/kg
Metabolism
Hepatic, via CYP3A4 (50%) and non-CYP-mediated pathways
Excretion
Urine (13% unchanged drug, remainder as metabolites); feces (7% unchanged drug)
Time to Peak
Plasma: 1 hour
Half-Life Elimination
10 hours
Protein Binding
60% to 70%; primarily to albumin
Use: Labeled Indications
Community-acquired pneumonia: Treatment of mild to moderate community-acquired pneumonia (CAP) due to Streptococcus pneumoniae (including multidrug-resistant isolates), Haemophilus influenzae, Moraxella catarrhalis, Chlamydophila (also known as Chlamydia) pneumoniae, or Mycoplasma pneumoniae in patients 18 years and older.
Contraindications
Hypersensitivity to telithromycin, macrolide antibiotics, or any component of the formulation; myasthenia gravis; history of hepatitis and/or jaundice associated with telithromycin or other macrolide antibiotic use; concurrent use of colchicine (if patient has concomitant renal or hepatic impairment), cisapride, pimozide, lovastatin, or simvastatin
Dosing: Adult
Note: Ketek has been discontinued in the United States for more than 1 year.
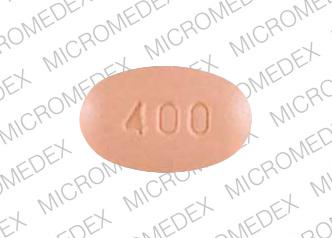
Community-acquired pneumonia (CAP): Oral: 800 mg once daily for 7-10 days
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Related/similar drugs
prednisone, amoxicillin, doxycycline, azithromycin, ciprofloxacin, metronidazole, clindamycin
Dosing: Geriatric
Refer to adult dosing.
Administration
Oral: May be administered with or without food.
Storage
Store at 15°C to 30°C (59°F to 86°F).
Drug Interactions
Abametapir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Abemaciclib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Abemaciclib. Management: In patients taking abemaciclib at a dose of 200 mg or 150 mg twice daily, reduce the dose to 100 mg twice daily when combined with strong CYP3A4 inhibitors. In patients taking abemaciclib 100 mg twice daily, decrease the dose to 50 mg twice daily. Consider therapy modification
Acalabrutinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Acalabrutinib. Avoid combination
Ado-Trastuzumab Emtansine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Ado-Trastuzumab Emtansine. Specifically, strong CYP3A4 inhibitors may increase concentrations of the cytotoxic DM1 component. Management: Avoid concomitant use of ado-trastuzumab emtansine and strong CYP3A4 inhibitors when possible. Consider alternatives that do not inhibit CYP3A4 or consider administering after CYP3A4 inhibitor discontinuation. Monitor for toxicities if combined. Consider therapy modification
Alfentanil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Alfentanil. Management: If use of alfentanil and strong CYP3A4 inhibitors is necessary, consider dosage reduction of alfentanil until stable drug effects are achieved. Frequently monitor patients for respiratory depression and sedation when these agents are combined. Consider therapy modification
Alfuzosin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Alfuzosin. Avoid combination
Alitretinoin (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Alitretinoin (Systemic). Management: Consider reducing the alitretinoin dose to 10 mg when used together with strong CYP3A4 inhibitors. Monitor for increased alitretinoin effects/toxicities if combined with a strong CYP3A4 inhibitor. Consider therapy modification
Almotriptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Almotriptan. Management: Limit initial almotriptan dose to 6.25 mg and maximum dose to 12.5 mg in any 24-period when used with a strong CYP3A4 inhibitor. Avoid concurrent use in patients with impaired hepatic or renal function. Consider therapy modification
Alosetron: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Alosetron. Monitor therapy
ALPRAZolam: CYP3A4 Inhibitors (Strong) may increase the serum concentration of ALPRAZolam. Management: Consider using an alternative agent that is less likely to interact. If combined, monitor for increased therapeutic/toxic effects of alprazolam if combined with a strong CYP3A4 inhibitor. Consider therapy modification
Apixaban: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Apixaban. Monitor therapy
Aprepitant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Aprepitant. Avoid combination
ARIPiprazole: CYP3A4 Inhibitors (Strong) may increase the serum concentration of ARIPiprazole. Management: Aripiprazole dose reductions are required for indications other than major depressive disorder. Dose reductions vary based on formulation, CYP2D6 genotype, and use of CYP2D6 inhibitors. See full interaction monograph for details. Consider therapy modification
ARIPiprazole Lauroxil: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of ARIPiprazole Lauroxil. Management: Decrease aripiprazole lauroxil dose to next lower strength if used with strong CYP3A4 inhibitors for over 14 days. No dose adjustment needed if using the lowest dose (441 mg). Max dose is 441 mg in CYP2D6 PMs or if also taking strong CYP2D6 inhibitors. Consider therapy modification
Astemizole: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Astemizole. Avoid combination
Asunaprevir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Asunaprevir. Avoid combination
AtorvaSTATin: Telithromycin may increase the serum concentration of AtorvaSTATin. Management: Consider limiting atorvastatin to a max (adult) dose of 20 mg/day when used with telithromycin. Although not a specific recommendation in atorvastatin labeling, this is consistent with dosing for other strong CYP3A4 inhibitors, including clarithromycin. Consider therapy modification
Avanafil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Avanafil. Avoid combination
Avapritinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Avapritinib. Avoid combination
Axitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Axitinib. Management: Avoid concurrent use of axitinib with any strong CYP3A inhibitor whenever possible. If a strong CYP3A inhibitor must be used with axitinib, a 50% axitinib dose reduction is recommended. Consider therapy modification
Barnidipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Barnidipine. Avoid combination
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Bedaquiline: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bedaquiline. Management: Limit duration of concurrent use of bedaquiline with CYP3A4 inhibitors to no more than 14 days, unless the benefit of continued use outweighs the possible risks. Monitor for toxic effects of bedaquiline. Consider therapy modification
Benperidol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Benperidol. Monitor therapy
Benzhydrocodone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Benzhydrocodone. Specifically, the concentration of hydrocodone may be increased. Monitor therapy
Betamethasone (Ophthalmic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Betamethasone (Ophthalmic). Monitor therapy
Betamethasone (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Betamethasone (Systemic). Monitor therapy
Bictegravir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bictegravir. Monitor therapy
Blonanserin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Blonanserin. Avoid combination
Bortezomib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bortezomib. Monitor therapy
Bosentan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bosentan. Monitor therapy
Bosutinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bosutinib. Avoid combination
Brentuximab Vedotin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Brexpiprazole: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Brexpiprazole. Management: Reduce brexpiprazole dose 50% with strong CYP3A4 inhibitors; reduce to 25% of usual if used with both a strong CYP3A4 inhibitor and a CYP2D6 inhibitor in patients not being treated for MDD, or strong CYP3A4 inhibitor used in a CYP2D6 poor metabolizer. Consider therapy modification
Brigatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Brigatinib. Management: Avoid concurrent use of brigatinib with strong CYP3A4 inhibitors when possible. If combination cannot be avoided, reduce the brigatinib dose by approximately 50%, rounding to the nearest tablet strength (ie, from 180 mg to 90 mg, or from 90 mg to 60 mg). Consider therapy modification
