Rifadin Disease Interactions
There are 6 disease interactions with Rifadin (rifampin).
Antibiotics (applies to Rifadin) colitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Colitis/Enteritis (Noninfectious)
Clostridioides difficile-associated diarrhea (CDAD), formerly pseudomembranous colitis, has been reported with almost all antibacterial drugs and may range from mild diarrhea to fatal colitis. The most common culprits include clindamycin and lincomycin. Antibacterial therapy alters the normal flora of the colon, leading to overgrowth of C difficile, whose toxins A and B contribute to CDAD development. Morbidity and mortality are increased with hypertoxin-producing strains of C difficile; these infections can be resistant to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea after antibacterial use. Since CDAD has been reported to occur more than 2 months after antibacterial use, careful medical history is necessary. Therapy with broad-spectrum antibacterials and other agents with significant antibacterial activity should be administered cautiously in patients with history of gastrointestinal disease, particularly colitis; pseudomembranous colitis (generally characterized by severe, persistent diarrhea and severe abdominal cramps, and sometimes associated with the passage of blood and mucus), if it occurs, may be more severe in these patients and may be associated with flares in underlying disease activity. Antibacterial drugs not directed against C difficile may need to be stopped if CDAD is suspected or confirmed. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C difficile, and surgical evaluation should be started as clinically indicated.
References
- "Product Information. Omnipen (ampicillin)." Wyeth-Ayerst Laboratories PROD (2002):
- "Product Information. Ceftin (cefuroxime)." Glaxo Wellcome PROD (2002):
- "Product Information. Zinacef (cefuroxime)." Glaxo Wellcome PROD (2002):
- "Product Information. Cleocin (clindamycin)." Pharmacia and Upjohn PROD (2002):
- "Product Information. Macrobid (nitrofurantoin)." Procter and Gamble Pharmaceuticals PROD (2002):
- "Product Information. Macrodantin (nitrofurantoin)." Procter and Gamble Pharmaceuticals PROD (2002):
- "Product Information. Amoxil (amoxicillin)." SmithKline Beecham PROD (2001):
- "Product Information. Merrem (meropenem)." Astra-Zeneca Pharmaceuticals PROD (2001):
- "Product Information. Coly-Mycin M Parenteral (colistimethate)." Parke-Davis PROD (2001):
- "Product Information. Lincocin (lincomycin)." Pharmacia and Upjohn PROD (2001):
- "Product Information. Cubicin (daptomycin)." Cubist Pharmaceuticals Inc (2003):
- "Product Information. Xifaxan (rifaximin)." Salix Pharmaceuticals (2004):
- "Product Information. Doribax (doripenem)." Ortho McNeil Pharmaceutical (2007):
- "Product Information. Penicillin G Procaine (procaine penicillin)." Monarch Pharmaceuticals Inc (2009):
- "Product Information. Vibativ (telavancin)." Theravance Inc (2009):
- "Product Information. Teflaro (ceftaroline)." Forest Pharmaceuticals (2010):
- "Product Information. Penicillin G Sodium (penicillin G sodium)." Sandoz Inc (2022):
- "Product Information. Dalvance (dalbavancin)." Durata Therapeutics, Inc. (2014):
- "Product Information. Orbactiv (oritavancin)." The Medicines Company (2014):
- "Product Information. Bicillin C-R (benzathine penicillin-procaine penicillin)." A-S Medication Solutions (2017):
- "Product Information. Baxdela (delafloxacin)." Melinta Therapeutics, Inc. (2017):
- "Product Information. Polymyxin B Sulfate (polymyxin B sulfate)." AuroMedics Pharma LLC (2022):
- "Product Information. Zemdri (plazomicin)." Achaogen (2018):
- "Product Information. Seysara (sarecycline)." Allergan Inc (2018):
- "Product Information. Nuzyra (omadacycline)." Paratek Pharmaceuticals, Inc. (2018):
- "Product Information. Aemcolo (rifamycin)." Aries Pharmaceuticals, Inc. (2018):
- "Product Information. Fetroja (cefiderocol)." Shionogi USA Inc (2019):
- "Product Information. Biaxin (clarithromycin)." AbbVie US LLC SUPPL-61 (2019):
- "Product Information. Zithromax (azithromycin)." Pfizer U.S. Pharmaceuticals Group LAB-0372-7.0 (2021):
- "Product Information. E.E.S.-400 Filmtab (erythromycin)." Arbor Pharmaceuticals SUPPL-74 (2018):
- "Product Information. Priftin (rifapentine)." sanofi-aventis SUPPL-18 (2020):
- "Product Information. Xerava (eravacycline)." Tetraphase Pharmaceuticals, Inc (2021):
- "Product Information. Xacduro (durlobactam-sulbactam)." La Jolla Pharmaceutical ORIG-1 (2023):
- "Product Information. Exblifep (cefepime-enmetazobactam)." Allecra Therapeutics ORIG-1 (2024):
- "Product Information. Maxipime (cefepime)." Hospira Inc SUPPL-46 (2021):
Rifampin (applies to Rifadin) hematopoietic disturbances
Major Potential Hazard, Low plausibility. Applicable conditions: Bone Marrow Depression/Low Blood Counts
Rifampin may infrequently cause hematopoietic abnormalities such as thrombocytopenia, leukopenia, decreased hemoglobin, and acute hemolytic anemia. Hemolysis has been described as part of an immune-mediated reaction which generally occurs after gaps in therapy. Thrombocytopenia is observed most frequently in patients receiving high-dose intermittent therapy or after a lapse in therapy, but very rarely during daily administration. It is reversible if rifampin is discontinued as soon as purpura appears. Patients with preexisting bone marrow depression or blood dyscrasias should be monitored closely during rifampin therapy for further decreases in blood counts. Although rifampin-related hematologic effects are often transient, cerebral hemorrhage and fatalities have been reported with the continued administration of rifampin after the appearance of purpura.
