Lithium (Monograph)
Brand names: Eskalith, Lithobid
Drug class: Antimanic Agents
VA class: CN750
CAS number: 554-13-2
Warning
-
Lithium toxicity is closely related to serum lithium concentrations and can occur at dosages close to therapeutic levels.
-
Facilities for prompt and accurate serum lithium determinations should be available before initiating therapy. (See Renal Effects under Cautions.)
Introduction
Antimanic agent.
Uses for Lithium
Bipolar Disorder
Management of bipolar disorder, particularly acute manic or mixed episodes in patients with bipolar 1 or bipolar 2 disorder.
A first-line agent in the initial treatment of depressive, manic, or mixed episodes in patients with bipolar disorder.
Combination therapy with an atypical antipsychotic, another mood stabilizing agent, and/or antidepressant may be required to adequately treat rapid cycling and more severe depressive, manic, or mixed episodes.
Maintenance therapy has been shown to prevent or diminish the intensity of subsequent manic episodes in patients with bipolar disorder with a history of mania.
Major Depression† [off-label]
Should be used only in patients who fail to respond to other antidepressants.
Schizoaffective and Schizophrenic Disorders† [off-label]
Limited effectiveness when used alone; should be used only after antipsychotic agents have failed.
May be added to existing antipsychotic therapy, but efficacy of such combined therapy has varied in different clinical studies. Careful monitoring (e.g., serum lithium concentrations, adverse effects, possible adverse drug interactions) recommended.
Disorders of Impulse Control† [off-label]
Has reduced temper outbursts, impulsive antisocial behavior, and the number of assaultive acts in a small number of adults with disorders of impulse control† [off-label].
Psychiatric Disorders in Children† [off-label]
Treatment of children with apparent mixed bipolar disorder symptomatology†, hyperactivity with psychotic or neurotic components†, or aggressive behavior† or aggressive outbursts† associated with attention-deficit hyperactivity disorder (ADHD); should be used only after more conservative therapies have failed.
Neutropenia and Anemia†
Treatment of neutropenia† or anemia† secondary to antineoplastic drugs.
Routine use not recommended for congenital, idiopathic, or cyclic neutropenias†; Felty’s syndrome†; or aplastic anemia†.
Hyperthyroidism†
Treatment of hyperthyroidism†; other treatments (e.g., radioactive iodine, surgery, propylthiouracil, methimazole) currently are preferred.
SIADH†
No longer considered one of the therapies of choice; generally has been replaced with other more effective and/or less toxic therapies (e.g., demeclocycline).
Lithium Dosage and Administration
General
-
Careful monitoring of serum lithium concentrations and clinical status of the patient is mandatory and patients should be carefully instructed in the safe use of the drug.
-
Carefully review the precautions and contraindications associated with lithium use before initiating therapy.
-
Monitor serum lithium concentrations twice weekly during initiation of the acute phase of therapy and until serum concentration and clinical condition have stabilized; patient’s ability to tolerate high serum lithium concentrations usually decreases as initial manic symptoms begin to subside.
-
After the patient has been stabilized, monitor serum concentrations at least every 2 months in most patients.
-
Onset of acute antimanic effect of lithium usually occurs within 5–7 days; full therapeutic effect often requires 10–21 days.
-
The manufacturers suggest that steady-state serum lithium concentrations be determined immediately before the next dose (i.e., 8–12 hours after the previous lithium dose). Total reliance must not be placed on serum lithium concentrations alone; accurate patient evaluation requires both careful clinical and laboratory evaluation.
-
Serum lithium concentrations of 1–1.2 mEq/L usually are required during acute affective episodes. Serum concentration should not exceed 1.5 mEq/L during the acute treatment phase.
-
If manifestations of lithium toxicity occur (see Lithium Toxicity under Cautions), temporarily discontinue for 24–48 hours, then resume at a lower dosage.
Administration
Oral Administration
Administer orally, preferably with meals in divided doses.
Administer conventional tablets, capsules, or oral solution 3 or 4 times daily; twice daily administration may be associated with adverse GI or nervous system effects. Administer extended-release tablets 2 or 3 times daily.
Extended-release preparations should be swallowed intact and should not be chewed, crushed, or halved.
Lithium citrate oral solutions may be useful in patients unable to swallow capsules or tablets; 5 mL of a commercially available solution contains about 8 mEq of lithium and is approximately equivalent to 300 mg of lithium carbonate.
Dosage
Available as lithium carbonate and lithium citrate; dosages expressed in terms of the salts.