Bromperidol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bromperidol. Monitor therapy
Budesonide (Nasal): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Nasal). Monitor therapy
Budesonide (Oral Inhalation): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Oral Inhalation). Monitor therapy
Budesonide (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Systemic). Management: Avoid the concomitant use of CYP3A4 inhibitors and oral budesonide. If patients receive both budesonide and a strong CYP3A4 inhibitor, they should be closely monitored for signs and symptoms of corticosteroid excess. Consider therapy modification
Budesonide (Topical): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Topical). Avoid combination
Buprenorphine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Buprenorphine. Monitor therapy
BusPIRone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of BusPIRone. Management: Limit the buspirone dose to 2.5 mg daily and monitor patients for increased buspirone effects/toxicities if combined with strong CYP3A4 inhibitors. Consider therapy modification
Cabazitaxel: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cabazitaxel. Management: Concurrent use of cabazitaxel with strong inhibitors of CYP3A4 should be avoided when possible. If such a combination must be used, consider a 25% reduction in the cabazitaxel dose. Consider therapy modification
Cabozantinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cabozantinib. Management: Avoid use of a strong CYP3A4 inhibitor with cabozantinib if possible. If combined, decrease cabozantinib capsules (Cometriq) by 40 mg from previous dose or decrease cabozantinib tablets (Cabometyx) by 20 mg from previous dose. Consider therapy modification
Calcifediol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Calcifediol. Monitor therapy
Calcium Channel Blockers: Macrolide Antibiotics may decrease the metabolism of Calcium Channel Blockers. Management: Consider using a noninteracting macrolide. Felodipine Canadian labeling specifically recommends avoiding its use in combination with clarithromycin. Consider therapy modification
Cannabidiol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cannabidiol. Monitor therapy
Cannabis: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cannabis. More specifically, tetrahydrocannabinol and cannabidiol serum concentrations may be increased. Monitor therapy
Capmatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Capmatinib. Monitor therapy
Cardiac Glycosides: Macrolide Antibiotics may increase the serum concentration of Cardiac Glycosides. Monitor therapy
Cariprazine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cariprazine. Management: Decrease cariprazine dose 50% (4.5 mg to 1.5 mg or 3 mg; 1.5 mg to 1.5 mg every other day) if starting a strong CYP3A4 inhibitor. If on a strong CYP3A4 inhibitor, start cariprazine at 1.5 mg day 1, 0 mg day 2, then 1.5 mg daily. May increase to 3 mg daily Consider therapy modification
Ceritinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ceritinib. Management: If such combinations cannot be avoided, the ceritinib dose should be reduced by approximately one-third (to the nearest 150 mg). Resume the prior ceritinib dose after cessation of the strong CYP3A4 inhibitor. Consider therapy modification
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Ciclesonide (Oral Inhalation): CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Ciclesonide (Oral Inhalation). Monitor therapy
Cilostazol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cilostazol. Management: Consider reducing the cilostazol dose to 50 mg twice daily in adult patients who are also receiving strong inhibitors of CYP3A4. Consider therapy modification
Cinacalcet: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cinacalcet. Monitor therapy
Cisapride: Telithromycin may increase the serum concentration of Cisapride. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CloZAPine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of CloZAPine. Monitor therapy
Cobicistat: Telithromycin may increase the serum concentration of Cobicistat. Cobicistat may increase the serum concentration of Telithromycin. Management: Consider alternatives to telithromycin in patients receiving cobicistat-containing products. If concomitant therapy is required, monitor patients for evidence of telithromycin toxicity, including QT interval prolongation. Consider therapy modification
Cobimetinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cobimetinib. Avoid combination
Codeine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
Colchicine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Colchicine. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a strong CYP3A4 inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See interaction monograph for details. Consider therapy modification
Conivaptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Conivaptan. Avoid combination
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Copanlisib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Copanlisib. Management: If concomitant use of copanlisib and strong CYP3A4 inhibitors cannot be avoided, reduce the copanlisib dose to 45 mg. Monitor patients for increased copanlisib effects/toxicities. Consider therapy modification
Cortisone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cortisone. Monitor therapy
Crizotinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Crizotinib. Management: Avoid concomitant use of crizotinib and strong CYP3A4 inhibitors whenever possible. If combined use cannot be avoided, decrease the crizotinib dose to 250 mg daily. Consider therapy modification
CycloSPORINE (Systemic): Telithromycin may increase the serum concentration of CycloSPORINE (Systemic). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Telithromycin. Avoid combination
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Telithromycin. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Telithromycin. Monitor therapy
CYP3A4 Substrates (High risk with Inhibitors): CYP3A4 Inhibitors (Strong) may decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Management: Consider avoiding this combination. Some combinations are specifically contraindicated by manufacturers; others may have recommended dose adjustments. If combined, monitor for increased substrate effects. Consider therapy modification
Dabrafenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dabrafenib. Avoid combination
Daclatasvir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Daclatasvir. Management: Decrease the daclatasvir dose to 30 mg once daily if combined with a strong CYP3A4 inhibitor. No dose adjustment is needed when daclatasvir is used with darunavir/cobicistat. Consider therapy modification
Dapoxetine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dapoxetine. Avoid combination
Darifenacin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Darifenacin. Management: Limit the darifenacin dose to no more than 7.5 mg daily if combined with strong CYP3A4 inhibitors. Monitor patients for increased darifenacin toxicities (eg, dry mouth, constipation, headache, CNS effects) when these agents are combined. Consider therapy modification
Dasatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dasatinib. Management: This combination should be avoided if possible. If combined, decrease dasatinib dose from 140 mg to 40 mg, 100 mg to 20 mg, or 70 mg to 20 mg. For patients taking 60 mg or 40 mg daily, stop dasatinib until the CYP3A4 inhibitor is discontinued. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deflazacort: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Deflazacort. Management: Administer one third of the recommended deflazacort dose when used together with a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Delamanid: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Delamanid. Management: Increase ECG monitoring frequency if delamanid is combined with strong CYP3A4 inhibitors due to the risk for QTc interval prolongation. Continue frequent ECG assessments throughout full delamanid treatment period. Consider therapy modification