References
- Allen RJ, Almond SN, Caiolsa SM, et al. "Rifampin." Drug Intell Clin Pharm 5 (1971): 364-5
- Ferguson GC "Rifampicin and thrombocytopenia." Br Med J 3 (1971): 638
- Mariette X, Mitjavila MT, Moulinie JP, et al. "Rifampicin-induced pure red cell aplasia." Am J Med 87 (1989): 459-60
- Dutt AK, Moers D, Stead WW "Undesirable side effects of isoniazid and rifampin in largely twice-weekly short-course chemotherapy for tuberculosis." Am Rev Respir Dis 128 (1983): 419-24
- Lee M, Berger HW "Eosinophilia caused by rifampin." Chest 77 (1980): 579
- Lee CH, Lee CJ "Thrombocytopenia: a rare but potentially serious side effect of initial daily and interrupted use of rifampicin." Chest 96 (1989): 202-3
- Hadfield JW "Rifampicin-induced thrombocytopenia." Postgrad Med J 56 (1980): 59-60
- Tahan SR, Diamond JR, Blank JM, Horan RF "Acute hemolysis and renal failure with rifampicin-dependent antibodies after discontinuous administration." Transfusion 25 (1985): 124-7
- Nolan RL, Cleary JD, Chapman SW "Fever associated with daily rifampin therapy." Clin Pharm 9 (1990): 57-8
- Levine M, Collin K, Kassen BO "Acute hemolysis and renal failure following discontinuous use of rifampin." DICP 25 (1991): 743-4
- Brook G, Pain A "Major adverse reactions to a short course of daily rifampicin." Scand J Infect Dis 19 (1987): 271-2
- van Assendelft AH "Renal failure and haemolysis caused by rifampicin." Tubercle 67 (1986): 234-5
- "Product Information. Rifadin (rifampin)." Hoechst Marion Roussel PROD (2001):
- Hall AP, Thorpe JW, Seaton D "New hazard of meningococcal chemoprophylaxis." J Antimicrob Chemother 31 (1993): 451
- Kindelan JM, Serrano I, Jurado R, Villanueva JL, Garcialazaro M, Garciaherola A, Cisneros JT "Rifampin-induced severe thrombocytopenia in a patient with pulmonary tuberculosis." Ann Pharmacother 28 (1994): 1304-5
Rifampin (applies to Rifadin) hepatotoxicity
Major Potential Hazard, High plausibility. Applicable conditions: Liver Disease, Alcoholism
The use of rifampin has been associated with hepatocellular injury and liver dysfunction. Hepatitis and jaundice resulting in death have occurred, mostly in patients with underlying liver disease and during coadministration with other hepatotoxic agents including other antituberculous drugs such as isoniazid and pyrazinamide. Therapy with rifampin should be administered cautiously and under strict medical supervision in patients with liver disease or a history of alcoholism. Serum transaminases (ALT, AST) and bilirubin should be measured at baseline and every 2 to 4 weeks during therapy, but keeping in mind that elevated levels may occur transiently in 10% to 15% of patients, usually during the early days of treatment. Patients should be instructed to discontinue the drug promptly and seek medical attention if signs and symptoms of hepatic injury develop, including fever, rash, anorexia, nausea, vomiting, fatigue, right upper quadrant pain, dark urine, and jaundice.
