Pneumonitis
Medically reviewed by Drugs.com. Last updated on Apr 2, 2024.
Pneumonitis is inflammation of your lungs. The inflammation can make it hard to breathe and prevent you from getting enough oxygen. Anything that irritates your lung tissues can lead to pneumonitis. The longer you are exposed, the more damage your lungs will develop. Pneumonitis can last a short time or become chronic.
 |
DISCHARGE INSTRUCTIONS:
Seek care immediately if:
- You have trouble breathing.
- You faint or cannot think clearly.
- You cough up blood.
- Your lips or fingernails turn blue or gray.
- Your lips, tongue, or throat swell and you have trouble breathing or swallowing.
Call your doctor or pulmonologist if:
- You have a fever that lasts more than 3 days, even with treatment.
- Your chest pain or breathing problems do not go away or get worse.
- Your cough does not get better with treatment.
- You vomit or have diarrhea.
- You have questions or concerns about your condition or care.
Medicines:
- Medicines may help decrease coughing and inflammation, open airways, and make it easier for you to breathe. You may also need medicine to treat a bacterial infection.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Manage pneumonitis:
- Rest as directed. Keep the head of your bed raised to help you breathe easier. You can also raise your head and shoulders up on pillows or rest in a reclining chair.
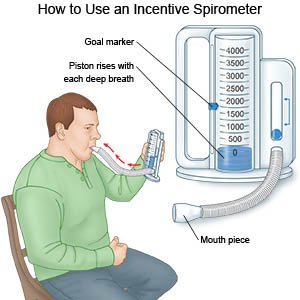
- Do deep breathing and coughing. Deep breaths help open your airway and clear mucus or congestion. Take a deep breath and hold it for as long as you can. Let the air out and then cough strongly. You may be given an incentive spirometer to help you take deep breaths. Put the plastic piece in your mouth. Take a slow, deep breath. Then let the air out and cough. Repeat these steps as directed by your healthcare provider.
- Do not smoke. Avoid secondhand smoke. Nicotine and other chemicals in cigarettes and cigars can make it harder for your lung inflammation to get better. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Get the flu vaccine. The flu can become serious in anyone who has a lung condition. Get the flu vaccine as soon as recommended each year, usually in September or October. You may also need the pneumococcal vaccine to prevent pneumonia.
- Do not drink alcohol when you are sick. Alcohol dulls your urge to cough and sneeze. Alcohol also causes your body to lose fluid. This can make the mucus in your lungs thicker and harder to cough up.
- Drink more liquids. Liquids help keep your air passages moist and better able to get rid of germs and other irritants. Ask your healthcare provider how much liquid to drink each day and which liquids are best for you.
- Use a cool mist humidifier. A humidifier will help increase air moisture in your home. This may make it easier for you to breathe and help decrease your cough.
- Go to pulmonary rehabilitation (rehab) as directed. Your healthcare provider may recommend rehab if you develop chronic pneumonitis. A rehab therapist can teach you breathing exercises to help keep your airway open.
Prevent pneumonitis:
- Avoid anything that irritates your lungs. Examples include smoke, dust, and fumes. You may need to wear a mask if you work with something that irritates your lungs.
- Be careful with household cleaners. Do not combine products that contain bleach and chlorine. Do not use these chemicals in closed spaces. Open a window or door to keep the air flowing.
Follow up with your doctor or pulmonologist as directed:
You may need to return for more tests. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Pneumonitis
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
