Tympanoplasty
Medically reviewed by Drugs.com. Last updated on Apr 2, 2024.
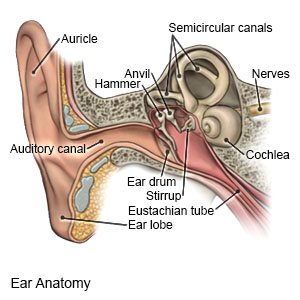
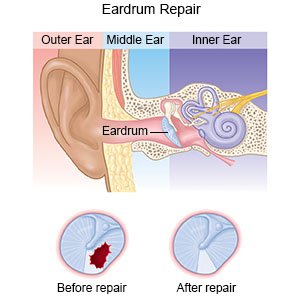
Tympanoplasty is surgery to fix a torn eardrum. Your eardrum is a tissue found in the middle part of your ear. Your eardrum divides your outer ear canal from your inner ear.
 |
WHILE YOU ARE HERE:
Before your surgery:
- Informed consent is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
- An IV is a small tube placed in your vein that is used to give you medicine or liquids.
- General anesthesia will keep you asleep and free from pain during surgery. Anesthesia may be given through your IV. You may instead breathe it in through a mask or a tube placed down your throat. The tube may cause you to have a sore throat when you wake up.
During your surgery:
- Your surgeon will make an incision behind your ear or inside your ear canal. Any infection, damage, or disease inside your ear will be cleaned out. The edges of your torn eardrum will be trimmed, or your entire eardrum may be removed.
- A graft will be used to close your torn eardrum or to replace your eardrum. A tissue graft may be taken from another part of your body. Your surgeon may place a medical sponge on one or both sides of the graft to hold it in place. Antibiotic foam may also be placed in your ear canal to help prevent infection. Your incision will be closed with stitches.
 |
After your surgery:
You will be taken to a room to rest until you are fully awake. You will be monitored closely for any problems. Do not get out of bed until your healthcare provider says it is okay. You will be able to go home or be taken to your hospital room.
- Gauze will stay in your ear for up to 1 week. You may also have a bandage covering the outside of your ear.
- Medicine may be given to decrease pain, swelling, and dizziness. You may need medicine to prevent an infection caused by bacteria.
RISKS:
You may bleed more than expected or get an infection. Nerves that control your face muscles or sense of taste may be damaged. The small bones in your ear may be damaged. You may become dizzy. The tear in your eardrum may not heal completely. You may develop bands of scar tissue in your inner ear or narrowing of your ear canal. You may have hearing loss. Your eardrum may swell or you may have drainage. Your graft may fail or you may develop another tear in your eardrum.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
