Aortic Valve Replacement
Medically reviewed by Drugs.com. Last updated on Apr 2, 2024.
What do I need to know about aortic valve replacement?
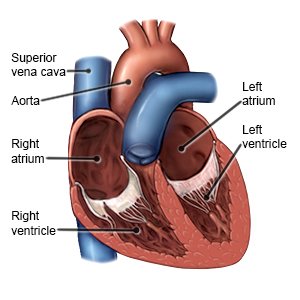
Aortic valve replacement is surgery to put a new aortic valve in your heart. Your aortic valve separates the lower section of your heart from your aorta. The aorta is the large blood vessel that carries blood from your heart to your body. Your aortic valve opens and closes to let blood flow from your heart. When the valve does not work correctly, your heart pumps less blood to your body.
 |
How do I prepare for surgery?
- Your surgeon will tell you how to prepare. Arrange to have someone drive you home after surgery. You may be told not to eat or drink anything after midnight on the day of surgery.
- Tell your surgeon about all medicines you currently take. He or she will tell you if you need to stop any medicine for surgery, and when to stop. He or she will tell you which medicines to take or not take on the day of surgery.
- Vasodilator medicine may be given to widen blood vessels in your heart allow blood to flow more easily. You may also be given blood thinning medicine to prevent blood clots. This medicine makes it easier for you to bruise and bleed. If you have a bleeding disorder or a history of bleeding or blood clots, tell your healthcare provider.
- You may need to see a dentist to make sure you do not have an infection that can increase your risk of problems after valve surgery.
- You will need blood tests. You may also need a transesophageal echocardiogram (TEE). A TEE is a moving ultrasound. TEE pictures will show the size and shape of your heart, and how it moves when it is beating. You may also need a TEE to check for certain problems, such as blood clots or infection inside the heart.
What will happen during surgery?
- You will be given general anesthesia medicine to keep you asleep and free from pain during surgery. One or more incisions will be made in your chest. Your surgeon will connect your heart to a heart-lung bypass machine. This machine does the work of your heart and lungs while healthcare providers work on your valve.
- Your aortic valve will be removed and replaced with a tissue valve or mechanical valve. The new valve will be sewn in place. Wires may be put into your chest to improve your heartbeat after surgery. The heart-lung bypass machine will be removed, and your own heart and lungs will start working again. The incision in your chest will be closed with wire and stitches.
What should I expect after surgery?
- You will be taken to the recovery room or an intensive care unit (ICU). Healthcare providers will watch you very closely. Your family may be allowed to visit you in the ICU for a short visit several times a day.
- You may need extra oxygen. The oxygen may be given through a plastic mask over your mouth and nose. Oxygen may also be given through nasal prongs (short, thin tubes in your nose).
- A chest tube may be used. A chest tube removes air, blood, or fluid from around your lungs or heart.
- Do deep breathing to open your airway. Slowly take a deep breath and hold the breath as long as you can. Then let out your breath. Take 10 deep breaths in a row every hour while you are awake. You may be asked to use an incentive spirometer to help you with this. Put the plastic piece into your mouth and slowly take a breath as deep and as long as you can. Hold your breath as long as you can. Then let your breath out.
- Intake and output may be measured. Healthcare providers will keep track of the amount of liquid you are getting. They also may need to know how much you are urinating. Ask healthcare providers if they need to measure or collect your urine.
- Prevent blood clots. Physical activity helps prevent blood clots. Healthcare providers will help you be as active as possible after your surgery.
- Medicines may be given to relieve pain or lower your blood pressure. You may need blood thinning or antiplatelet medicine to prevent blood clots. Antibiotics are given to prevent or treat an infection caused by bacteria. Heart medicine may be needed to help strengthen or regulate your heartbeat.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What are the risks of aortic valve replacement?
You may bleed more than expected during or after surgery. You may need a blood transfusion or more surgery. After your surgery, you may get an infection or have a stroke. Your new valve may not work, or over time the new valve or area around it may become damaged. The new valve may be too small and worsen your condition. The problem you had before the surgery may come back or may still be there after surgery. You may need to have heart valve surgery again. Your heart may not beat as it should after surgery. You may develop a blood clot. The blood clot can break loose and travel to your lungs. This problem can be life-threatening. You may need to take medicine to prevent blood clots for the rest of your life after your surgery.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Aortic Valve Replacement
Treatment options
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