Pediatric Patients
Bipolar Disorder
Acute Episodes†
OralChildren ≤11 years of age: Usual dosages not established; lithium carbonate dosages of 15–20 mg/kg (about 0.4–0.5 mEq/kg) daily or equivalent lithium citrate dosages have been given in 2 or 3 divided doses. (Do not exceed usual adult dosages. )
Children ≥12 years of age: Dosages usually are the same as those of adults.
Maintenance Dosages†
OralUsual maintenance dosages have not been established; dosage should be adjusted according to serum lithium concentrations, patient tolerance, and clinical response.
Adults
Bipolar Disorder
Acute Episodes
OralInitially, 1.8 g daily as conventional lithium carbonate capsules or tablets, given in 3 or 4 divided doses, or 30 mL (about 48 mEq of lithium) of lithium citrate oral solution daily, given in 3 divided doses.
Alternatively, 900 mg twice daily (morning and evening) or 600 mg 3 times daily as extended-release lithium carbonate tablets.
Maintenance Dosages
Oral900 mg to 1.2 g daily as conventional lithium carbonate capsules or tablets, given in 3 or 4 divided doses, or 15–20 mL (about 24–32 mEq of lithium) of lithium citrate oral solution daily, given in 3 or 4 divided doses. This dosage generally provides serum lithium concentrations of 0.6–1.2 mEq/L.
Alternatively, 900 mg to 1.2 g daily as extended-release lithium carbonate tablets, given in 2 or 3 divided doses.
Prescribing Limits
Pediatric Patients
Bipolar Disorder
Oral
When calculating dosage based on weight, do not exceed usual adult dosage.
Adults
Bipolar Disorder
Oral
Maintenance dosage usually should not exceed 2.4 g of lithium carbonate (65 mEq) daily.
Special Populations
Geriatric Patients
Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy. Lower initial dosages (e.g., ≤900 mg of lithium carbonate daily) and more gradual dosage titration recommended.
May have decreased renal function; monitor renal function and adjust dosage accordingly.
Dosages that produce serum lithium concentrations at the lower end of therapeutic range may be sufficient for maintenance. (See Geriatric Use under Cautions.)
Pregnant Women
Dosages generally need to be increased during pregnancy but should be reduced 1 week before parturition or when labor begins. (See Fetal/Neonatal Morbidity and Mortality and also see Pregnancy under Cautions.)
Cautions for Lithium
Contraindications
-
Significant renal or cardiovascular disease, severe debilitation, dehydration, sodium depletion, or concomitant therapy with diuretics; very high risk of lithium toxicity under such conditions.
-
Only begin lithium in such patients if psychiatric indication is life-threatening, and other treatments have failed; however, must use with extreme caution, including daily serum lithium determinations and adjustment to usually low doses ordinarily tolerated by these individuals. In such instances, hospitalization is a necessity.
Warnings/Precautions
Warnings
Fetal/Neonatal Morbidity and Mortality
May cause fetal toxicity (e.g., increase in cardiac and other anomalies, especially Ebstein’s anomaly) when administered to pregnant women, but potential benefits may be acceptable in certain conditions despite the possible risks to the fetus.
If used in women of childbearing potential, during pregnancy, or if a patient becomes pregnant during treatment, the patient should be be informed of the potential hazard to the fetus.
Whenever possible, lithium should be withdrawn for at least the first trimester unless it is determined that this would seriously endanger the mother. (See Pregnant Women under Dosage and Administration and see Pregnancy under Cautions.)
Lithium Toxicity
Risk of toxicity increases with increasing serum lithium concentrations. Serum concentration should not exceed 1.5 mEq/L during the acute treatment phase.
Serum lithium concentrations >1.5 mEq/L usually carry a greater risk than lower levels. (See General under Dosage and Administration.)
Diarrhea, vomiting, drowsiness, muscular weakness and lack of coordination may be early signs of lithium toxicity, and can occur at lithium concentrations <2 mEq/L. At higher levels, giddiness, ataxia, blurred vision, tinnitus, and a large output of dilute urine may be seen.
Serum lithium levels above 3 mEq/L may produce a complex clinical picture involving multiple organs and organ systems. (See General under Dosage and Administration.)
Renal Effects
Diminution of renal concentrating ability, occasionally presenting as nephrogenic diabetes insipidus, with polyuria and polydipsia, possible following chronic lithium therapy. Morphologic changes with glomerular and interstitial fibrosis and nephron atrophy also possible.
Measurement of 24-hour Clcr, renal-concentrating ability, and a urinalysis recommended prior to initiating therapy. Renal function should then be evaluated every 2–3 months for the first 6 months, then every 6–12 months during therapy or whenever clinically indicated.
If progressive or sudden changes in renal function, even within the normal range, occur during lithium therapy, reevaluate need for therapy with the drug.
