Warfarin Dosage
Medically reviewed by Drugs.com. Last updated on Aug 10, 2023.
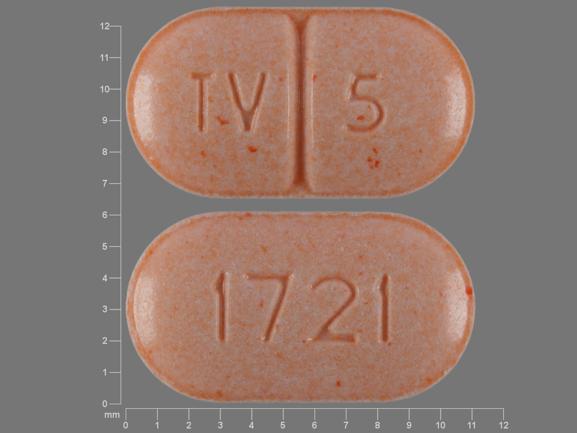
Applies to the following strengths: 4 mg; 1 mg; 2 mg; 5 mg; 7.5 mg; 10 mg; 2.5 mg; 3 mg; 6 mg
Usual Adult Dose for:
- Prevention of Thromboembolism in Atrial Fibrillation
- Thromboembolic Stroke Prophylaxis
- Myocardial Infarction
- Myocardial Infarction - Prophylaxis
- Deep Vein Thrombosis - Prophylaxis
- Pulmonary Embolism
- Deep Vein Thrombosis - First Event
- Deep Vein Thrombosis - Recurrent Event
- Pulmonary Embolism - First Event
- Pulmonary Embolism - Recurrent Event
- Prosthetic Heart Valves - Tissue Valves
- Prosthetic Heart Valves - Mechanical Valves
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Prevention of Thromboembolism in Atrial Fibrillation
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
Target INR: 2.5 (range: 2 to 3)
Duration of therapy: Indefinite
Comments:
- For patients with atrial fibrillation (AF) and prosthetic heart valves, target INR may be increased depending on valve type, valve position, and patient factors.
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Use: Prophylaxis and treatment of thromboembolic complications associated with AF.
Usual Adult Dose for Thromboembolic Stroke Prophylaxis
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
Target INR: 2.5 (range: 2 to 3)
Duration of therapy: Indefinite
Comments:
- For patients with atrial fibrillation (AF) and prosthetic heart valves, target INR may be increased depending on valve type, valve position, and patient factors.
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Use: Prophylaxis and treatment of thromboembolic complications associated with AF.
Usual Adult Dose for Myocardial Infarction
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
INR: 2 to 3
Duration of therapy: At least 3 months after myocardial infarction
Comments:
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Use: Reduction in the risk of death, recurrent myocardial infarction (MI), and thromboembolic events such as stroke or systemic embolization after myocardial infarction.
Usual Adult Dose for Myocardial Infarction - Prophylaxis
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
INR: 2 to 3
Duration of therapy: At least 3 months after myocardial infarction
Comments:
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Use: Reduction in the risk of death, recurrent myocardial infarction (MI), and thromboembolic events such as stroke or systemic embolization after myocardial infarction.
Usual Adult Dose for Deep Vein Thrombosis - Prophylaxis
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
Target INR: 2.5 (range: 2 to 3)
Duration of therapy:
- Deep venous thrombosis (DVT) or pulmonary embolism (PE) secondary to a reversible risk factor: 3 months
- Unprovoked DVT or PE: At least 3 months; evaluate risk-benefit ratio of long-term treatment after 3 months.
- Two episodes of unprovoked DVT or PE: Indefinite; periodically reassess risk-benefit ratio of continuing such treatment.
Comments:
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Use: Prophylaxis and treatment of venous thrombosis and PE.
Usual Adult Dose for Pulmonary Embolism
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
Target INR: 2.5 (range: 2 to 3)
Duration of therapy:
- Deep venous thrombosis (DVT) or pulmonary embolism (PE) secondary to a reversible risk factor: 3 months
- Unprovoked DVT or PE: At least 3 months; evaluate risk-benefit ratio of long-term treatment after 3 months.
