Dicloxacillin (Monograph)
Drug class: Penicillinase-resistant Penicillins
Chemical name: [2S-(2α,5α,6β)]-6-[[[3-(2,6-Dichlorophenyl)-5-methyl-4-isoxazolyl]carbonyl]amino]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylic acid monosodium salt monohydrate
CAS number: 13412-64-1
Introduction
Antibacterial; β-lactam antibiotic; isoxazolyl penicillin classified as a penicillinase-resistant penicillin.
Uses for Dicloxacillin
Staphylococcal Infections
Treatment of infections caused by, or suspected of being caused by, susceptible penicillinase-resistant staphylococci.
Should not be used for initial treatment of severe, life-threatening infections, including endocarditis, but may be used as follow-up after a parenteral penicillinase-resistant penicillin (nafcillin, oxacillin).
If used empirically, consider whether staphylococci resistant to penicillinase-resistant penicillins (oxacillin-resistant [methicillin-resistant] staphylococci) are prevalent in the hospital or community. (See Staphylococci Resistant to Penicillinase-resistant Penicillins under Cautions.)
Dicloxacillin Dosage and Administration
Administration
Oral Administration
Administer orally at least 1 hour before or 2 hours after meals.
Should not be used for initial treatment of severe infections and should not be relied on in patients with nausea, vomiting, gastric dilatation, cardiospasm, or intestinal hypermotility.
Dosage
Available as dicloxacillin sodium; dosage expressed in terms of dicloxacillin.
Duration of treatment depends on type and severity of infection and should be determined by the clinical and bacteriologic response of the patient. Usually continued for ≥48 hours after cultures are negative and patient becomes afebrile and asymptomatic. For severe staphylococcal infections, continue therapy for ≥14 days; more prolonged therapy is necessary for treatment of osteomyelitis, endocarditis, or other metastatic infections.
Pediatric Patients
Staphylococcal Infections
Mild to Moderate Infections
OralChildren weighing <40 kg: 12.5 mg/kg daily given in divided doses every 6 hours.
Children weighing ≥40 kg: 125 mg every 6 hours.
Children ≥1 month of age: AAP recommends 25–50 mg/kg daily in 4 divided doses.
More Severe Infections
OralChildren weighing <40 kg: 25 mg/kg daily given in divided doses every 6 hours; higher dosage may be necessary depending on severity of infection.
Children weighing ≥40 kg: 250 mg every 6 hours; higher dosage may be necessary depending on severity of infection.
Inappropriate for severe infections per AAP.
Acute or Chronic Osteomyelitis
Oral50–100 mg/kg daily given in divided doses every 6 hours as follow-up to initial parenteral therapy. If an oral regimen is used, compliance must be assured and some clinicians suggest that serum bactericidal titers (SBTs) be used to monitor adequacy of therapy and adjust dosage.
When used as follow-up in treatment of acute osteomyelitis, oral regimen usually given for 3–6 weeks or until total duration of parenteral and oral therapy is ≥6 weeks; when used as follow-up in treatment of chronic osteomyelitis, oral regimen usually given for ≥1–2 months and has been given for as long as 1–2 years.
Adults
Staphylococcal Infections
Mild to Moderate Infections
Oral125 mg every 6 hours.
More Severe Infections
Oral250 mg every 6 hours; higher dosage may be necessary depending on severity of infection.
Special Populations
Renal Impairment
Dosage adjustment generally unnecessary in patients with renal impairment.
Related/similar drugs
prednisone, amoxicillin, doxycycline, azithromycin, cephalexin, ciprofloxacin, metronidazole
Cautions for Dicloxacillin
Contraindications
-
Known hypersensitivity to any penicillin.
Warnings/Precautions
Sensitivity Reactions
Hypersensitivity Reactions
Serious and occasionally fatal hypersensitivity reactions, including anaphylaxis, reported with penicillins. Anaphylaxis occurs most frequently with parenteral penicillins but has occurred with oral penicillins.