References
- Allen RJ, Almond SN, Caiolsa SM, et al. "Rifampin." Drug Intell Clin Pharm 5 (1971): 364-5
- Gabriel R "Rifampin jaundice." Br Med J 3 (1971): 182
- Dutt AK, Moers D, Stead WW "Short-course chemotherapy for tuberculosis with mainly twice-weekly isoniazid and rifampin: community physicians' seven-year experience with mainly outpatients." Am J Med 77 (1984): 233-42
- O'Brien RJ, Long MW, Cross FS, et al. "Hepatotoxicity from isoniazid and rifampin among children treated for tuberculosis." Pediatrics 72 (1983): 491-9
- Dutt AK, Moers D, Stead WW "Undesirable side effects of isoniazid and rifampin in largely twice-weekly short-course chemotherapy for tuberculosis." Am Rev Respir Dis 128 (1983): 419-24
- Bartelink AK, Lenders JW, van Herwaarden CL, et al. "Fatal hepatitis after treatment with isoniazid and rifampicin in a patient on anticonvulsant therapy." Tubercle 64 (1983): 125-8
- Maddrey WC "Drug-related acute and chronic hepatitis." Clin Gastroenterol 9 (1980): 213-24
- Yoshikawa TT, Nagami PH "Adverse drug reactions in TB therapy: risks and recommendations." Geriatrics 37 (1982): 61-8
- "Product Information. Rifadin (rifampin)." Hoechst Marion Roussel PROD (2001):
- CDC. Centers for Disease Control. "Update: fatal and severe liver injuries associated with rifampin and pyrazinamide for latent tuberculosis infection, and revisions in American Thoracic Society/CDC recommendations--United States, 2001." Morb Mortal Wkly Rep 50 (2001): 733-5
Rifampin (applies to Rifadin) liver disease
Major Potential Hazard, High plausibility.
Rifampin is primarily metabolized by the liver. Patients with liver disease may be at greater risk for adverse effects from rifampin due to decreased drug clearance. In addition, the accumulation of rifampin may result in hyperbilirubinemia because rifampin competes with bilirubin for uptake by hepatocytes. Dosage adjustments are recommended in patients with liver disease. Withdrawal of rifampin therapy may be required if serum bilirubin is persistently high.
References
- Nitti V, Virgilio R, Patricolo MR, Iuliano A "Pharmacokinetic study of intravenous rifampicin." Chemotherapy 23 (1977): 1-6
- Acocella G "Clinical pharmacokinetics of rifampicin." Clin Pharmacokinet 3 (1978): 108-27
- Loos U, Musch E, Jensen JC, et al. "Pharmacokinetics of oral and intravenous rifampicin during chronic administration." Klin Wochenschr 63 (1985): 1205-11
- "Product Information. Rifadin (rifampin)." Hoechst Marion Roussel PROD (2001):
Rifampin (applies to Rifadin) porphyria
Major Potential Hazard, Moderate plausibility.
Rifampin may induce the activity of delta amino levulinic acid synthetase, an enzyme involved in the biosynthesis of porphyrins. The use of rifampin has been associated with isolated cases of porphyria exacerbation. Therapy with rifampin should be administered cautiously in patients with a history of porphyria.
References
- "Product Information. Rifadin (rifampin)." Hoechst Marion Roussel PROD (2001):
Rifampin (applies to Rifadin) enzyme induction
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Hyperthyroidism, Hyperadrenocorticism, Hypoparathyroidism, Hypothyroidism, Panhypopituitarism, Hyperparathyroidism, Adrenal Insufficiency
Rifampin has enzyme-inducing effects that can enhance the metabolism of many endogenous substrates, including adrenal hormones, thyroid hormones, and vitamin D, the latter of which may affect serum calcium, phosphate and parathyroid hormone levels. Patients with preexisting imbalances of these hormones should be monitored more closely during long-term therapy with rifampin. In patients whose hormonal condition is stabilized on treatment, adjustments may be necessary in their treatment regimen to compensate for these effects.
References
- "Product Information. Rifadin (rifampin)." Hoechst Marion Roussel PROD (2001):
Rifadin drug interactions
There are 721 drug interactions with Rifadin (rifampin).
Rifadin alcohol/food interactions
There is 1 alcohol/food interaction with Rifadin (rifampin).
More about Rifadin (rifampin)
- Rifadin consumer information
- Check interactions
- Compare alternatives
- Reviews (1)
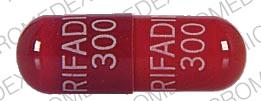
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Generic availability
- Drug class: rifamycin derivatives
- Breastfeeding
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.