- Two episodes of unprovoked DVT or PE: Indefinite; periodically reassess risk-benefit ratio of continuing such treatment.
Comments:
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Use: Prophylaxis and treatment of venous thrombosis and PE.
Usual Adult Dose for Deep Vein Thrombosis - First Event
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
Target INR: 2.5 (range: 2 to 3)
Duration of therapy:
- Deep venous thrombosis (DVT) or pulmonary embolism (PE) secondary to a reversible risk factor: 3 months
- Unprovoked DVT or PE: At least 3 months; evaluate risk-benefit ratio of long-term treatment after 3 months.
- Two episodes of unprovoked DVT or PE: Indefinite; periodically reassess risk-benefit ratio of continuing such treatment.
Comments:
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Use: Prophylaxis and treatment of venous thrombosis and PE.
Usual Adult Dose for Deep Vein Thrombosis - Recurrent Event
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
Target INR: 2.5 (range: 2 to 3)
Duration of therapy:
- Deep venous thrombosis (DVT) or pulmonary embolism (PE) secondary to a reversible risk factor: 3 months
- Unprovoked DVT or PE: At least 3 months; evaluate risk-benefit ratio of long-term treatment after 3 months.
- Two episodes of unprovoked DVT or PE: Indefinite; periodically reassess risk-benefit ratio of continuing such treatment.
Comments:
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Use: Prophylaxis and treatment of venous thrombosis and PE.
Usual Adult Dose for Pulmonary Embolism - First Event
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
Target INR: 2.5 (range: 2 to 3)
Duration of therapy:
- Deep venous thrombosis (DVT) or pulmonary embolism (PE) secondary to a reversible risk factor: 3 months
- Unprovoked DVT or PE: At least 3 months; evaluate risk-benefit ratio of long-term treatment after 3 months.
- Two episodes of unprovoked DVT or PE: Indefinite; periodically reassess risk-benefit ratio of continuing such treatment.
Comments:
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Use: Prophylaxis and treatment of venous thrombosis and PE.
Usual Adult Dose for Pulmonary Embolism - Recurrent Event
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
Target INR: 2.5 (range: 2 to 3)
Duration of therapy:
- Deep venous thrombosis (DVT) or pulmonary embolism (PE) secondary to a reversible risk factor: 3 months
- Unprovoked DVT or PE: At least 3 months; evaluate risk-benefit ratio of long-term treatment after 3 months.
- Two episodes of unprovoked DVT or PE: Indefinite; periodically reassess risk-benefit ratio of continuing such treatment.
Comments:
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Use: Prophylaxis and treatment of venous thrombosis and PE.
Usual Adult Dose for Prosthetic Heart Valves - Tissue Valves
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
Comments:
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Uses:
- Prophylaxis and treatment of thromboembolic complications in patients with a bileaflet mechanical valve or a Medtronic Hall (Minneapolis, MN) tilting disk valve in the aortic position who are in sinus rhythm and without left atrial enlargement (target INR: 2.5; range: 2 to 3).
- Prophylaxis and treatment of thromboembolic complications in patients with tilting disk valves and bileaflet mechanical valves in the mitral position (target INR: 3; range: 2.5 to 3.5).
- Prophylaxis and treatment of thromboembolic complications in patients with caged ball or caged disk valves (target INR: 3; range: 2.5 to 3.5).
- Prophylaxis and treatment of thromboembolic complications in patients with a bioprosthetic valve in the mitral position (target INR: 2.5; range: 2 to 3) for the first 3 months after valve insertion is recommended. If additional risk factors for thromboembolism are present (atrial fibrillation, previous thromboembolism, left ventricular dysfunction), a target INR of 2.5 (range: 2 to 3) is recommended.
Usual Adult Dose for Prosthetic Heart Valves - Mechanical Valves
Initial dose: 2 to 5 mg orally once a day
Maintenance dose: 2 to 10 mg orally once a day
Comments:
- Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors.
- Dosage and administration must be individualized according to the patient's INR and condition being treated.