DexAMETHasone (Ophthalmic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of DexAMETHasone (Ophthalmic). Monitor therapy
Dienogest: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dienogest. Monitor therapy
Disopyramide: Telithromycin may enhance the QTc-prolonging effect of Disopyramide. Telithromycin may increase the serum concentration of Disopyramide. Avoid combination
DOCEtaxel: CYP3A4 Inhibitors (Strong) may increase the serum concentration of DOCEtaxel. Management: Avoid the concomitant use of docetaxel and strong CYP3A4 inhibitors when possible. If combined use is unavoidable, consider a 50% docetaxel dose reduction and monitor for increased docetaxel toxicities. Consider therapy modification
Dofetilide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dofetilide. Monitor therapy
Domperidone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Domperidone. Avoid combination
Doxercalciferol: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Doxercalciferol. Monitor therapy
DOXOrubicin (Conventional): CYP3A4 Inhibitors (Strong) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to strong CYP3A4 inhibitors in patients treated with doxorubicin whenever possible. Prescribing information for at least one doxorubicin product recommends that these combinations be avoided. Consider therapy modification
Dronabinol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dronabinol. Monitor therapy
Dronedarone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dronedarone. Management: Concurrent use of strong CYP3A4 inhibitors with dronedarone is contraindicated according to dronedarone prescribing information. Avoid combination
Drospirenone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Drospirenone. Management: Drospirenone use is contraindicated specifically when the strong CYP3A4 inhibitors atazanavir and cobicistat are administered concurrently. Caution should be used when drospirenone is coadministered with other strong CYP3A4 inhibitors. Consider therapy modification
Dutasteride: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dutasteride. Monitor therapy
Duvelisib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Duvelisib. Management: Reduce the dose of duvelisib to 15 mg twice a day when used together with a strong CYP3A4 inhibitor. Monitor closely for evidence of altered response to treatment. Consider therapy modification
Elagolix: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Elagolix. Management: Use of the elagolix 200 mg twice daily dose with a strong CYP3A4 inhibitor for longer than 1 month is not recommended. Limit combined use of the elagolix 150 mg once daily dose with a strong CYP3A4 inhibitor to a maximum of 6 months. Consider therapy modification
Elagolix, Estradiol, and Norethindrone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Elagolix, Estradiol, and Norethindrone. Avoid combination
Eletriptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Eletriptan. Avoid combination
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Management: When combined with strong CYP3A4 inhibitors, administer two elexacaftor/tezacaftor/ivacaftor tablets (100 mg/50 mg/75 mg) in the morning, twice a week, approximately 3 to 4 days apart. No evening doses of ivacaftor (150 mg) alone should be administered. Consider therapy modification
Eliglustat: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Eliglustat. Management: Reduce eliglustat dose to 84 mg daily in CYP2D6 EMs when used with strong CYP3A4 inhibitors. Use of strong CYP3A4 inhibitors is contraindicated in CYP2D6 IMs, PMs, or in CYP2D6 EMs who are also taking strong or moderate CYP2D6 inhibitors. Consider therapy modification
Encorafenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Encorafenib. Management: Avoid use of encorafenib and strong CYP3A4 inhibitors when possible. If combined, decrease encorafenib from 450 mg to 150 mg; or from 300 mg, 225 mg, or 150 mg to 75 mg. Once the CYP3A4 inhibitor is discontinued for 3 to 5 half-lives, resume prior dose. Consider therapy modification
Enfortumab Vedotin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Enfortumab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Entrectinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Entrectinib. Management: Avoid strong CYP3A4 inhibitors during treatment with entrectinib when possible. If combined in adults and those 12 yrs of age or older with a BSA of at least 1.5 square meters, reduce dose to 100 mg/day. Avoid if BSA is less than 1.5 square meters. Consider therapy modification
Eplerenone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Eplerenone. Avoid combination
Erdafitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Erdafitinib. Management: Avoid concomitant use of erdafitinib and strong CYP3A4 inhibitors when possible. If combined, monitor closely for erdafitinib adverse reactions and consider dose modifications accordingly. Consider therapy modification
Ergot Derivatives: Macrolide Antibiotics may increase the serum concentration of Ergot Derivatives. Cabergoline and Clarithromycin may interact, see specific monograph for full details. Avoid combination
Erlotinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Erlotinib. Management: Avoid use of this combination when possible. When the combination must be used, monitor the patient closely for the development of severe adverse reactions, and if such severe reactions occur, reduce the erlotinib dose (in 50 mg decrements). Consider therapy modification
Estrogen Derivatives: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Estrogen Derivatives. Monitor therapy
Eszopiclone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Eszopiclone. Management: Limit the eszopiclone dose to 2 mg daily when combined with strong CYP3A4 inhibitors and monitor for increased eszopiclone effects and toxicities (eg, somnolence, drowsiness, CNS depression). Consider therapy modification
Etizolam: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Etizolam. Management: Consider use of lower etizolam doses when using this combination; specific recommendations concerning dose adjustment are not available. Monitor clinical response to the combination closely. Consider therapy modification
Everolimus: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Everolimus. Management: Consider avoiding use of strong CYP3A4 inhibitors with everolimus. If combined, closely monitor for increased everolimus serum concentrations and toxicities. Everolimus dose reductions will likely be required. Consider therapy modification
Evogliptin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Evogliptin. Monitor therapy
Fedratinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fedratinib. Management: Consider alternatives when possible. If used together, decrease fedratinib dose to 200 mg/day. After the inhibitor is stopped, increase fedratinib to 300 mg/day for the first 2 weeks and then to 400 mg/day as tolerated. Consider therapy modification
FentaNYL: CYP3A4 Inhibitors (Strong) may increase the serum concentration of FentaNYL. Management: Consider fentanyl dose reductions when combined with a strong CYP3A4 inhibitor. Monitor for respiratory depression and sedation. Upon discontinuation of a CYP3A4 inhibitor, consider a fentanyl dose increase; monitor for signs and symptoms of withdrawal. Consider therapy modification
Fesoterodine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Fesoterodine. Management: Limit fesoterodine doses to 4 mg daily in patients who are also receiving strong CYP3A4 inhibitors. Consider therapy modification
Flibanserin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Flibanserin. Management: Use of flibanserin with strong CYP3A4 inhibitors is contraindicated. If starting flibanserin, start 2 weeks after the last dose of the CYP3A4 inhibitor. If starting a CYP3A4 inhibitor, start 2 days after the last dose of flibanserin. Avoid combination
Fluticasone (Nasal): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fluticasone (Nasal). Avoid combination