Interactions
Encephalopathic syndrome reported with concomitant use with antipsychotic agents. May be similar to or same as neuroleptic malignant syndrome (NMS). (See Specific Drugs under Interactions.)
May prolong effects of neuromuscular blocking agents. (See Specific Drugs under Interactions.)
General Precautions
Concomitant Illnesses
Decreased tolerance to lithium has been reported to ensue from protracted sweating, diarrhea, or concomitant infection with elevated temperatures and may necessitate a temporary reduction or cessation of medication. Patients should maintain their usual fluid (2.5–3 L/day) and sodium intake, and supplement these in the event of fever (e.g., during infections), vomiting, or diarrhea.
Sodium-restricted Diet
Use with caution in patients whose sodium intake is restricted; stabilize sodium intake and carefully titrate lithium dosage to avoid increased serum lithium concentrations that may occur with sodium depletion.
Endocrine Effects
Hypothyroidism, with manifestations ranging from mild to severe myxedema, may occur within weeks to years after initiating lithium therapy; rarely, hypothyroidism may persist after discontinuance of the drug. Geriatric patients and patients with antithyroglobulin antibody, a prior history of Graves’ disease or Hashimoto’s thyroiditis, or those receiving iodine appear most at risk. Paradoxically, a few cases of hyperthyroidism also have been reported.
Preexisting thyroid disorders are not contraindications to lithium therapy. Patients with underlying hypothyroidism should have thyroid function (T3, T4, and TSH concentrations) evaluated yearly and be given supplemental thyroid therapy when needed.
Specific Populations
Pregnancy
Category D. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Women of childbearing age receiving lithium should be counseled about methods of birth control. If used during pregnancy, carefully monitor serum lithium concentrations and adjust dosage accordingly. (See Pregnant Women under Dosage and Administration.)
Lactation
Lithium is distributed into milk; discontinue nursing or the drug, taking into account the importance of the drug to the woman.
Pediatric Use
Safety and efficacy have not been established in children <12 years of age; however, the drug has been used in this age group when benefits were thought to outweigh risks.
Transient acute dystonia and hyperreflexia occurred in a 15-kg child who ingested 300 mg of lithium carbonate.
Geriatric Use
Insufficient experience with extended-release tablets in patients ≥65 years of age to determine whether geriatric patients respond differently than younger patients.
Age-related differences in response to lithium generally not observed.
Use with caution; geriatric patients appear more susceptible to adverse effects (e.g., adverse nervous system and neuromuscular effects), even at therapeutic serum concentrations, and more prone to developing lithium-induced goiter and clinical hypothyroidism. Some clinicians recommend that thyroid function tests be performed every 6–12 months in these patients.
Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and potential for concomitant disease and drug therapy; geriatric patients should receive initial lithium dosages in the lower end of the usual range (see Geriatric Patients under Dosage and Administration).
Lithium is substantially excreted by the kidneys; consider monitoring renal function and adjust dosage if necessary since geriatric patients are more likely to have decreased renal function.
Common Adverse Effects
Fine hand tremor, polyuria, mild thirst, transient and mild nausea, and general discomfort may appear during the first few days of lithium administration; usually subside with continued treatment, a temporary reduction of dosage, or temporary cessation. If persistent, a cessation of therapy is indicated.
Drug Interactions
Lithium is not metabolized.