Uses:
- Prophylaxis and treatment of thromboembolic complications in patients with a bileaflet mechanical valve or a Medtronic Hall (Minneapolis, MN) tilting disk valve in the aortic position who are in sinus rhythm and without left atrial enlargement (target INR: 2.5; range: 2 to 3).
- Prophylaxis and treatment of thromboembolic complications in patients with tilting disk valves and bileaflet mechanical valves in the mitral position (target INR: 3; range: 2.5 to 3.5).
- Prophylaxis and treatment of thromboembolic complications in patients with caged ball or caged disk valves (target INR: 3; range: 2.5 to 3.5).
- Prophylaxis and treatment of thromboembolic complications in patients with a bioprosthetic valve in the mitral position (target INR: 2.5; range: 2 to 3) for the first 3 months after valve insertion is recommended. If additional risk factors for thromboembolism are present (atrial fibrillation, previous thromboembolism, left ventricular dysfunction), a target INR of 2.5 (range: 2 to 3) is recommended.
Usual Pediatric Dose for Thrombotic/Thromboembolic Disorder
The American College of Chest Physicians (ACCP) provides the following dosage guidelines for antithrombotic therapy in neonates and children:
Initial dose (if baseline INR is 1 to 1.3): 0.2 mg/kg orally; subsequent dose adjustments should be made to maintain an INR between 2 and 3.
Comments:
- Infants required an average of 0.33 mg/kg to maintain an INR of 2 to 3.
- Teenagers required an average of 0.09 mg/kg to maintain an INR of 2 to 3.
Renal Dose Adjustments
No adjustment recommended
Liver Dose Adjustments
Use with caution
Dose Adjustments
The following factors may necessitate a dose reduction: weight loss, acute illness, or smoking cessation.
The following factors may necessitate a dose increase: weight gain, diarrhea, or vomiting.
Dose Adjustments for Pediatric Patients to Maintain an INR Between 2 and 3 (American College of Chest Physicians [ACCP]):
Day 1 (if baseline INR is 1 to 1.3): 0.2 mg/kg orally.
Loading days 2 to 4:
- INR 1.1 to 1.3: Repeat initial loading dose.
- INR 1.4 to 1.9: 50% of initial loading dose.
- INR 2 to 3: 50% of initial loading dose.
- INR 3.1 to 3.5: 25% of loading dose.
- INR greater than 3.5: Hold until INR is less than 3.5 and restart at 50% decreased dose.
- INR 1.1 to 1.4: Increase by 20% of dose.
- INR 1.5 to 1.9: Increase by 10% of dose.
- INR 2 to 3: No change.
- INR 3.1 to 3.5: Decrease by 10% of dose.
- INR greater than 3.5: Hold until INR is less than 3.5 and restart at 20% decreased dose.
Dosing Recommendations with Consideration of Genotype:
Genetic variations in the CYP450 2C9 and vitamin K epoxide reductase complex 1 (VKORC1) enzymes can significantly influence patient response to this drug as indicated by the prothrombin time (PT)/INR. Lower initial doses have been suggested for patients with these genetic variations due to increased risk of bleeding. Range of expected maintenance daily doses based on CYP450 2C9 and VKORC1 genotypes:
- VKORC1 GG and CYP450 2C9 *1/*1: 5 to 7 mg
- VKORC1 AG and CYP450 2C9 *1/*1: 5 to 7 mg
- VKORC1 AA and CYP450 2C9 *1/*1: 3 to 4 mg
- VKORC1 GG and CYP450 2C9 *1/*2: 5 to 7 mg
- VKORC1 AG and CYP450 2C9 *1/*2: 3 to 4 mg
- VKORC1 AA and CYP450 2C9 *1/*2: 3 to 4 mg
- VKORC1 GG and CYP450 2C9 *1/*3: 3 to 4 mg
- VKORC1 AG and CYP450 2C9 *1/*3: 3 to 4 mg
- VKORC1 AA and CYP450 2C9 *1/*3: 0.5 to 2 mg
- VKORC1 GG and CYP450 2C9 *2/*2: 3 to 4 mg
- VKORC1 AG and CYP450 2C9 *2/*2: 3 to 4 mg
- VKORC1 AA and CYP450 2C9 *2/*2: 0.5 to 2 mg
- VKORC1 GG and CYP450 2C9 *2/*3: 3 to 4 mg
- VKORC1 AG and CYP450 2C9 *2/*3: 0.5 to 2 mg
- VKORC1 AA and CYP450 2C9 *2/*3: 0.5 to 2 mg
- VKORC1 GG and CYP450 2C9 *3/*3: 0.5 to 2 mg
- VKORC1 AG and CYP450 2C9 *3/*3: 0.5 to 2 mg
- VKORC1 AA and CYP450 2C9 *3/*3: 0.5 to 2 mg
Patients with CYP450 2C9 *1/*3, *2/*2, *2/*3, and *3/*3 alleles may take up to 4 weeks to achieve maximum INR with a given dose regimen.