Prior to initiation of therapy, make careful inquiry regarding previous hypersensitivity reactions to penicillins, cephalosporins, or other drugs. Partial cross-allergenicity occurs among penicillins and other β-lactam antibiotics including cephalosporins and cephamycins.
If a severe hypersensitivity reaction occurs, discontinue immediately and institute appropriate therapy as indicated (e.g., epinephrine, corticosteroids, maintenance of an adequate airway and oxygen).
General Precautions
Superinfection
Possible emergence and overgrowth of nonsusceptible bacteria or fungi. Discontinue and institute appropriate therapy if superinfection occurs.
Laboratory Monitoring
Periodically assess organ system functions, including renal, hepatic, and hematopoietic, during prolonged therapy.
Peform urinalysis and determine serum creatinine and BUN concentrations prior to and periodically during therapy.
To monitor for hepatotoxicity, determine AST and ALT concentrations prior to and periodically during therapy.
Because adverse hematologic effects have occurred with penicillinase-resistant penicillins, total and differential WBC counts should be performed prior to and 1–3 times weekly during therapy.
Selection and Use of Anti-infectives
To reduce development of drug-resistant bacteria and maintain effectiveness of dicloxacillin and other antibacterials, use only for treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria.
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing. In the absence of such data, consider local epidemiology and susceptibility patterns when selecting anti-infectives for empiric therapy.
Staphylococci Resistant to Penicillinase-resistant Penicillins
Consider that staphylococci resistant to penicillinase-resistant penicillins (referred to as oxacillin-resistant [methicillin-resistant] staphylococci) are being reported with increasing frequency.
If dicloxacillin used empirically for treatment of any infection suspected of being caused by staphylococci, the drug should be discontinued and appropriate anti-infective therapy substituted if the infection is found to be caused by any organism other than penicillinase-producing staphylococci susceptible to penicillinase-resistant penicillins. If staphylococci resistant to penicillinase-resistant penicillins (oxacillin-resistant staphylococci) are prevalent in the hospital or community, empiric therapy of suspected staphylococcal infections should include another appropriate anti-infective (e.g., vancomycin).
Sodium Content
Each 250-mg capsule contains approximately 0.6 mEq of sodium.
Specific Populations
Pregnancy
Category B.
Lactation
Distributed into milk. Use with caution.
Pediatric Use
Elimination of penicillins is delayed in neonates because of immature mechanisms for renal excretion; abnormally high serum concentrations may occur in this age group.
If used in neonates, monitor closely for clinical and laboratory evidence of toxic or adverse effects, determine serum concentrations frequently, and make appropriate reductions in dosage and frequency of administration when indicated.
Common Adverse Effects
GI effects (nausea, vomiting, epigastric distress, loose stools, diarrhea, flatulence); hypersensitivity reactions.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Aminoglycosides |
In vitro evidence of synergistic antibacterial effects against penicillinase-producing and nonpenicillinase-producing S. aureus |
|
|
Anticoagulants, oral (warfarin) |
Possible decreased hypothrombinemic effect |
Monitor PTs and adjust anticoagulant dosage if indicated |
|
Probenecid |
Decreased renal tubular secretion and increased and prolonged dicloxacillin plasma concentrations. |
|
|
Tetracyclines |
Possible antagonism |
Concomitant use not recommended |
Dicloxacillin Pharmacokinetics
Absorption
Bioavailability
Rapidly, but incompletely, absorbed from GI tract.
35–76% of an oral dose absorbed from GI tract; peak serum concentrations generally attained within 0.5–2 hours.
Food
Food in the GI tract generally decreases the rate and extent of absorption.
Distribution
Extent
Distributed into bone, bile, pleural fluid, ascitic fluid, and synovial fluid.
Only minimal concentrations attained in CSF.
Crosses the placenta and is distributed into milk.
Plasma Protein Binding
95–99% bound to serum proteins.
Elimination
Metabolism
Partially metabolized to active and inactive metabolites.