Electroconvulsive Therapy
Acute neurotoxicity with prominent delirium has occurred in patients receiving lithium and electroconvulsive therapy (ECT) concurrently. Some clinicians recommend decreasing lithium dosage or withdrawing the drug 2 days prior to ECT.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Increased plasma lithium concentrations resulting in several cases of lithium intoxication |
If used concomitantly, adjust lithium dosages and carefully monitor serum lithium concentrations Some clinicians advise against concomitant ACE inhibitor use in geriatric patients or those patients with CHF, renal insufficiency, or volume depletion |
|
Alkalinizing agents (e.g., sodium bicarbonate) |
May increase renal excretion of lithium |
Higher lithium dosage may be required |
|
Anticonvulsants (e.g., carbamazepine, phenytoin) |
Adverse neurologic effects following concomitant therapy with carbamazepine or phenytoin Concurrent use of lithium and phenytoin may increase serum lithium concentrations |
Clinical importance not determined |
|
Antidepressants, SSRIs (e.g., fluoxetine, paroxetine) |
Possibly associated with increased serum lithium concentrations, lithium toxicity, and/or serotonin syndrome (e.g., absence seizures, agitation, ataxia, confusion, diarrhea, dizziness, dysarthria, stiffness of the extremities, tremor); decreased serum lithium concentrations also reported |
Use with caution and monitor closely |
|
Antipsychotic agents (e.g., haloperidol, phenothiazines) |
Acute encephalopathic syndromes or extrapyramidal reactions (e.g., NMS or NMS-type reactions), possibly resulting in irreversible brain damage, parkinsonian movements, and dyskinesias Nausea and vomiting, which are occasionally signs of lithium intoxication, may be masked by the antiemetic effect of some phenothiazines when used concurrently |
Monitor patients for adverse neurologic effects, especially when large dosages of lithium and an antipsychotic agent are used; combined therapy should be promptly discontinued if such signs or symptoms appear |
|
β-Adrenergic blocking agents |
Absence of tremor may make lithium intoxication more difficult to diagnose |
Monitor for other signs and symptoms of lithium intoxication |
|
Baclofen |
May cause hyperkinetic movements |
|
|
Calcium-channel blocking agents (e.g., verapamil) |
May potentiate the toxic effects of lithium; neurotoxicity (e.g., ataxia, choreoathetosis, tremors, tinnitus), adverse GI effects (e.g., nausea, vomiting, diarrhea), and bradycardia reported Decreased serum lithium concentrations following initiation of verapamil in patients stabilized on lithium therapy |
Use with caution Monitor serum lithium concentrations and patient; adjust lithium dosage accordingly when verapamil is initiated or discontinued in patients receiving lithium therapy |
|
Diazepam |
Profound hypothermia has been reported in at least one patient |
Widespread use usually without unusual adverse effects indicates that it is safe in most patients |
|
Diuretics (e.g., amiloride, aminophylline, furosemide, spironolactone, thiazides, urea) |
Decreased lithium clearance resulting in increased serum lithium concentrations and several cases of lithium intoxication have occurred with concomitant thiazide use Other diuretics (e.g., aminophylline, furosemide, spironolactone, urea) also may reduce renal clearance of lithium Amiloride does not appear to substantially affect lithium pharmacokinetics in most patients |
Concomitant use usually is contraindicated If used in combination with thiazide diuretics, usual initial dosage of lithium should be reduced by about 50% and the patient and serum lithium concentrations should be monitored carefully; subsequent lithium dosage should be adjusted as necessary |
|
Iodides |
Additive or synergistic hypothyroid effect; may result in hypothyroidism |
Concomitant use is not recommended; if used concomitantly, monitor closely for signs and symptoms of hypothyroidism |
|
Metronidazole |
May increase serum lithium concentrations, resulting in signs of lithium toxicity |
Use with caution; monitor serum lithium concentrations frequently |
|
Neuromuscular blocking agents (e.g., pancuronium, succinylcholine) |
May prolong the latency of neuromuscular blockade |
Use with caution and carefully monitor patients during concomitant use; consider temporary discontinuance of lithium |
|
NSAIAs (e.g., celecoxib, indomethacin, piroxicam) |
Decreased renal clearance of lithium, which may lead to increased serum or plasma lithium concentrations and lithium toxicity |
Monitor serum lithium concentrations and observe patient for signs and symptoms of lithium intoxication Adjust lithium dosages as needed |
|
Opiate agonists |
Interferes with opiate-induced euphoria and diminishes the analgesic effect of opiates (narcotic analgesics) |
|
|
Sodium |
Changes in sodium intake in patients receiving lithium may alter the renal elimination of lithium |
Patients should be advised to avoid substantial changes in their sodium intake When drugs with a high sodium content (e.g., antacids) are used concomitantly with lithium, serum lithium concentrations should be monitored |
|
Tetracycline |
Increased serum lithium concentrations |
The clinical importance of this effect has not been determined |
Lithium Pharmacokinetics
Absorption
Bioavailability
Conventional lithium carbonate capsules and tablets are 95–100% absorbed.
Extended-release lithium carbonate tablets are 60–90% absorbed.
Lithium citrate oral solutions are essentially 100% absorbed.
Onset
Acute antimanic effect usually occurs within 5–7 days; full therapeutic effect often requires 10–21 days.
Food
Food does not appear to affect the bioavailability of lithium.
Plasma Concentrations
Therapeutic serum lithium concentrations usually range from 1–1.2 mEq/L during acute affective episodes.
A 12-hour steady-state serum lithium concentration is used by most clinicians for monitoring serum concentrations; this concentration shows a high intraindividual (but not interindividual) reproducibility. (See General under Dosage and Administration.)
Distribution
Extent
Widely distributed into most body tissues and fluids, including bone, brain tissue, erythrocytes, saliva, and thyroid.