Fluticasone (Oral Inhalation): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fluticasone (Oral Inhalation). Consider therapy modification
Fosaprepitant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fosaprepitant. Avoid combination
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fostamatinib: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Fostamatinib. Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Galantamine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Galantamine. Monitor therapy
Gefitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Gefitinib. Monitor therapy
Gilteritinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Gilteritinib. Management: Consider alternatives to the use of a strong CYP3A4 inhibitor with gilteritinib. If the combination cannot be avoided, monitor more closely for evidence of gilteritinib toxicities. Consider therapy modification
Glasdegib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Glasdegib. Management: Consider alternatives to this combination when possible. If the combination must be used, monitor closely for evidence of QT interval prolongation and other adverse reactions to glasdegib. Consider therapy modification
GuanFACINE: CYP3A4 Inhibitors (Strong) may increase the serum concentration of GuanFACINE. Management: Reduce the extended-release guanfacine dose 50% when combined with a strong CYP3A4 inhibitor. Monitor for increased guanfacine toxicities when these agents are combined. Consider therapy modification
Halofantrine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Halofantrine. Management: The combination of halofantrine with a strong CYP3A4 inhibitor should be avoided whenever possible due to the risk for QTc interval prolongation. Avoid combination
HYDROcodone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of HYDROcodone. Monitor therapy
Hydrocortisone (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Hydrocortisone (Systemic). Monitor therapy
Ibrutinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ibrutinib. Management: Avoid concomitant use of ibrutinib and strong CYP3A4 inhibitors. If a strong CYP3A4 inhibitor must be used short-term (eg, anti-infectives for 7 days or less), interrupt ibrutinib therapy until the strong CYP3A4 inhibitor is discontinued. Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ifosfamide: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Iloperidone: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Iloperidone. Specifically, concentrations of the metabolites P88 and P95 may be increased. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Iloperidone. Management: Reduce iloperidone dose by half when administered with a strong CYP3A4 inhibitor. Consider therapy modification
Imatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Imatinib. Monitor therapy
Imidafenacin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Imidafenacin. Monitor therapy
Irinotecan Products: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Irinotecan Products. Specifically, serum concentrations of SN-38 may be increased. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Irinotecan Products. Avoid combination
Isavuconazonium Sulfate: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Isavuconazonium Sulfate. Specifically, CYP3A4 Inhibitors (Strong) may increase isavuconazole serum concentrations. Management: Combined use is considered contraindicated per US labeling. Lopinavir/ritonavir (and possibly other uses of ritonavir doses less than 400 mg every 12 hours) is treated as a possible exception to this contraindication despite strongly inhibiting CYP3A4. Avoid combination
Istradefylline: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Istradefylline. Management: Limit the maximum istradefylline dose to 20 mg daily when combined with strong CYP3A4 inhibitors and monitor for increased istradefylline effects/toxicities. Consider therapy modification
Itraconazole: May increase the serum concentration of Telithromycin. Telithromycin may increase the serum concentration of Itraconazole. Avoid combination
Ivabradine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ivabradine. Avoid combination
Ivacaftor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ivacaftor. Management: Ivacaftor dose reductions are required; consult full drug interaction monograph content for age- and weight-specific recommendations. Consider therapy modification
Ivosidenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ivosidenib. Management: Avoid use of a strong CYP3A4 inhibitor with ivosidenib whenever possible. When combined use is required, reduce the ivosidenib dose to 250 mg once daily. Consider therapy modification
Ixabepilone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ixabepilone. Management: Avoid use of ixabepilone and strong CYP3A4 inhibitors when possible. If combined, reduce the ixabepilone dose to 20 mg/m2. The previous ixabepilone dose can be resumed 1 week after discontinuation of the strong CYP3A4 inhibitor. Consider therapy modification
Ketoconazole (Systemic): May increase the serum concentration of Telithromycin. Telithromycin may increase the serum concentration of Ketoconazole (Systemic). Avoid combination
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Lapatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lapatinib. Management: Avoid use of lapatinib and strong CYP3A4 inhibitors when possible. If combined, reduce lapatinib dose to 500 mg daily. The previous lapatinib dose can be resumed 1 week after discontinuation of the strong CYP3A4 inhibitor. Consider therapy modification
Larotrectinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Larotrectinib. Management: Avoid use of strong CYP3A4 inhibitors with larotrectinib. If this combination cannot be avoided, reduce the larotrectinib dose by 50%. Increase to previous dose after stopping the inhibitor after a period of 3 to 5 times the inhibitor's half-life. Consider therapy modification
Lefamulin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin tablets and strong inhibitors of CYP3A4. Avoid combination
Lemborexant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lemborexant. Avoid combination
Lercanidipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lercanidipine. Avoid combination
Levobupivacaine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Levobupivacaine. Monitor therapy
Levomilnacipran: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Levomilnacipran. Management: Do not exceed a maximum adult levomilnacipran dose of 80 mg/day in patients also receiving strong CYP3A4 inhibitors. Consider therapy modification
Lomitapide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lomitapide. Avoid combination
Lorlatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lorlatinib. Management: Avoid use of lorlatinib with strong CYP3A4 inhibitors. If the combination cannot be avoided, reduce the lorlatinib dose from 100 mg once daily to 75 mg once daily, or from 75 mg once daily to 50 mg once daily. Consider therapy modification
Lovastatin: Telithromycin may increase the serum concentration of Lovastatin. Avoid combination
Lumateperone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lumateperone. Avoid combination
Lumefantrine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lumefantrine. Monitor therapy
Lurasidone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lurasidone. Avoid combination
Lurbinectedin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lurbinectedin. Avoid combination
Macitentan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Macitentan. Avoid combination
Manidipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Manidipine. Management: Consider avoiding concomitant use of manidipine and strong CYP3A4 inhibitors. If combined, monitor closely for increased manidipine effects and toxicities. Manidipine dose reductions may be required. Consider therapy modification
Maraviroc: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Maraviroc. Management: Reduce maraviroc to 150mg twice/day in adult and pediatrics weighing 40kg or more. See full interaction monograph for dose adjustments in pediatrics weighing 10 to less than 40kg. Do not use if CrCl less than 30mL/min or in those weighing less than 10 kg. Consider therapy modification