Approximately 10% of absorbed drug is hydrolyzed to penicilloic acids which are microbiologically inactive; also hydroxylated to a small extent to a microbiologically active metabolite which appears to be slightly less active than dicloxacillin.
Elimination Route
Dicloxacillin and its metabolites rapidly eliminated in urine mainly by tubular secretion and glomerular filtration. Also partly excreted in feces via biliary elimination.
31–65% of a dose excreted in urine as unchanged drug and active metabolites within 6–8 hours; approximately 10–20% of this is the active metabolite.
Only minimally removed by hemodialysis or peritoneal dialysis.
Half-life
Adults with normal renal function: 0.6–0.8 hours.
Children 2–16 years of age: average half-life is 1.9 hours.
Neonates: half-life is longer than in older children.
Special Populations
Patients with renal impairment: serum half-life is slightly prolonged and may range from 1–2.2 hours in those with severe renal impairment.
Patients with cystic fibrosis eliminate dicloxacillin approximately 3 times faster than healthy individuals.
Stability
Storage
Oral
Capsules
15–30°C in tight containers.
Actions and Spectrum
-
Based on spectrum of activity, classified as a penicillinase-resistant penicillin.
-
Usually bactericidal.
-
Like other β-lactam antibiotics, antibacterial activity results from inhibition of bacterial cell wall synthesis.
-
Spectrum of activity includes many gram-positive aerobic cocci, some gram-positive bacilli, and a few gram-negative aerobic cocci; generally inactive against gram-negative bacilli and anaerobic bacteria. Inactive against mycobacteria, Mycoplasma, Rickettsia, fungi, and viruses.
-
Gram-positive aerobes: active in vitro against penicillinase-producing and nonpenicillinase-producing Staphylococcus aureus and S. epidermidis, S. pyogenes (group A β-hemolytic streptococci), S. agalactiae (group B streptococci), groups C and G streptococci, S. pneumoniae, and some viridans streptococci. Enterococci (including E. faecalis) usually are resistant.
-
Like other penicillinase-resistant penicillins, dicloxacillin is resistant to inactivation by staphylococcal penicillinases and is active against many penicillinase-producing strains of S. aureus and S. epidermidis resistant to natural penicillins, aminopenicillins, or extended-spectrum penicillins.
-
Staphylococci resistant to penicillinase-resistant penicillins (referred to as oxacillin-resistant [methicillin-resistant] staphylococci) are being reported with increasing frequency. Complete cross-resistance occurs among the penicillinase-resistant penicillins (dicloxacillin, nafcillin, oxacillin).
Advice to Patients
-
Advise patients that antibacterials (including dicloxacillin) should only be used to treat bacterial infections and not used to treat viral infections (e.g., the common cold).
-
Importance of completing full course of therapy, even if feeling better after a few days.
-
Advise patients that skipping doses or not completing the full course of therapy may decrease effectiveness and increase the likelihood that bacteria will develop resistance and will not be treatable with dicloxacillin or other antibacterials in the future.
-
Importance of taking dicloxacillin 1 hour before or 2 hours after meals.
-
Importance of discontinuing dicloxacillin and notifying clinician if they develop shortness of breath, wheezing, rash, mouth irritation, black tongue, sore throat, nausea, vomiting, diarrhea, fever, swollen joints, or any unusual bleeding or bruising during dicloxacillin treatment.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Importance of women informing clinician if they are or plan to become pregnant or to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
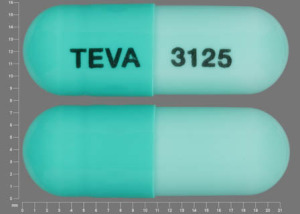
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
250 mg (of dicloxacillin)* |
Dicloxacillin Sodium |
Sandoz |
|
500 mg (of dicloxacillin)* |
Dicloxacillin Sodium |
Sandoz |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions May 1, 2004. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about dicloxacillin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (8)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: penicillinase resistant penicillins
- Breastfeeding
- En español