Lithium freely crosses the placenta; maternal and fetal serum concentrations are approximately equal. The milk of nursing women contains lithium concentrations that are approximately 33–50% of those in serum.
Plasma Protein Binding
Lithium is not bound to plasma proteins.
Elimination
Metabolism
Lithium is not metabolized.
Elimination Route
Principally renal.
Half-life
Approximately 24 hours.
Special Populations
In geriatric patients and patients with impaired renal function, serum half-lives of 36 and 40–50 hours, respectively, have been reported.
Clearance and distribution into erythrocytes may be increased during pregnancy. Immediately postpartum, renal clearance of lithium may decrease to pre-pregnancy levels.
Lithium is readily removed by hemodialysis but not as readily removed by peritoneal dialysis. Rebound increases in serum lithium concentration frequently occur 5–8 hours after dialysis.
Stability
Storage
Oral
Capsules, Tablets, and Extended-release Tablets
Well-closed containers at 15–30°C. Protect from moisture.
Solution
Tight containers at 15–30°C.
Actions
-
Alters sodium transport in nerve and muscle cells and effects a shift toward intraneuronal metabolism of catecholamines, but the specific biochemical mechanism of lithium action in mania is unknown.
-
Decreases renal-concentrating ability and water reabsorption and initially increases sodium and potassium excretion. Some of these effects are overcome by counteracting physiologic mechanisms, while others may persist. GFR may be slightly decreased in patients receiving prolonged lithium therapy.
-
Various effects on the thyroid gland; principal effect is to block the release of thyroxine (T4) and triiodothyronine (T3) mediated by thyrotropin. This results in a decrease in circulating T4 and T3 concentrations and a feedback increase in serum thyrotropin concentration. Lithium also inhibits thyrotropin-stimulated adenylate cyclase activity and thyrotropin-induced release of thyroidal iodine 131, decreases intrathyroidal iodothyronine-iodotyrosine ratios, and inhibits colloid droplet formation.
Advice to Patients
-
Importance of avoiding dehydration and maintaining usual sodium and fluid intake; importance of reporting polyuria and any prolonged vomiting, diarrhea, or fever to clinician.
-
Importance of immediately discontinuing lithium therapy and consulting a clinician if signs of lithium intoxication (e.g., muscle twitching, tremor, mild ataxia, drowsiness, muscle weakness, diarrhea, vomiting) occur.
-
Importance of advising patients that lithium may impair their ability to perform activities requiring mental alertness or physical coordination (e.g., operating machinery, driving a motor vehicle).
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
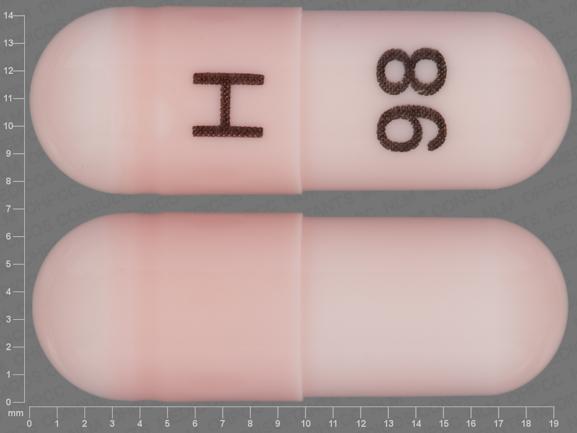
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
150 mg (4.06 mEq of lithium) |
Lithium Carbonate Capsules |
Roxane |
|
300 mg (8.12 mEq of lithium)* |
Eskalith (with benzyl alcohol and povidone) |
GlaxoSmithKline |
||
|
600 mg (16.24 mEq of lithium) |
Lithium Carbonate Capsules |
Roxane |
||
|
Tablets |
300 mg (8.12 mEq of lithium) |
Lithium Carbonate Tablets (with povidone; scored) |
Roxane |
|
|
Tablets, extended-release |
450 mg (12.18 mEq of lithium) |
Eskalith CR (scored) |
GlaxoSmithKline |
|
|
Tablets, extended-release, film-coated |
300 mg (8.12 mEq of lithium) |
Lithobid Slow-release (with povidone and propylene glycol) |
JDS Pharma |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
8 mEq (of lithium) per 5 mL |
Lithium Citrate Syrup (with alcohol 0.3%) |
Major |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions June 1, 2006. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
More about lithium
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (483)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: antimanic agents
- Breastfeeding
- En español
Patient resources
Professional resources
- Lithium prescribing information
- Lithium Capsules (FDA)
- Lithium Carbonate (FDA)
- Lithium Carbonate ER Tablets (FDA)
- Lithium Carbonate Tablets (FDA)