MedroxyPROGESTERone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of MedroxyPROGESTERone. Monitor therapy
Meperidine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Meperidine. Monitor therapy
Midazolam: Macrolide Antibiotics may increase the serum concentration of Midazolam. Management: Consider an alternative less likely to interact. Azithromycin is likely a lower-risk macrolide, and benzodiazepines less dependent on CYP3A metabolism (e.g., lorazepam, oxazepam) are similarly less likely to interact. Consider therapy modification
Midostaurin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Midostaurin. Management: Seek alternatives to the concomitant use of midostaurin and strong CYP3A4 inhibitors if possible. If concomitant use cannot be avoided, monitor patients for increased risk of adverse reactions. Consider therapy modification
MiFEPRIStone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of MiFEPRIStone. Management: For treatment of hyperglycemia in Cushing's syndrome, start mifepristone at 300 mg/day, may titrate to a maximum of 900 mg/day. If starting a strong CYP3A4 inhibitor and taking >300 mg/day mifepristone, decrease the mifepristone dose by 300 mg/day. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mirodenafil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Mirodenafil. Management: Consider using a lower dose of mirodenafil when used with strong CYP3A4 inhibitors. Monitor for increased mirodenafil effects/toxicities with the use of this combination. Consider therapy modification
Mirtazapine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Mirtazapine. Monitor therapy
Mizolastine: Macrolide Antibiotics may increase the serum concentration of Mizolastine. Avoid combination
Mometasone (Oral Inhalation): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Mometasone (Oral Inhalation). Monitor therapy
Naldemedine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Naldemedine. Monitor therapy
Nalfurafine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Nalfurafine. Monitor therapy
Naloxegol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Naloxegol. Avoid combination
Neratinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Neratinib. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nilotinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Nilotinib. Management: Avoid if possible. If combination needed, decrease nilotinib to 300 mg once/day for patients with resistant or intolerant Ph+ CML or to 200 mg once/day for patients with newly diagnosed Ph+ CML in chronic phase. Consider therapy modification
NiMODipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of NiMODipine. Avoid combination
Nisoldipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Nisoldipine. Avoid combination
Olaparib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Olaparib. Management: Avoid use of strong CYP3A4 inhibitors with olaparib, if possible. If such concurrent use cannot be avoided, the dose of olaparib tablets should be reduced to 100 mg twice daily and the dose of olaparib capsules should be reduced to 150 mg twice daily. Consider therapy modification
Oliceridine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Oliceridine. Monitor therapy
Osilodrostat: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Osilodrostat. Management: Reduce osilodrostat dose by 50% during coadministration with a strong CYP3A4 inhibitor. Consider therapy modification
Ospemifene: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ospemifene. Monitor therapy
Oxybutynin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Oxybutynin. Monitor therapy
Palbociclib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Palbociclib. Management: Avoid concurrent use of strong CYP3A4 inhibitors with palbociclib when possible. If the use of a strong CYP3A4 inhibitor cannot be avoided, decrease the palbociclib dose to 75 mg/day. Consider therapy modification
Panobinostat: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Panobinostat. Management: Reduce the panobinostat dose to 10 mg when it must be used with a strong CYP3A4 inhibitor. Monitor patient response to therapy closely for evidence of more severe adverse effects related to panobinostat therapy. Consider therapy modification
Parecoxib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Parecoxib. Specifically, serum concentrations of the active moiety valdecoxib may be increased. Monitor therapy
Paricalcitol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Paricalcitol. Monitor therapy
PAZOPanib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of PAZOPanib. Management: Avoid concurrent use of pazopanib with strong inhibitors of CYP3A4 whenever possible. If it is not possible to avoid such a combination, reduce pazopanib dose to 400 mg. Further dose reductions may also be required if adverse reactions occur. Consider therapy modification
Pemigatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pemigatinib. Management: If combined use cannot be avoided, reduce the pemigatinib dose from 13.5 mg daily to 9 mg daily, or from 9 mg daily to 4.5 mg daily. Resume prior pemigatinib dose after stopping the strong inhibitor once 3 half-lives of the inhibitor has passed. Consider therapy modification
Pexidartinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pexidartinib. Management: Avoid use of pexidartinib with strong CYP3A4 inhibitors if possible. If combined use cannot be avoided, pexidartinib dose should be reduced. Decrease 800 mg or 600 mg daily doses to 200 mg twice daily. Decrease doses of 400 mg per day to 200 mg once daily Consider therapy modification
Pimavanserin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pimavanserin. Management: Decrease the pimavanserin dose to 10 mg daily when combined with strong CYP3A4 inhibitors. Consider therapy modification
Pimecrolimus: CYP3A4 Inhibitors (Strong) may decrease the metabolism of Pimecrolimus. Monitor therapy
Pimozide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pimozide. Avoid combination
Piperaquine: CYP3A4 Inhibitors (Strong) may enhance the QTc-prolonging effect of Piperaquine. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Piperaquine. Management: Avoid concomitant use of piperaquine and strong CYP3A4 inhibitors when possible. If the combination cannot be avoided, frequent ECG monitoring is recommended due to the risk for QTc prolongation. Consider therapy modification
Pitavastatin: Telithromycin may increase the serum concentration of Pitavastatin. Monitor therapy
Polatuzumab Vedotin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Polatuzumab Vedotin. Exposure to unconjugated MMAE, the cytotoxic small molecule component of polatuzumab vedotin, may be increased. Monitor therapy
PONATinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of PONATinib. Management: Reduce the adult starting dose of ponatinib to 30 mg daily during treatment with any strong CYP3A4 inhibitor. Consider therapy modification
Pralsetinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pralsetinib. Avoid combination
Pranlukast: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pranlukast. Monitor therapy
Pravastatin: Telithromycin may increase the serum concentration of Pravastatin. Monitor therapy
Praziquantel: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Praziquantel. Monitor therapy
PrednisoLONE (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of PrednisoLONE (Systemic). Monitor therapy
PredniSONE: CYP3A4 Inhibitors (Strong) may increase the serum concentration of PredniSONE. Monitor therapy
Propafenone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Propafenone. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QUEtiapine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of QUEtiapine. Management: In quetiapine treated patients, reduce quetiapine to one-sixth of regular dose after starting strong CYP3A4 inhibitor. In those on strong CYP3A4 inhibitors, start quetiapine at lowest dose and up-titrate as needed. Consider therapy modification