Conversion from Heparin and Other Anticoagulants:
Heparin:
- Conversion to this drug may begin concomitantly with heparin or may be delayed 3 to 6 days.
- Continue full-dose heparin with this drug and overlap for 4 to 5 days and until the desired therapeutic response as determined by INR has been achieved, at which point heparin may be discontinued.
Other anticoagulants:
- Consult the manufacturer product information of other anticoagulants to determine appropriate conversion to this drug.
Precautions
US BOXED WARNING:
- BLEEDING RISK: This drug can cause major or fatal bleeding. Perform regular monitoring of INR in all treated patients. Drugs, dietary changes, and other factors affect INR levels achieved with this drug. Instruct patients about prevention measures to minimize risk of bleeding and to report signs and symptoms of bleeding.
NARROW THERAPEUTIC INDEX:
- This drug should be considered a narrow therapeutic index (NTI) drug as small differences in dose or blood concentrations may lead to serious therapeutic failures or adverse drug reactions.
- Generic substitution should be done cautiously, if at all, as current bioequivalence standards are generally insufficient for NTI drugs.
- Additional and/or more frequent monitoring should be done to ensure receipt of an effective dose while avoiding unnecessary toxicities.
Safety and efficacy have not been established in patients younger than 18 years.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- Consult the latest guidelines regarding duration and intensity of anticoagulation for the indicated conditions.
- This drug should be taken at the same time each day. A missed dose should be taken as soon as possible on the same day, and not doubled the next day.
- In emergencies, initiate this drug with heparin.
- In general, anticoagulant therapy should be continued until the risk of thrombosis and embolism has passed.
Storage requirements: Protect from light.
Reconstitution/preparation techniques: Pregnant pharmacy and clinical personnel should avoid exposure to crushed or broken tablets.
General:
- This drug has no direct effect on an established thrombus, nor does it reverse ischemic tissue damage.
- Various brands of this drug may not be bioequivalent.
Monitoring:
- Hematologic: Prothrombin time (PT)/INR (the manufacturer product information and institution-specific protocol should be consulted).
- Hepatic: Liver function tests at baseline
Patient advice:
- Instruct patients about prevention measures to minimize risk of bleeding and to report signs and symptoms of bleeding.
- Advise patients to eat a balanced diet with a consistent amount of vitamin K and to avoid drastic changes in dietary habits, such as eating large amounts of green leafy vegetables.
- Inform patients to contact their healthcare provider immediately if they notice possible signs of skin necrosis/gangrene or small cholesterol emboli, such as pain or color/temperature change in any part of the body.
- Instruct patients to inform their doctor before they start any additional medications, including over-the-counter products, herbal remedies, and supplements.
- Advise females of reproductive potential to use effective contraception during treatment and for at least 1 month after the final dose.
- Advise patients to contact their doctor immediately if they think they are pregnant, to discuss pregnancy planning, and if they are considering breastfeeding.
Frequently asked questions
- What is the antidote for warfarin?
- Is warfarin used as rat poison?
- Does Feverfew interact with any drugs?
- Why does warfarin cause purple toe syndrome?
- Does cranberry juice help prevent a UTI?
- Why are Warfarin tablets color-coded?
- Is your blood really thinner with warfarin?
More about warfarin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (56)
- Drug images
- Side effects
- Patient tips
- During pregnancy
- Support group
- Drug class: coumarins and indandiones
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.