Quinidine (Non-Therapeutic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Quinidine (Non-Therapeutic). Monitor therapy
QuiNINE: Telithromycin may enhance the QTc-prolonging effect of QuiNINE. Telithromycin may increase the serum concentration of QuiNINE. Management: Concomitant therapy with quinine and telithromycin should be avoided, if possible, due to the risk of elevated quinine serum levels and potential adverse cardiac effects. If combined, monitor for QT prolongation and quinine toxicities. Consider therapy modification
Radotinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Radotinib. Avoid combination
Ramelteon: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ramelteon. Monitor therapy
Ranolazine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ranolazine. Avoid combination
Red Yeast Rice: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Red Yeast Rice. Specifically, concentrations of lovastatin and related compounds found in Red Yeast Rice may be increased. Avoid combination
Regorafenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Regorafenib. Avoid combination
Repaglinide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Repaglinide. Management: The addition of a CYP2C8 inhibitor to this drug combination may substantially increase the magnitude of increase in repaglinide exposure. Monitor therapy
Retapamulin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Retapamulin. Management: Avoid this combination in patients less than 2 years old. No action is required in other populations. Monitor therapy
Ribociclib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ribociclib. Management: Avoid use of ribociclib with strong CYP3A4 inhibitors when possible; if combined use cannot be avoided, reduce ribociclib dose to 400 mg once daily. Consider therapy modification
Rifamycin Derivatives: Macrolide Antibiotics may decrease the metabolism of Rifamycin Derivatives. Monitor therapy
Rilpivirine: Macrolide Antibiotics may increase the serum concentration of Rilpivirine. Management: Consider the use of azithromycin or another non-macrolide alternative when appropriate to avoid this potential interaction. Consider therapy modification
Rimegepant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Rimegepant. Avoid combination
Riociguat: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Riociguat. Monitor therapy
Ripretinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ripretinib. Monitor therapy
RomiDEPsin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of RomiDEPsin. Monitor therapy
Rupatadine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Rupatadine. Avoid combination
Ruxolitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ruxolitinib. Management: This combination should be avoided under some circumstances; dose adjustments may be required in some circumstances and depend on the indication for ruxolitinib. See monograph for details. Consider therapy modification
Salmeterol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Salmeterol. Avoid combination
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
SAXagliptin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of SAXagliptin. Management: Limit the saxagliptin dose to 2.5 mg daily when combined with strong CYP3A4 inhibitors. When using the saxagliptin combination products saxagliptin/dapagliflozin or saxagliptin/dapagliflozin/metformin, avoid use with strong CYP3A4 inhibitors. Consider therapy modification
Selpercatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Selpercatinib. Management: Avoid combination if possible. If use is necessary, reduce selpercatinib dose as follows: from 120 mg twice/day to 40 mg twice/day, or from 160 mg twice/day to 80 mg twice/day. Consider therapy modification
Selumetinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Selumetinib. Management: Avoid concomitant use when possible. If combined, selumetinib dose reductions are recommended and vary based on body surface area and selumetinib dose. For details, see the full drug interaction monograph or selumetinib prescribing information. Consider therapy modification
Sibutramine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Sibutramine. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Sibutramine. Monitor therapy
Sildenafil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Sildenafil. Management: Use of sildenafil for pulmonary hypertension should be avoided with strong CYP3A4 inhibitors. When used for erectile dysfunction, starting adult dose should be reduced to 25 mg. Maximum adult dose with ritonavir or cobicistat is 25 mg per 48 hours. Consider therapy modification
Silodosin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Silodosin. Avoid combination
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Simeprevir. Avoid combination
Simvastatin: Telithromycin may increase the serum concentration of Simvastatin. Avoid combination
Sirolimus: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Sirolimus. Management: Avoid concurrent use of sirolimus with strong CYP3A4 inhibitors when possible and alternative agents with lesser interaction potential with sirolimus should be considered. Concomitant use of sirolimus and voriconazole or posaconazole is contraindicated. Consider therapy modification
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Solifenacin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Solifenacin. Management: Limit adult solifenacin doses to 5 mg daily and limit doses in pediatric patients to the recommended weight-based starting dose (and do not increase the dose) when combined with strong CYP3A4 inhibitors. Consider therapy modification
Sonidegib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Sonidegib. Avoid combination
SORAfenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of SORAfenib. Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
SUFentanil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of SUFentanil. Management: If a strong CYP3A4 inhibitor is initiated in a patient on sufentanil, consider a sufentanil dose reduction and monitor for increased sufentanil effects and toxicities (eg, respiratory depression). Consider therapy modification
SUNItinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of SUNItinib. Management: Avoid when possible. If combined, decrease sunitinib dose to a minimum of 37.5 mg daily when treating GIST or RCC. Decrease sunitinib dose to a minimum of 25 mg daily when treating PNET. Monitor patients for both reduced efficacy and increased toxicities. Consider therapy modification
Suvorexant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Suvorexant. Avoid combination
Tacrolimus (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tacrolimus (Systemic). Management: Reduce tacrolimus dose to one-third of the original dose if starting posaconazole or voriconazole. Coadministration with nelfinavir is not generally recommended. Tacrolimus dose reductions or prolongation of dosing interval will likely be required. Consider therapy modification
Tacrolimus (Topical): Macrolide Antibiotics may increase the serum concentration of Tacrolimus (Topical). Monitor therapy
Tadalafil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tadalafil. Management: Avoid this combination in patients taking tadalafil for pulmonary arterial hypertension. In patients taking tadalafil for ED or BPH, max tadalafil dose is 2.5 mg if taking daily or 10 mg no more frequently than every 72 hours if used as needed. Consider therapy modification
Tamsulosin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tamsulosin. Avoid combination
Tasimelteon: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tasimelteon. Monitor therapy
Tazemetostat: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tazemetostat. Avoid combination
Temsirolimus: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Temsirolimus. Management: Avoid concomitant use of temsirolimus and strong CYP3A4 inhibitors. If coadministration is unavoidable, decrease temsirolimus dose to 12.5 mg per week. Resume previous temsirolimus dose 1 week after discontinuation of the strong CYP3A4 inhibitor. Consider therapy modification
Terfenadine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Terfenadine. Avoid combination
Tetrahydrocannabinol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tetrahydrocannabinol and Cannabidiol. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tezacaftor and Ivacaftor. Management: If combined with strong CYP3A4 inhibitors, tezacaftor/ivacaftor should be administered in the morning, twice a week, approximately 3 to 4 days apart. Tezacaftor/ivacaftor dose depends on age and weight; see full Lexi-Interact monograph for details. Consider therapy modification
Thioridazine: CYP2D6 Inhibitors (Weak) may increase the serum concentration of Thioridazine. Management: Consider avoiding concomitant use of thioridazine and weak CYP2D6 inhibitors. If combined, monitor closely for QTc interval prolongation and arrhythmias. Some weak CYP2D6 inhibitors list use with thioridazine as a contraindication. Consider therapy modification
Thiotepa: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Thiotepa. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Thiotepa. Management: Thiotepa prescribing information recommends avoiding concomitant use of thiotepa and strong CYP3A4 inhibitors. If concomitant use is unavoidable, monitor for adverse effects and decreased efficacy. Consider therapy modification
Ticagrelor: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Ticagrelor. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ticagrelor. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tofacitinib. Management: Tofacitinib dose reductions are recommended when combined with strong CYP3A4 inhibitors. Recommended dose adjustments vary by tofacitinib formulation and therapeutic indication. See full Lexi Interact monograph for details. Consider therapy modification
Tolterodine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tolterodine. Management: The maximum recommended dose of tolterodine is 2 mg per day (1 mg twice daily for immediate-release tablets or 2 mg daily for extended-release capsules) when used together with a strong CYP3A4 inhibitor. Consider therapy modification
Tolvaptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tolvaptan. Avoid combination
Toremifene: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Toremifene. Management: Use of toremifene with strong CYP3A4 inhibitors should be avoided if possible. If coadministration is necessary, monitor for increased toremifene toxicities, including QTc interval prolongation. Consider therapy modification
Trabectedin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Trabectedin. Avoid combination
TraMADol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of TraMADol. Monitor therapy
TraZODone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of TraZODone. Management: Consider the use of a lower trazodone dose and monitor for increased trazodone effects (eg, sedation, QTc prolongation) if combined with strong CYP3A4 inhibitors. Consider therapy modification
Triamcinolone (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Triamcinolone (Systemic). Monitor therapy
Triazolam: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Triazolam. Avoid combination
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Avoid use of live attenuated typhoid vaccine (Ty21a) in patients being treated with systemic antibacterial agents. Postpone vaccination until 3 days after cessation of antibiotics and avoid starting antibiotics within 3 days of last vaccine dose. Consider therapy modification
Ubrogepant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ubrogepant. Avoid combination
Udenafil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Udenafil. Avoid combination
Ulipristal: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ulipristal. Management: This is specific for when ulipristal is being used for signs/symptoms of uterine fibroids (Canadian indication). When ulipristal is used as an emergency contraceptive, patients receiving this combo should be monitored for ulipristal toxicity. Avoid combination
Upadacitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Upadacitinib. Monitor therapy
Valbenazine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Valbenazine. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Valbenazine. Management: Reduce the valbenazine dose to 40 mg daily when combined with strong CYP3A4 inhibitors. Consider therapy modification
Vardenafil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vardenafil. Management: Limit Levitra (vardenafil) dose to a single 2.5 mg dose within a 24-hour period if combined with strong CYP3A4 inhibitors. Avoid concomitant use of Staxyn (vardenafil) and strong CYP3A4 inhibitors. Combined use is contraindicated outside of the US. Consider therapy modification
Vemurafenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vemurafenib. Management: Avoid concurrent use of vemurafenib with strong CYP3A4 inhibitors when possible. If concomitant use is unavoidable, consider a vemurafenib dose reduction if clinically indicated. Consider therapy modification
Venetoclax: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Venetoclax. Management: Coadministration is contraindicated during venetoclax initiation and ramp-up in CLL/SLL patients. Reduced venetoclax doses are required during ramp-up for patients with AML, and all maintenance therapy. See full Lexi Interact monograph for details. Consider therapy modification
Verapamil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Verapamil. Management: Consider alternatives to this combination when possible. If combined, monitor for increased verapamil effects and toxicities (eg, hypotension, bradycardia). Consider therapy modification
Vilanterol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vilanterol. Monitor therapy
Vilazodone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vilazodone. Management: Limit the maximum vilazodone dose to 20 mg daily in patients receiving strong CYP3A4 inhibitors. The original vilazodone dose can be resumed following discontinuation of the strong CYP3A4 inhibitor. Consider therapy modification
VinBLAStine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of VinBLAStine. Monitor therapy
VinCRIStine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of VinCRIStine. Management: Seek alternatives to this combination when possible. If combined, monitor closely for vincristine toxicities (eg, neurotoxicity, gastrointestinal toxicity, myelosuppression). Consider therapy modification
VinCRIStine (Liposomal): CYP3A4 Inhibitors (Strong) may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vindesine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vindesine. Monitor therapy
Vinflunine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vinflunine. Avoid combination
Vinorelbine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vinorelbine. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Macrolide Antibiotics may increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Vorapaxar: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vorapaxar. Avoid combination
Voxelotor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and strong CYP3A4 inhibitors. If concomitant use is unavoidable, reduce the voxelotor dose to 1,000 mg once daily. Consider therapy modification
Zanubrutinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Zanubrutinib. Management: Decrease the zanubrutinib dose to 80 mg once daily during coadministration with a strong CYP3A4 inhibitor. Further dose adjustments may be required for zanubrutinib toxicities, refer to prescribing information for details. Consider therapy modification
Zolpidem: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Zolpidem. Monitor therapy
Zopiclone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Zopiclone. Management: If coadministered with strong CYP3A4 inhibitors, initiate zopiclone at 3.75 mg in adults, with a maximum dose of 5 mg. Monitor for zopiclone toxicity (eg, drowsiness, confusion, lethargy, ataxia, respiratory depression). Consider therapy modification
Adverse Reactions
The following adverse drug reactions and incidences are derived from product labeling unless otherwise specified.
>10%: Gastrointestinal: Diarrhea (10% to 11%)
2% to 10%:
Central nervous system: Headache (2% to 6%), dizziness (3% to 4%)
Gastrointestinal: Nausea (7% to 8%), vomiting (2% to 3%), dysgeusia (2%), loose stools (2%)
≥0.2% to <2%:
Central nervous system: Drowsiness, fatigue, insomnia, vertigo
Dermatologic: Diaphoresis, skin rash
Gastrointestinal: Abdominal distension, abdominal pain, anorexia, constipation, dyspepsia, flatulence, gastric distress, gastritis, gastroenteritis, glossitis, oral candidiasis, stomatitis, xerostomia
Genitourinary: Fungal vaginosis, vaginitis, vulvovaginal candidiasis
Hematologic & oncologic: Thrombocythemia
Hepatic: Abnormal hepatic function tests, increased serum transaminases
Ophthalmic: Accommodation disturbance, blurred vision, diplopia
<0.2%, postmarketing, and/or case reports: Ageusia, altered sense of smell, anaphylaxis, angioedema, anosmia, anxiety, arthralgia, atrial arrhythmia, bradycardia, cardiac arrhythmia, confusion, convulsions, dyspnea, eczema, eosinophilia, erythema multiforme, exacerbation of myasthenia gravis, facial edema, flushing, hallucination, hepatic failure, hepatic injury (including necrosis), hepatitis, hypersensitivity reaction, hypotension, increased serum alkaline phosphatase, increased serum bilirubin, ischemic heart disease, jaundice, loss of consciousness (may be vagal-related), muscle cramps, myalgia, palpitations, pancreatitis, paresthesia, prolonged QT interval on ECG, pruritus, pseudomembranous colitis, respiratory failure, syncope, torsades de pointes, tremor, urticaria, urine discoloration, ventricular arrhythmia, ventricular tachycardia
ALERT: U.S. Boxed Warning
Myasthenia gravis:Telithromycin is contraindicated in patients with myasthenia gravis. There have been reports of fatal and life-threatening respiratory failure in patients with myasthenia gravis associated with the use of telithromycin.
Warnings/Precautions
Concerns related to adverse effects:
• Altered cardiac conduction: May prolong QTc interval, leading to a risk of ventricular arrhythmias, including torsades de pointes. Avoid in patients with congenital prolongation of QTc interval, ongoing proarrhythmic conditions (including uncorrected hypokalemia or hypomagnesemia), significant bradycardia, or concurrent therapy with QTc-prolonging drugs (eg, class Ia and class III antiarrhythmics).
• Hepatic effects: Acute hepatic failure and severe liver injury (some fatal), including fulminant hepatitis and hepatic necrosis (leading to liver transplant) have been reported, in some cases after only a few doses; if signs/symptoms of hepatitis or liver damage occur, discontinue therapy and initiate liver function testing. If clinical hepatitis or transaminase evaluations combined with other systemic symptoms occur, permanently discontinue. Do not readminister to patients with a previous history of hepatitis and/or jaundice associated with the use of telithromycin or any macrolide antibiotic. Less severe hepatic dysfunction associated with increased liver enzymes and hepatitis with or without jaundice has also been reported; these events were reversible.
• Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
• Syncope: May cause loss of consciousness (possibly vagal-related); caution patients that these events may interfere with ability to operate machinery or drive, and to use caution until effects are known.
• Visual disturbances: May cause visual disturbances (eg, changes in accommodation ability, diplopia, blurred vision); most cases are mild to moderate, but severe cases have been reported. Caution patients that these events may interfere with ability to operate machinery or drive, and to use caution until effects are known.
Disease-related concerns:
• Myasthenia gravis: [U.S. Boxed Warning]: Life-threatening (including fatal) respiratory failure has occurred in patients with myasthenia gravis; use in these patients is contraindicated. Exacerbations of myasthenia gravis may occur within hours of the first dose; respiratory failure with a rapid onset and progression has been reported.
• Renal impairment: Use with caution in patients with renal impairment; severe impairment (CrCl <30 mL/minute) requires dosage adjustment.
Monitoring Parameters
Liver function tests; signs/symptoms of liver failure (eg, jaundice, fatigue, malaise, anorexia, nausea, bilirubinemia, acholic stools, liver tenderness, hepatomegaly); visual acuity
Pregnancy Risk Factor C Pregnancy Considerations
Adverse events have been observed in animal reproduction studies
Patient Education
What is this drug used for?
• It is used to treat bacterial infections.
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
• Headache
• Nausea
• Vomiting
• Diarrhea
• Change in taste
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
• Severe dizziness
• Passing out
• Fast heartbeat
• Slow heartbeat
• Arrhythmia
• Bruising
• Bleeding
• Vision changes
• Confusion
• Sensing things that seem real but are not
• Muscle weakness
• Vaginal pain, itching, and discharge
• Clostridioides (formerly Clostridium) difficile-associated diarrhea like stomach pain or cramps, very loose or watery stools, or bloody stools.
• Liver problems like dark urine, feeling tired, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes.
• Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a limited summary of general information about the medicine's uses from the patient education leaflet and is not intended to be comprehensive. This limited summary does NOT include all information available about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not intended to provide medical advice, diagnosis or treatment and does not replace information you receive from the healthcare provider. For a more detailed summary of information about the risks and benefits of using this medicine, please speak with your healthcare provider and review the entire patient education leaflet.
More about telithromycin
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: ketolides
- Breastfeeding
Patient resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.